Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 4 - July / Aug. of 2009
Vol. 42 nº 4 - July / Aug. of 2009
|
ORIGINAL ARTICLE
|
|
Dosimetric evaluation of a combination of brachytherapy applicators for uterine cervix cancer with involvement of the distal vagina |
|
|
Autho(rs): Roger Guilherme Rodrigues Guimarães, Heloisa de Andrade Carvalho, Silvia Radwanski Stuart, Rodrigo Augusto Rubo, Rodrigo Migotto Seraide |
|
|
Keywords: Cervical cancer, Radiotherapy, Intracavitary brachytherapy, Dosimetry |
|
|
Abstract:
Roger Guilherme Rodrigues GuimarãesI; Heloisa de Andrade CarvalhoII; Silvia Radwanski StuartIII; Rodrigo Augusto RuboIV; Rodrigo Migotto SeraideV
INTRODUCTION Uterine cervix cancer is the second most frequent malignant tumor in women, with approximately 550,000 new cases being diagnosed every year, and causing 270,000 deaths per year(1). In Brazil, it is estimated that uterine cervix cancer is the third most common malignant neoplasm affecting women, after non-melanoma skin cancers and breast cancer, and the fourth most common cause of cancer death. According to the Instituto Nacional do Câncer, the estimated incidence rate for 2008, was 19 cases per 100,000 women, corresponding to 18,680 of expected new cases(2). The standard treatment for most patients with invasive cervix cancer is concomitant radiochemotherapy. The global benefit obtained from this association, as compared with radiotherapy alone is about 12%, due to better local control, and overall and disease-free survival rates(3-7). Therefore, local control represents an important factor impacting the survival of such patients. Radiotherapy consists of a combination of external pelvic irradiation with intracavitary brachytherapy. In spite of the low incidence of cases with stage IIIa (FIGO(8)), where the distal third of the vagina is involved, many patients in more advanced stages of disease also present infiltration of distal half or third of the vagina(9). Patients presenting involvement of the distal vagina by the tumor are usually submitted to intracavitary brachytherapy with intrauterine tandem and vaginal cylinder. However, the uterine cervix, where the larger tumor volume is located, is underdosed, if one compares this technique with that using intrauterine tandem and ovoids or ring. On the other hand, with such technique, the lower half of the vagina is underdosed. The ideal situation would be utilizing a gynecologic applicator specially developed for these cases, associating an adequate coverage of the uterine cervix tumor with an appropriate treatment of the vaginal disease. For low dose-rate brachytherapy, some prototypes have already been developed(10,11). However, concerning high dose-rate brachytherapy, besides the applicator with the tandem and cylinder, only applicators for individual treatment of either cervical or vaginal diseases are available. Thus, we decided to study a treatment technique using a combination of two gynecologic applicators already available (intrauterine tandem and ring in combination with the vaginal cylinder), where the 100% isodose of brachytherapy would involve more adequately the tumor in the described situation, without increasing the risks of toxicity.
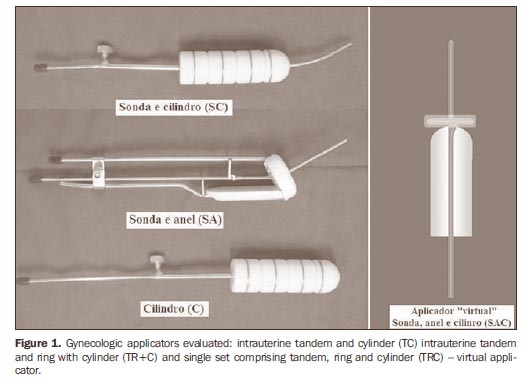
MATERIALS AND METHODS A theoretical study comparing three high dose-rate brachytherapy techniques was undertaken. The applicators most frequently utilized in our daily practice were selected as follows: a 60 mm tandem and 30 mm-diameter cylinder (TC) (Nucletron BV®; Veenendaal, Netherlands); tandem/ ring applicator - r30i60 (Nucletron®) - 60 mm tandem, 30 mm-diameter ring, and 60º angle, with rectal retractor, associated with the 30 mm diameter vaginal cylinder (intrauterine tandem and ring + cylinder: TR+C) (Nucletron®). Additionally, a virtual applicator was idealized to simulate the 60 mm intrauterine tandem, with ring (30 mm diameter) and vaginal cylinder (30 mm diameter) in a single set (TRC) (Figure 1). Treatments were simulated with each one of these applicators, with a prescribed dose of 7 Gy to point A and 5 Gy to the vaginal mucosa surface or at a 5 mm depth by 6 cm extent. The volumes involved by the 50% (V50), 100% (V100), 150% (V150) and 200% (V200) isodoses, respectively, were evaluated, besides the doses to the organs at risk, according to the ICRU 38 recommendations(12).
Besides the reference points A, B, rectum and bladder, the following points were also considered: a) a sigmoid point - the midpoint on a straight line from the extremity of the intrauterine tandem to the promontory on the lateral radiographic image and its projection on the center of the patient at the anteroposterior radiographic image; b) two additional points for the rectum - 2.5 and 5 cm caudal to the ICRU 38 point and in the same plane (Figure 2). The points for dose evaluation in the vagina were defined at 15 mm from the cylinder source axis, corresponding to the applicator surface/vaginal mucosa surface, and at 20 mm, corresponding to the dose at a 5 mm depth, respectively, throughout the treatment extent of 6 cm.
For the simulations, semiorthogonal radiographs of an actual case treated with the selected ring applicator (r30i60) were used. The calculations were performed with the Plato v 13.0 (Nucletron®) 3D planning system for brachytherapy. According to the standard established in our institution, the prescribed dose per fraction is 7 or 7.5 Gy to point A, without optimization, when the ring applicator is used. If necessary, in order to maintain the doses on the organs at risk within the tolerance limits, individualized manual optimization is utilized. In cases requiring irradiation of the whole vagina, the intrauterine tandem with vaginal cylinder (TC) is used, and the calculation of 7 Gy is done at 2 cm from the intrauterine tandem axis, and 5 Gy on the cylinder surface, when there is no macroscopic residual disease in the vagina, or at a 5 mm depth if vaginal disease is still present, with "optimization on dose points". The doses to the points of the organs at risk should be kept below 60% to 65% of the dose prescribed for point A, i.e., absolute doses < 4.5 Gy. When the prescription is at 5 mm depth in the vaginal mucosa, a maximum dose of 5 Gy to the points of the organs at risk is accepted. Therefore, for each applicator, calculations were made with 7 Gy to point A and 5 Gy at the cylinder surface and at 5 mm depth. The calculation for TC followed the previously described steps (Figure 3). The simulation of the TR+C was idealized for a two-phase treatment, in a single application where, after the treatment with the tandem/ring applicator, it would be replaced by the cylinder for vaginal irradiation. A 7 Gy dose was calculated, as usual, on point A with TR, and subsequently, for the loading of the vaginal cylinder, the vaginal extent covered by the 5 Gy isodose obtained from the calculation with TR was measured. This extent was subtracted from the proximal loading of the cylinder. The sum of the two plans generated a final isodose of 100%, where point A received 7 Gy and the dose to the vagina was 5 Gy (on the surface or at a 5 mm depth) (Figure 4). The virtual applicator (TRC) was created to simulate an application in a single phase, without the need to change applicators. For the calculation, the same loading scheme obtained with the TR+C combination was adopted, achieving with a single plan, the same final isodose of 100% (Figure 5). In all situations, if necessary, adjustments in the source dwell times were made by means of manual optimization, in order to keep the doses to the organs at risk below the tolerance limits.
The volumes involved by the respective treatment isodoses were calculated and compared: V50 (50%), V100 (100%), V150 (150%), V200 (200%), for prescriptions of 7 Gy to point A and 5 Gy on the surface or at a 5 mm depth in the vaginal mucosa, respectively.
RESULTS Tables 1 and 2 present the results obtained in the analyzed situations and the relationships between the volumes obtained with TC and TRC with TR+C. Among the three simulated treatments, the one utilizing TC presented larger volumes irradiated with low doses and smaller volumes with high doses when the 5 Gy dose was calculated on the vaginal surface. All the volumes were larger when this dose was calculated at a 5 mm depth. Looking at the dose distribution, the largest irradiated volumes were obtained by the larger irradiation of the uterine body in relation to the tumor area itself (Figure 3).
By comparing the values obtained with the simulation of TR+C and TRC for the calculation of 5 Gy on the surface of the vaginal mucosa (Table 1), it was observed that, with TRC the 7 Gy volume can be slightly increased (4% to 5%), while the high dose volumes are the lowest (approximately 50% lower than with TR+C). Regarding the low doses volumes, the ones receiving 5 Gy or 2.5 Gy are also larger with the TRC. However, the volume receiving 3.5 Gy (V50) was larger when the TR+C was used. On the other hand, when the 5 Gy prescription was changed for 5 mm depth, all the 100% or less dose volumes were larger (around 10% to 15%) with the TRC. Again, TR+C presented larger high dose volumes, mainly V200 (12%). With TR+C or TRC, both the region of the uterine cervix ("tumor") and the vaginal "disease" were appropriately covered by the 100% isodose. The high-dose volumes comprised mainly the uterine cervix region at the widest portion of the classical "pear shaped" isodose, at the same time that a great part of these volumes was contained within the cylinder, in the vaginal portion (Figures 4 and 5).
DISCUSSION Uterine cervix tumors, like other neoplasms, when locally advanced, present a higher probability of recurrence. An extremely important aspect of the treatment and local control of these tumors is the possibility of performing intracavitary brachytherapy, with the delivery of high doses to the tumor volume, at the same time preserving the surrounding healthy tissues, due to the steep dose gradient generated. Classically, the dose prescription in brachytherapy for uterine cervix cancer is on point A, which does not reflect the dose to the existing tumor volume. In spite of being published for more than 20 years ago, the recommendations of the ICRU report n. 38(12) still remain as the main reference and guideline for brachytherapy of gynecologic tumors(13). However, significant changes have occurred, resulting in developments in the brachytherapy technique, such as improvement in images acquisition, novel 3D planning systems, availability of safer and more reliable equipment, and development of highdose-rate brachytherapy, among others. In spite of all that, because of the good results achieved and the high cost of this more advanced technology, most centers still perform gynecologic brachytherapy based exclusively on 2D planning and dose evaluation in points. However, the dose prescription in one point is attached to some problems, such as the great variation in the dose to the tumor, due to the greater heterogeneity of the prescribed dose, and also the difficulties in reproducibility and definition of the point. In cases where the presence of an extensive vaginal lesion is observed in addition to the uterine cervix disease, these problems are even greater, as the whole tumor volume must be appropriately irradiated both in the uterine cervix and in the vaginal area. In order to improve the brachytherapy quality delivered to the patients with uterine cervix tumors, particularly those with involvement of the distal portion of the vagina, we developed a preliminary theoretical study, based on the prescription on dose points routinely adopted by our institution. Also, a study of the irradiated volumes was associated, although without the appropriate imaging studies, but following some evaluation parameters already described for other brachytherapy techniques(14). We could observe that the treatment with TC is the one that irradiates the largest volumes, although with larger irradiation of the uterine body and not of the tumor volume itself. In other words, in spite of its indication for such cases, it does not represent the best therapeutic option. The dosimetric study demonstrated that the dose distribution achieved with the combination of two applicators may be similar to that achieved with a single applicator especially designed for these cases. The placement of the vaginal cylinder after the treatment with TR to complement the dose to the distal portion of the vagina is simple, feasible and safe. In spite of eventual inconveniences of changing applicators and increased treatment time, patients presenting with uterine cervix cancer extending to the lower vaginal third may potentially benefit from this technique(10,15). Other authors have developed a similar study combining two gynecologic high dose-rate brachytherapy applicators: intrauterine tandem and mini-ovoids, and intrauterine tandem and vaginal cylinder(15). The authors have reported the treatment results based on calculations performed by a homemade planning software that generates a "galaxy-shaped" isodose. Twenty-two patients with disease at stages IIB to IVA were treated with the technique. With a median 87.4-month follow-up, a disease-free survival rate of 90.7% and overall five-year survival rate of 81.8% were observed, respectively. Grade 2 toxicity was 4.5% (one patient with proctitis). However, for calculations, two semi-orthogonal radiographs sets were necessary: one with the intrauterine tandem and vaginal cylinder and another with the tandem and colpostates. And, for the treatment, once more, the patient was submitted to the change of applicators. An interesting aspect to be noticed in this study, was the fact that there was a decrease of 10% to 15% in the relative weight in the ovoids loading, to avoid an increase in the prescribed dose in point A. In the present study, the combination of applicators presented larger high dose volumes, mainly due to the overlap of the two plans. However, when the 3D dose distribution is considered, a great part of these volumes is contained in the region of highest risk (uterine cervix), or within the cylinder (Figure 4). On the other hand, the virtual applicator presents a steeper dose gradient, with larger low dose volumes. It was possible to keep the values at the points of the organs at risk below the tolerance doses in all the evaluated situations. However, some considerations regarding the methodology of our study should be made. The high dose volumes were calculated in relation to the prescribed dose at point A (7 Gy). With the prescribed dose of 5 Gy in the vagina, the high dose volumes in this region, besides corresponding to lower doses (V150 = 7.5 Gy and V200 = 10 Gy), will be within the vaginal cylinder. Only one model of each applicator was used, and the calculations should be validated for the existing alternatives: different angles and intrauterine tandem lengths, variations in ring and cylinder diameters, applicators using ovoids, and others. For the simulation, the radiographs of a real case treated with TR, were used, where the reconstruction of the applicator was based on the corresponding standard applicator already described in the planning system. The tandem of the TR applicator is straight, while the tandem of the TC applicator is curved. This fact may have caused a difference, albeit negligible, in the calculations of the respective volumes. However, the dose distribution with TC will never be equivalent to that obtained with ring or ovoids, in relation to the widening of the isodoses in the cervix portion. Ring and cylinder with the same diameter (30 mm) were selected, in accordance with the routine use in our institution. However, the ring diameter is defined in relation to the source axis and its actual external diameter, with the cap, is 40 mm. This fact should be taken into account when selecting the applicator that better fits the patient. Additionally, anatomic variations caused by the replacement of applicators could not be evaluated. In this aspect, perhaps a single applicator could be more appropriate, avoiding changes in the uterus position and distortions of the vaginal walls. This would also avoid the uncertainty originated from the isodoses overlapping for the definition of the cylinder portion that needs to be loaded. This aspect could be better evaluated with the use of computed tomography or magnetic resonance imaging in a real case, as the reproducibility of anatomic variation in a phantom might be questionable. The use of thermoluminescent dosimeters might also add more safety in the validation of the calculations, and allow better optimization. In any instance, the higher dose volumes generated by the isodoses overlapping, would still be within the cylinder, in the vaginal portion. The methods of calculation for TC ("optimization in dose points" only) and for TR+C and TRC ("non-optimized" for dose in point A and "optimization of dose points" for the vagina) were slightly different, due to the applicators' characteristics and interaction with the planning system. This fact might also have interfered in the volume calculation, but this is an actual limitation of the currently available system. The applicators with the desired characteristics developed for low dose-rate(10,11)had the purpose of minimizing eventual uncertainties of the combination of two applicators, besides eliminating the inconvenience and discomfort of an additional hospital stay for treatment of the vaginal portion. In one of the studies(10), the applicator was used clinically, with satisfactory, although preliminary results. For high dose-rate, however, there is not an applicator especially designed to provide the desired coverage for tumors in such conditions. A 3D study, based on magnetic resonance imaging, has been already designed for better evaluation of all these aspects. It is important to emphasize that the clinical validation of the method for later development of an applicator with the ideal configuration, or of an accessory that adapts to applicators currently in routine use, is necessary. This latter alternative would be welcome in the medical environment, considering the cost reduction and easing of the procedure.
CONCLUSION The combination of two available applicators (intrauterine tandem and ring + cylinder: TR+C) presented an adequate dose distribution considering the coverage of the tumor and sparing of the organs at risk. Clinical validation is still necessary for implementation of the method in the daily routine.
REFERENCES 1. National Institutes of Health Consensus Development Conference statement on cervical cancer. April 1-3, 1996. Gynecol Oncol. 1997;66:351-61. [ ] 2. Brasil. Ministério da Saúde. Instituto Nacional de Câncer - INCA. Estimativa de incidência e mortalidade por câncer. Rio de Janeiro: INCA; 2008. [ ] 3. Rose PG, Bundy BN, Watkins EB, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340:1144-53. [ ] 4. Whitney CW, Sause W, Bundy BN, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999;17:1339-48. [ ] 5. Peters WA 3rd, Liu PY, Barrett RJ 2nd, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000;18:1606-13. [ ] 6. Green JA, Kirwan JM, Tierney JF, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet. 2001;358:781-6. [ ] 7. Eifel PJ. Chemoradiotherapy in the treatment of cervical cancer. Semin Radiat Oncol. 2006;16: 177-85. [ ] 8. Benedet JL, Bender H, Jones H 3rd, et al. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2000;70:209-62. [ ] 9. Aisen S. Braquiterapia de alta taxa de dose no tratamento do câncer do colo uterino: resultados de controle local, sobrevida e complicações [tese de doutorado]. São Paulo: Universidade de São Paulo; 2003. [ ] 10. Wolfson AH, Wu X, Takita C, et al. A novel applicator for low-dose-rate brachytherapy of gynecological cancers. Int J Gynecol Cancer. 2003;13: 532-40. [ ] 11. Baker C, Dini SA, Kudrimoti M, et al. Dosimetric evaluation of a newly designed low dose rate brachytherapy applicator for treatment of cervical cancer with extension into the lower vagina. J Appl Clin Med Phys. 2007;8:37-46. [ ] 12. International Commission on Radiation Units and Measurements. Dose and volume specification for reporting intracavitary therapy in gynecology. ICRU Report 38. Bethesda: ICRU; 1985. [ ] 13. Pötter R, Van Limbergen E, Gerstner N, et al. Survey of the use of the ICRU 38 in recording and reporting cervical cancer brachytherapy. Radiother Oncol. 2001;58:11-8. [ ] 14. International Commission on Radiation Units and Measurements. Dose and volume specification for reporting interstitial therapy. ICRU Report 58. Bethesda: ICRU; 1997. [ ] 15. Kazumoto T, Kato S, Tabushi K, et al. High doserate intracavitary brachytherapy for cervical carcinomas with lower vaginal infiltration. Int J Radiat Oncol Biol Phys. 2007;69:1157-66. [ ] Received April 3, 2009. * Study developed at Unit of Radiotherapy, Division of Oncology - Instituto de Radiologia do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554