Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 4 - July / Aug. of 2009
Vol. 42 nº 4 - July / Aug. of 2009
|
CASE REPORT
|
|
Ruptured hepatic cavernous hemangioma: a case report and literature review |
|
|
Autho(rs): Walter Teixeira de Paula Neto, Ana Celia Baptista Koifman, Carlos Alberto de Souza Martins |
|
|
Keywords: Hepatic hemangioma, Hemoperitoneum, Computed tomography, Acute abdomen |
|
|
Abstract:
IMD, Radiologist at Division of Radiology and Diagnostic Imaging - Hospital Uniclínicas, Chapecó, SC, Brazil
INTRODUCTION Spontaneous hepatic hemorrhage is an uncommon condition, and in the absence of trauma or anticoagulant therapy, it frequently occurs as a consequence of the subjacent hepatic disease(1). The most common causes of nontraumatic hepatic hemorrhages are hepatocellular carcinoma and hepatic adenoma(2). There are few cases of spontaneous rupture of cavernous hemangioma(3) reported in the literature. Radiological findings reveal hemoperitoneum and heterogeneous hepatic mass. Intraperitoneal clot may also be identified adjacent to the site of the bleeding(4).
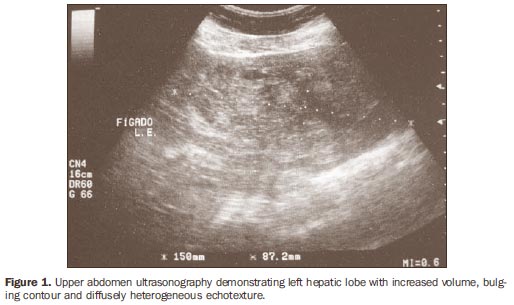
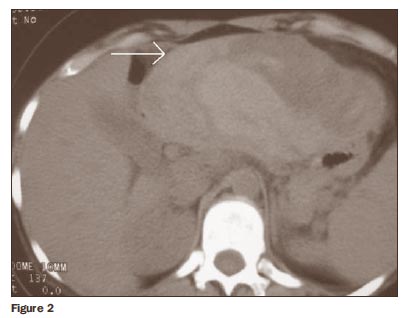
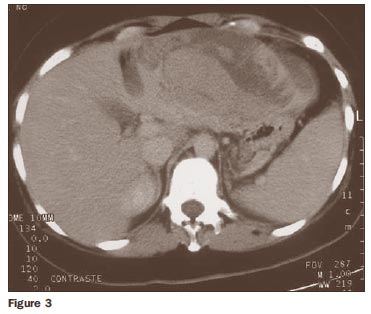
CASE REPORT Female, 31-year-old patient presenting with acute abdomen. There was no history of subjacent abdominal disease. The patient was using oral contraceptives. At physical examination the patient presented a tense abdomen, with pain at light and deep palpation in the epigastrium and right hypochondrium regions. Laboratory analysis showed a subtle decrease in hematocrit (34%) and hemoglobin (11 g/dl) levels. Abdominal ultrasonography (US) was performed, demonstrating increased volume of the left hepatic lobe, with diffusely heterogeneous echotexture corresponding to intermingled, poorly defined, hypo and hyperechoic areas (Figure 1). Abdominal computed tomography (CT) evidenced hypo and hyperdense areas, at times reaching a density of 40 UH, without contrast enhancement, compromising almost the whole left hepatic lobe, compatible with acute hematoma (Figures 2 and 3).
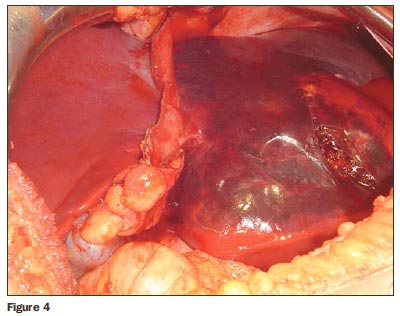
The patient was submitted to exploratory laparotomy, which demonstrated a large reddish tumor taking up almost entirely the left hepatic lobe (Figure 4).
The histopathological diagnosis was ruptured cavernous hemangioma involved by hepatic tissue with recent hematomas.
DISCUSSION Spontaneous hepatic hemorrhage is a very uncommon condition, and in the absence of trauma or anticoagulant therapy, it frequently occurs as a consequence of a subjacent hepatic disease(1). The most common nontraumatic causes of spontaneous hepatic hemorrhage are hepatocellular carcinoma and hepatic adenoma, and it also may occur in patients with focal nodular hyperplasia, hemangioma, angiosarcoma and metastases(1-3). Cavernous hemangioma is the most common benign hepatic tumor(4,5), with greater prevalence in women. In general, they are single tumors, smaller than 5 cm, and cause no symptoms(6). There are few cases of hemorrhage and spontaneous rupture of these lesions reported in literature(3). Giant hemangiomas > 10 cm are the most likely ones to rupture, particularly when associated with trauma or during pregnancy(3,7). At US these lesions present a nonspecific appearance, with large dimensions, heterogeneous echotexture and poorly defined limits(6). Magnetic resonance imaging (MRI) is the most sensitive method for detection of acute abdominal bleeding(5). However CT is more widely utilized for such purpose, due to shorter acquisition time, lower cost and wider availability as compared with MRI(2). At the first 48 hours, noncoagulated blood is observed with a high density (30-45 UH), due to the high proteic content. These values may change according to the hematocrit levels and bleeding progression time(3). In patients with hepatic hemangioma, the imaging diagnosis of lesional hemorrhage is suggested in the presence of a large lesion (> 10 cm), increased echogenicity at US, increased attenuation at CT or areas with hypersignal on T1-weighted sequences at MRI(1). These findings may be associated with subcapsular hematoma or hemoperitoneum(4).
CONCLUSION The diagnosis of nontraumatic hepatic hemorrhage should always be suspected in patients presenting sudden abdominal pain, particularly in patients using anticoagulant drugs or with preexisting hepatic lesions. Although rare, ruptured hepatic hemangiomas are surgical emergencies with high mortality rates. CT is the appropriate method for hepatic evaluation due to rapid image acquisition and the possibility of dynamic studies(8).
REFERENCES 1. Casillas VJ, Amendola MA, Gascue A, et al. Imaging of nontraumatic hemorrhagic hepatic lesions. Radiographics. 2000;20:367-78. [ ] 2. Lubner M, Menias C, Rucker C, et al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 2007;27:109-25. [ ] 3. Hanbidge AE, Buckler PM, O'Malley ME, et al. Imaging evaluation for acute pain in the right upper quadrant. Radiographics. 2004;24:1117-35. [ ] 4. Vilgrain V, Boulos L, Vullierme MP, et al. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000;20: 379-97. [ ] 5. D'Ippolito G, Appezzato LF, Ribeiro ACR, et al. Apresentações incomuns do hemangioma hepático: ensaio iconográfico. Radiol Bras. 2006;39: 219-25. [ ] 6. Machado MM, Rosa ACF, Lemes MS, et al. Hemangiomas hepáticos: aspectos ultra-sonográficos e clínicos. Radiol Bras. 2006;39:441-6. [ ] 7. Coumbaras M, Wendum D, Monnier-Cholley L, et al. CT and MR imaging features of pathologically proven atypical giant hemangiomas of the liver. AJR Am J Roentgenol. 2002;179:1457-63. [ ] 8. Pereira IMR, Álvares BR, Baracat J, et al. Estudo de 50 casos por tomografia computadorizada de lesões hipodensas hepáticas fundamentais na infância. Radiol Bras. 2006;39:103-6. [ ] Received November 25, 2007. * Study developed at Life Imagem - Hospital Evangélico, Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554