Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 5 - Sep. / Oct. of 2009
Vol. 42 nº 5 - Sep. / Oct. of 2009
|
REVIEW ARTICLE
|
|
Imaging evaluation of vocal cord paralysis |
|
|
Autho(rs): Marcelo de Mattos Garcia, Fabiana Pizanni Magalhães, Gabriela Bijos Dadalto, Marina Vimieiro Timponi de Moura |
|
|
Keywords: Vocal cord, Paralysis, Imaging |
|
|
Abstract:
ITitular Members of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MDs, Radiologists, Axial Centro de Imagem, Belo Horizonte, MG, Brazil
INTRODUCTION Vocal cord paralysis is a frequent cause of hoarseness, and may be secondary to several conditions along the vagus nerve (paired cranial nerve X) pathway and its branches. The recognition of specific radiological findings, as well as the knowledge on the anatomy and diseases that may affect the paired cranial nerve X are extremely important for the choice and programming of the best imaging method to be utilized, and for an appropriate interpretation of images. In the present study, the authors sought to demonstrate radiological findings indicative of vocal cord paralysis. Additionally, the strategies for evaluation of computed tomography (CT) and magnetic resonance imaging (MRI) studies were focused in the research of the main causes of the condition, illustrating them with typical cases.
ANATOMY The vagus nerve is the longest of the cranial nerves, extending from the brainstem to the abdomen(1). It originates from four nuclei in the bulb, three of them converging in the basal cistern to form a single nerve that emerges from the skull through the jugular foramen, passing through the neck and chest to the abdomen. In this long course, the vagus nerve gives rise to a number of branches to innervate the larynx and the pharynx. In the cervical region, it passes between the carotid artery (medially) and the internal jugular vein (laterally). There are three major branches of the vagus nerve in this region: the pharyngeal, superior laryngeal and the recurrent laryngeal nerves. The pharyngeal branch originates from the inferior ganglion of the vagus nerve and is part of the pharyngeal plexus, responsible for the motor innervation of the pharyngeal and levator veli palatine muscles. The superior laryngeal nerve also originates from the inferior ganglion of the vagus nerve, caudally to the pharyngeal branch, and is divided into external laryngeal nerve (motor) and internal laryngeal nerve (sensory). It is responsible for the cricothyroid muscle innervation. The recurrent laryngeal nerves (RLNs) (Figure 1) are responsible for the innervation of the other intrinsic muscles of the larynx(2). These nerves carry motor, sensory and parasympathetic fibers, dividing itself into internal branch, responsible for the sensory function of the vocal cords and subglottic region, and external branch that bears the motor function of four intrinsic laryngeal muscles: thyroarytenoid, anterior and posterior cricoarytenoid, oblique and transverse arytenoid muscles(3). At right, the RLN emerges anteriorly from the vagus nerve at the intersection with the right subclavian artery to loop under and around the artery to reach its posterior surface. Then, it runs superiorly in the tracheoesophageal cleft towards the larynx. The left RLN emerges from the vagus nerve in the mediastinum, after crossing it anterolaterally to the aortic arch to loop under the arch and running between the aorta and the left pulmonary artery, extending posteriorly to the tracheoesophageal cleft to reach the larynx. Because of its longer and partially intrathoracic course, the left RLN may be affected by mediastinal diseases(1). Both nerves enter the larynx in the region of the cricothyroid joint through the fibers of the inferior constrictor muscle of the pharynx.
In the RLN ascending course from the chest to the larynx, a number of anatomical variations may be found. Rustad(4), in a post-mortem series has observed that 43% of the RLNs split into one or more branches on both sides. The findings of nerve branching before reaching the larynx have also been surgically confirmed by Nemiroff & Katz(5) in 40% of cases. The path of the RLNs may change because of congenital vascular abnormalities or anatomical distortions resulting from the presence of goiter, neoplasias or inflammatory processes. In cases of aberrant subclavian artery, the right RLN runs directly from the vagus nerve to the larynx, without looping around the respective artery. This variation is closely related to surgical injuries and is known as "non-recurrent" inferior laryngeal nerve. The RLN is localized in the tracheoesophageal cleft that is a relevant anatomical landmark, in 65% of cases at right, and in 77%, at left. The nerve is found at the right side of the trachea in 33% of cases, and at left, in 22%. It rarely ascends anterolaterally to the trachea and, in this case, it is more susceptible to surgical injury.
CLINICAL FINDINGS Usually, patients with vocal cord paralysis present with complaint of hoarseness. Other more severe symptoms include frequent aspiration and pneumonia(6). However, up to 35%f patients may be asymptomatic(5). In these cases, vocal cord paralysis will be incidentally identified, and this finding should alert the clinician to the necessity of additional evaluation. The previous and direct evaluation by laryngoscopy must be initially performed to rule out the presence of mucosal and submucosal lesions like those caused by squamous cell carcinoma, to justify a subsequent imaging study. Vocal cord paralysis may be acute or chronic, and may occur in one or both vocal folds. The left vocal cord is most frequently affected, because of the longer course of the left recurrent laryngeal nerve, with about 12 cm in length from the aorta to the cricothyroid joining. At clinical examination, the identification of the affected side is relatively simple: the truly involved vocal fold will be with a complete or partially reduced mobility.
IMAGING DIAGNOSIS The classic findings of vocal cord paralysis can be observed on plain radiographs and, particularly, on sectional imaging methods such as CT and MRI. These studies should include a scan from the skull base thru the aortic-pulmonary window, covering the whole course of the RLN. CT should include pre- and post-contrast phases, sometimes with a phonation phase with vocalization of the vowel i. This acquisition is useful in the evaluation of the true vocal folds mobility, but should be cautiously used to minimize the exposure of the patient to ionizing radiation. The study includes axial acquisitions with later 3D coronal and sagittal multiplanar reconstructions. The CT and MRI parameters utilized in the authors' institution are shown on Table 1.
The bulging of the oropharyngeal and hypopharyngeal contour in association with the thinning of the constrictor muscle constitutes an evidence of a lesion in the ipsilateral pharyngeal plexus(7). Such findings indicate that the abnormality is localized immediately below the skull base or more cranially in the posterior fossa. Most of imaging findings related to RLN paralysis are secondary to the thyroarytenoid muscle atrophy (Figure 2)(7). At least ten findings associated with this nerve paralysis are described by Landman(8) in laryngoscopic studies. Notwithstanding the limitations of the method, these findings were transferred for analysis by axial CT. Several findings correlated the CT images with vocal cord paralysis(7); among them, the following can be mentioned: – thickening and medial displacement of the ipsilateral aryepiglottic fold (the most frequent finding) (Figure 3); – dilatation of the pyriform sinus (Figure 4); – dilatation of the ipsilateral laryngeal ventricle (Figure 5); – antero-medial displacement of the ipsilateral arytenoid cartilage (Figure 6); – dilatation of the ipsilateral vallecula; – flattening of the subglottic arch demonstrated on coronal images.
The first two findings above described are observed in more than 75% of cases, constituting the most reliable diagnostic criteria. With the advent of multidetector CT, high-resolution reformatted coronal images have provided a higher capacity for analyzing the larynx. However, the authors emphasize that axial images allow a correct diagnosis in most of cases.
CAUSES There are several causes of vocal cord paralysis, and approximately 50% of reported cases are toxic or idiopathic(7). Thus, in at least half of patients, sectional images may fail in identifying lesions along the vagus and recurrent laryngeal nerves path. In the past, the most common cause of vocal cord paralysis was thyroid surgery with dissection of the Berry's ligament, the site where the RLN penetrates the larynx. In these cases, the lesions result from an excessive traction of the thyroid gland, or occur at the moment of the hemostasis. The RLN may be connected with the inferior thyroid vessels, therefore its identification during the surgical procedure is essential. Recently, lung (Figure 7) and skull base neoplasms, as well as surgical injuries have been the most frequent causes of vocal cord paralysis.
Several diseases may affect the vagus nerve tract (Figure 8), leading to vocal cord paralysis. Thus, it is necessary to evaluate this nerve from the brainstem to the carina. The causes of vocal cord paralysis may be divided into central origin (vagal neuropathy) and peripheral (RLN neuropathy), the latest being most frequently observed, achieving up to 90% of cases in some series. However, in most (up to 85%), lesions have not been identified along the nerves pathway.
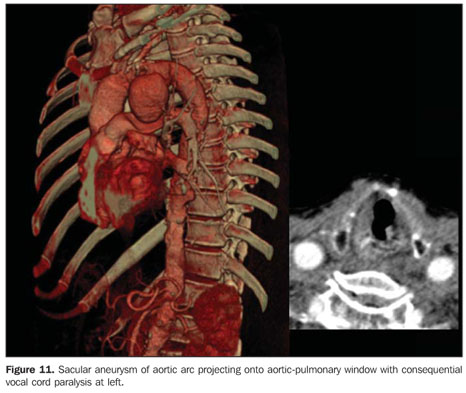
Among the central causes, lesions affecting the brainstem, the skull base and the carotid bifurcation can be mentioned, all of them also associated with vagal neuropathy. In this group, vagal paragangliomas, hypervascularized masses involving or compressing the whole cranial nerve X pathway, as well as their nuclei in the jugular foramen can be clearly demonstrated on contrast-enhanced phases at CT and MRI(9). Vascular events involving, for example, the posterior-inferior cerebellar artery leading to occlusion, may compromise the ambiguous nucleus in the dorsolateral aspect of the bulb. Thus, infarcts in this area may justify ipsilateral vocal cord paralysis(10). Central vagal neuropathy may be suspected in the setting of paralysis or paresis of the pharyngeal constrictor muscles in cases where the pharyngeal plexus is involved. The pharyngeal plexus is formed by branches of cranial nerves IX, X and XI, besides branches of the sympathetic trunk. The vagal branches emerge from the nodose ganglion localized below the skull base, and penetrate the pharyngeal muscles, branching into the superior and inferior constrictor muscles. A lesion affecting the pharyngeal plexus will cause paresis or paralysis of the ipsilateral constrictor muscles, eventually leading to atrophy. Peripheral causes include RLN invasion by thyroid and cervical esophageal tumors (respectively Figures 9 and 10). Four percent of patients with unilateral vocal cord paralysis present thyroid disease, but only 0.7% are benign. Locally invasive thyroid cancers must be correctly evaluated by imaging methods, considering that the laryngotracheal invasion justifies the RLN involvement with subsequent vocal cord paralysis(11). Advanced malignant esophageal tumors may extend towards the tracheoesophageal groove, the RLN pathway(12). On the left side, aortic aneurysms (Figure 11), cardiomegaly, and upper lobe lung tumors are implicated as potential causes of vocal cord paralysis. On the right side, supraclavicular tumors and subclavian artery aneurysms are considered as causal factors. Pancoast tumors, also known as superior sulcus tumors, are typically bronchogenic non-small-cell carcinoma, usually of squamous-cell type, affecting the superior sulcus that is the pathway of the right RLN(13).
Vocal cord paralysis may also be associated with peripheral neuritis triggered by alcoholism, viruses, acute bacterial infections and drugs toxicity. Neurological diseases associated with multiple sclerosis, poliomyelitis, myasthenia gravis, amyotrophic lateral sclerosis, cerebrovascular disease and acromegaly complications are also implicated.
CONCLUSION Considering that up to 35% of patients with vocal cord paralysis are asymptomatic, the recognition of radiological findings indicative of this condition is essential for the radiologist who must warn the referring physician on the imaging findings. Additionally, imaging methods, particularly the sectional ones, allow the study of the whole paired cranial nerve X and RLNs identifying the several diseases affecting this region. Thus, the knowledge of local anatomy and related diseases is of great importance for the radiologist, so that he can tailor the examination properly to allow an appropriate diagnosis and therapy planning.
REFERENCES 1. Curtin HD. The larynx. In: Som PM, Curtin HD, editors. Head and neck imaging. 4th ed. St. Louis: Mosby; 2003. p. 1601–3. [ ] 2. O'Rahilly R. Cabeça e pescoço: faringe e laringe. In: Gardner E, Gray DJ, O'Rahilly R, editors. Anatomia: estudo regional do corpo humano. 4ª ed. Rio de Janeiro: Guanabara Koogan; 1988. p. 730–50. [ ] 3. Ardito G, Revelli L, D'Alatri L, et al. Revisited anatomy of the recurrent laryngeal nerves. Am J Surg. 2004;187:249–53. [ ] 4. Rustad VH. Revised anatomy of recurrent laryngeal nerves: surgical importance based on dissection of 100 cadavers. J Clin Endocrinol Metab. 1954;14:87–96. [ ] 5. Nemiroff PM, Katz AD. Extralaryngeal divisions of the recurrent laryngeal nerve. Surgical and clinical significance. Am J Surg. 1982;144:466–9. [ ] 6. Ramadan HH, Wax MK, Avery S. Outcome and changing cause of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 1998;118:199–202. [ ] 7. Chin SC, Edelstein S, Chen CY, et al. Using CT to localize side and level of vocal cord paralysis. AJR Am J Roentgenol. 2003;180:1165–70. [ ] 8. Landman GHM. Laryngography and cinelaryngography. Baltimore: Williams & Wilkins; 1970. [ ] 9. Rao AB, Koeller KK, Adair CF. From the Archives of the AFIP. Paragangliomas of the head and neck: radiologic-pathologic correlation. Radiographics. 1999;19:1605–32. [ ] 10. Cornier PJ, Long ER, Russell EJ. MR imaging of posterior fossa infarctions: vascular territories and clinical correlates. Radiographics. 1992;12:1079–96. [ ] 11. Dedivitis RA, Guimarães AV. Carcinoma papilífero da tireóide localmente invasivo. Rev Bras Otorrinolaringol. 2002;68:687–91. [ ] 12. Duarte BB, Mikinev RM, Costa KC, et al. Paralisia bilateral em abdução de pregas vocais como manifestação de câncer de esôfago: relato de caso e revisão de literatura. Arq Int Otorrinolaringol. 2006;10:327–30. [ ] 13. Duarte RLM, Almeida MHH, Paschoal MEM. Tumor de Pancoast e carcinoma gástrico primários e sincrônicos. Pulmão RJ. 2005;14:75–8. [ ] Received November 18, 2008. Accepted after revision July 28, 2009. * Study developed at Axial Centro de Imagem, Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554