Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 6 - Nov. / Dec. of 2009
Vol. 42 nº 6 - Nov. / Dec. of 2009
|
ORIGINAL ARTICLE
|
|
Manifestations of infection by the novel influenza A (H1N1) virus at chest computed tomography |
|
|
Autho(rs): Carlos Gustavo Yuji Verrastro, Luiz de Abreu Junior, Diego Ziotti Hitomi, Emerson Pelarigo Antonio, Rodrigo Azambuja Neves, Giuseppe D'Ippolito |
|
|
Keywords: Influenza A virus, Influenza A (H1N1) virus subtype, Viral pneumonia, X-ray computed tomography |
|
|
Abstract:
IFellow PhD degree, Department of Diagnostic Imaging - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), MD, Radiologist, Unit of Diagnostic Imaging - Hospital e Maternidade São Luiz, São Paulo, SP, Brazil
INTRODUCTION Early in 2009, the world saw the outbreak of a novel epidemic of acute febrile respiratory disease caused by one of the categories of influenza virus, with the first cases reported in the USA and Mexico(1-4), rapidly spreading throughout other countries with inter-human dissemination, achieving pandemic levels(5). In Brazil, the first cases were confirmed in May this year. The influenza virus is classified into A, B and C types and also subdivided according to their HA (hemagglutinin) 1, 2 and 3 and NA (neuraminidase) 1 and 2 constituents. The agent responsible for the current epidemic has been classified as A (H1N1)(6-8). The clinical manifestations of infection by the influenza A (H1N1) virus are similar to the ones of the common flu such as fever, cough, myalgia, fatigue, headache, rhinorrhea, emesis and diarrhea(9). In most of cases, the condition is self-limited, requiring only clinical support measures and general care(10). However, there are some clinical features, groups and risk factors where the infection by influenza virus may be highly severe, progressing with exuberant respiratory symptoms, probably requiring specific viral therapy on an inpatient basis, with mechanical ventilation, and even so with possibility of progressing to respiratory failure and death(11). The risk groups include children under two years and elderly above 60 years of age, pregnant women, immunosuppressed individuals (transplant, cancer, AIDS patients, or immunosuppressing drugs users) and individuals with chronic comorbidities (hemoglobinopathies, cardiopathies, pneumopathies, chronic renal diseases, metabolic diseases and morbid obesity)(12). The laboratory diagnosis can be confirmed by means of viral culture or real time polymerase chain reaction (RT-PCR) of material obtained through nasopharyngeal and oropharyngeal aspirate or swab(6,13,14). In August 2009, Brazil already figured as one of the countries with highest absolute number of deaths(15), and governmental and institutional protocols were created to meet the high demand generated by suspicious cases and guiding the medical conduct(12). Despite the presence of a frustrating and self-limitating clinical situation, some patients progress with severe infection and pulmonary failure, requiring diagnostic studies such as computed tomography (CT) to establish the pulmonary involvement extent. The present study was aimed at describing main tomographic findings observed in confirmed cases of infection by the influenza A (H1N1) virus.
MATERIALS AND METHODS The authors developed a retrospective, observational, cross-sectional study to evaluate chest CT findings in patients with proved infection by the influenza A (H1N1) virus. The sample of the present study included patients assisted in four different hospitals in the period from July to August 2009. The following inclusion criteria were adopted: a) laboratory evidence of infection by the novel influenza A (H1N1) virus either by means of viral culture or RTPCR; b) complete chest CT studies performed as part of the diagnostic investigation during the acute phase of the disease. Nine patients in total have met the inclusion criteria. The age range of the patients included in the present study ranged from 14 to 64 years (mean, 40 years), and five were men and four women. Four of these patients were previously healthy, four were kidney transplant recipients and one was pregnant at approximately the 33th gestational week at the time of the diagnosis. Besides the initial CT study, the pregnant patient was also submitted to follow-up CT because of the deterioration of her clinical status seven days after the first CT study. Previously to the acute respiratory symptoms onset, the kidney transplant recipients presented stable clinical status. The CT scans were performed in multidetector Toshiba Aquilion 16 (Toshiba; Tokyo, Japan), GE LightSpeed VCT 32 (General Electric Medical Systems; Milwaukee, USA), and Philips Brilliance 16 (Philips Medical Systems; Cleveland, USA) equipments with 1.0 mm-thick sections at 1.0 mm intervals, without contrast-enhancement. The images were consensually interpreted by three radiologists, one of them with < two-year experience and two with > five-year experience in chest radiology, who assessed the presence, frequency, extent and distribution of the following findings: a) ground-glass opacity; b) consolidation; c) nodules; d) interlobular septa thickening; e) lymph node enlargement; f) pleural effusion.
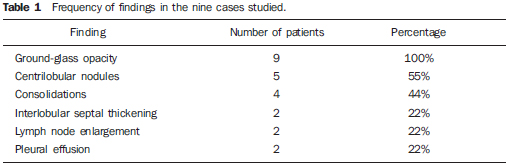
RESULTS Among the findings approached, ground-glass opacity was the most frequently found (Table 1), present in all of the cases evaluated. In two patients, sole, subtle and limited ground-glass opacity was observed. In the other seven patients, multiple, bilateral extensive areas of ground-glass opacity were observed, with no predilection for upper, middle or lower pulmonary zones, or clear central or peripheral predominance. The authors observed a lobular pattern of ground-glass opacity in four of the nine cases evaluated (Figure 1).
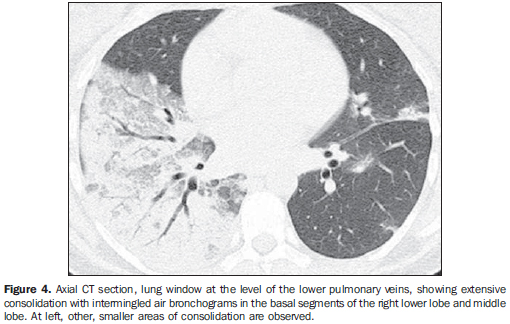
Centrilobular nodules measuring between 0.3 and 0.8 mm represented the second most frequent finding, present in five patients. In one of such cases, the centrilobular nodules presented a coalescent appearance and tree-in-bud pattern (Figure 2). In the other four patients, predominance of ill-defined ground-glass centrilobular nodules was observed (Figure 3). Consolidation was found in four cases, three of them with extensive areas of lobar consolidation and with air bronchograms (Figure 4). Areas of consolidation predominated in the middle/lower pulmonary zones, involving the lower lobes in all of the cases and the middle lobe in one patient. The pregnant patient was among these cases, presenting worsening in consolidations at the follow-up CT, with bilateral involvement and predominance in the gravity-dependent portions of the lungs (Figure 5).
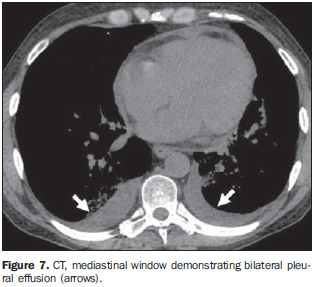
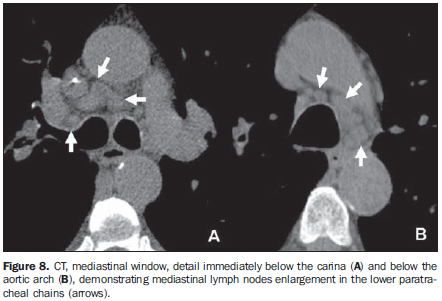
Interlobular septal thickening was present in two cases. In these two patients, the septal thickening was smooth, with no architectural distortion and preferential distribution. In one of the cases, the septal thickening overlapped areas of ground-glass opacity, corresponding to the crazy paving appearance (Figure 6). Free pleural effusions with small and mild volumes were observed in two cases (Figure 7), and mediastinal lymph node enlargement in other two cases, with up to 1.5 cm in diameter in their short axis (Figure 8).
DISCUSSION A high number of different viral agents may cause respiratory tract infections. Influenza virus, Hantavirus, Epstein-Barr virus, adenovirus in immunocompetent patients, and herpes simplex virus, varicella-zoster virus, cytomegalovirus, adenovirus, respiratory syncytial virus and parainfluenza virus in immunocompromised hosts (16,17). Viral infections may present as tracheobronchitis, bronchiolitis or pneumonia, whose radiological manifestations include: bronchiectasis, hyperinsuflation and air trapping, small ill-defined nodules, ground-glass opacities and areas of consolidation(16). Usually, infection by the influenza virus involves the trachea and main bronchi, although some patients may develop severe pneumonias. In such cases, it is frequent to find bilateral, focal or diffuse areas of ground-glass opacity associated with consolidation that may rapidly become confluent, as well as centrilobular nodules(16,18-21). Although rare, other findings such as interlobular septal thickening, pleural effusion, mediastinal lymph nodes enlargement, pneumatocele and fibrosis have already been described(18,19). In the present study, the authors evaluated chest CT findings in nine patients with proven infection by the influenza A (H1N1) virus in a pandemic moment. Despite the high number of confirmed cases worldwide, most of the patients present subtle symptoms and the investigation by means of imaging methods is restricted to radiographic studies. Additionally, the infectious-contagious nature of the approached disease tends to restrict the mobilization of these patients because of the respiratory isolation, even in the most severe cases(6). For these reasons, few cases have been available for study, hindering the drawing of conclusions on typical patterns of tomographic findings in infections by the influenza A (H1N1) virus. However, even with the limitations of the present study, the authors could observe a tendency for presentation of findings similar to the ones of the other viral pneumonias, particularly the other types of influenza such as the A (H5N1) subtype responsible for the avian flu. In such cases, the findings most frequently described were ground-glass opacity, centrilobular nodules and consolidation(16,18-20). Pleural effusion and mediastinal lymph nodes enlargement are rarely seen(18,20,22), these findings being similar to the ones observed in the present study. Among the nine patients included in the present study, five presented characteristics that included them in the risk group for developing severe disease (one pregnant woman and four recipients of kidney transplant), and these cases were precisely the ones with the most extensive tomographic findings. Among the recipients of kidney transplant, the authors observed one case where the predominant finding was centrilobular nodules with tree-in-bud pattern (Figure 2), a finding already previously described in cases of influenza pneumonias in immunocompromised patients(19). Also in the group of recipients of kidney transplant, the authors observed patients who progressed with pleural effusion and mediastinal lymph node enlargement, findings that are less frequent in viral infections in immunocompetent hosts. This is one of the first studies approaching tomographic findings in patients with infection by influenza A (H1N1) virus.
CONCLUSION Ground-glass opacity, centrilobular nodules and consolidation were the most common findings at chest CT of patients with infection by the novel influenza A (H1N1) virus. Such patterns are not typical of this specific etiological agent, and also may be found in other viral and bacterial pneumonias. In immunocompromised patients, the spectrum of findings is even wider, presenting centrilobular nodules with tree-in-bud pattern, besides pleural effusion and mediastinal lymph nodes enlargement. Despite their nonspecificity, it is important that the radiologist recognizes the main tomographic findings in patients infected by the influenza A (H1N1) virus, contributing in the follow-up of the disease progression.
REFERENCES 1. Perez-Padilla R, de la Rosa-Zamboni D, Ponce de Leon S, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680-9. [ ] 2. Centers for Disease Control and Prevention (CDC). Swine influenza A (H1N1) infection in two children - Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009; 58:400-2. [ ] 3. Zimmer SM, Burke DS. Historical perspective - emergence of influenza A (H1N1) viruses. N Engl J Med. 2009;361:279-85. [ ] 4. Brownstein JS, Freifeld CC, Madoff LC. Influenza A (H1N1) virus, 2009 - online monitoring. N Engl J Med. 2009;360:2156. [ ] 5. Zarocostas J. World Health Organization declares A (H1N1) influenza pandemic. BMJ. 2009;338:b2425. [ ] 6. Galwankar S, Clem A. Swine influenza A (H1N1) strikes a potential for global disaster. J Emerg Trauma Shock. 2009;2:99-105. [ ] 7. Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605-15. [ ] 8. Gatherer D. The 2009 H1N1 influenza outbreak in its historical context. J Clin Virol. 2009;45:174-8. [ ] 9. Centers for Disease Control and Prevention (CDC). Swine-origin influenza A (H1N1) virus infections in a school - New York City, April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:470-2. [ ] 10. Senna MC, Cruz DV, Pereira ACG, et al. Emergência do vírus influenza A-H1N1 no Brasil: a propósito do primeiro caso humano em Minas Gerais. Rev Med Minas Gerais. 2009;19:173-6. [ ] 11. Ho YC, Wang JL, Wang JT, et al. Prognostic factors for fatal adult influenza pneumonia. J Infect. 2009;58:439-45. [ ] 12. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Protocolo de manejo clínico e vigilância epidemiológica da influenza. Brasília: Ministério da Saúde; 2009. [ ] 13. Ginocchio CC, Zhang F, Manji R, et al. Evaluation of multiple test methods for the detection of the novel 2009 influenza A (H1N1) during the New York City outbreak. J Clin Virol. 2009;45:191-5. [ ] 14. Whiley DM, Bialasiewicz S, Bletchly C, et al. Detection of novel influenza A (H1N1) virus by real-time RT-PCR. J Clin Virol. 2009;45:203-4. [ ] 15. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Situação epidemiológica da nova influenza A (H1N1) no Brasil, 2009. [acessado em 20 de setembro de 2009]. Disponível em: http://portal.saude.gov.br/portal/aplicacoes/noticias/default.cfm?pg=dspDetalheNoticia&id_area=124&CO_NOTICIA=10536 [ ] 16. Kim EA, Lee KS, Primack SL, et al. Viral pneumonias in adults: radiologic and pathologic findings. Radiographics. 2002;22 Spec No:S137-49. [ ] 17. Matar LD, McAdams HP, Palmer SM, et al. Respiratory viral infections in lung transplant recipients: radiologic findings with clinical correlation. Radiology. 1999;213:735-42. [ ] 18. Qureshi NR, Hien TT, Farrar J, et al. The radio-logic manifestations of H5N1 avian influenza. J Thorac Imaging. 2006;21:259-64. [ ] 19. Oikonomou A, Müller NL, Nantel S. Radiographic and high-resolution CT findings of influenza virus pneumonia in patients with hematologic malignancies. AJR Am J Roentgenol. 2003; 181:507-11. [ ] 20. Bay A, Etlik Ö, Öner AF, et al. Radiological and clinical course of pneumonia in patients with avian influenza H5N1. Eur J Radiol. 2007;61:245-50. [ ] 21. Tanaka N, Matsumoto T, Kuramitsu T, et al. High resolution CT findings in community-acquired pneumonia. J Comput Assist Tomogr. 1996;20:600-8. [ ] 22. Tran TH, Nguyen TL, Nguyen TD, et al. Avian influenza A (H5N1) in 10 patients in Vietnam. N Engl J Med. 2004;350:1179-88. [ ] Received October 8, 2009. * Study developed at Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM) and at Hospital e Maternidade São Luiz, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554