Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 3 - May / June of 2009
Vol. 42 nº 3 - May / June of 2009
|
ICONOGRAPHIC ESSAY
|
|
Magnetic resonance imaging in lower urinary tract endometriosis: iconographic essay |
|
|
Autho(rs): Cláudio Márcio Amaral de Oliveira Lima, Elisa Pompeu Dias Coutinho, Érica Barreiros Ribeiro, Marisa Nassar Aidar Domingues, Flávia Pegado Junqueira, Antonio Carlos Coutinho Junior |
|
|
Keywords: Magnetic resonance imaging, Endometriosis, Infertility, Genitourinary tract, Bladder, Urethra |
|
|
Abstract:
IMD, Radiologist, Trainee at Clínicas de Diagnóstico Por Imagem (CDPI) and Multi-Imagem, Radiologist at Hospital Naval Marcílio Dias (HNMD), Rio de Janeiro, RJ, Brazil
INTRODUCTION Although most expansive lesions correspond to epithelial neoplasms, there are some non neoplastic diseases such as endometriosis that may progress with focal or diffuse parietal thickening of the bladder wall, simulating malignancy(1). Endometriosis is defined as the presence of functional endometrial tissue outside the endometrial cavity and myometrium(2-4). It is a frequent multifactorial disease, affecting from 7% to 10% of the general population. Genitourinary involvement is observed in 1% to 3% of cases, most frequently in women between 25 and 40 years of age(5). Deep endometriosis is a specific entity, histologically defined as invasion of the peritoneum by ectopic foci at a depth of > 5 mm, generally involving uterosacral ligaments, bowel, rectovaginal septum, and the urinary tract(6). The clinical diagnosis is difficult and based on history, physical examination, laparoscopy and biopsy of suspicious lesions(6,7). Magnetic resonance imaging (MRI) is a noninvasive method that allows multiplanar evaluations, with high spatial resolution and tissue characterization capacity, without use of ionizing radiation or iodinated contrast agents. MRI presents high accuracy for the diagnosis of vesical lesions, with higher sensitivity than transvaginal ultrasonography in demonstrating the involvement of the bladder muscular layer and defining the relation of the lesion and the adjacent structures in the surgical planning(8). The present iconographic essay aims to demonstrate the main MRI findings in the involvement of the lower urinary tract by deep endometriosis.
MRI PROTOCOLS Specific protocols must be followed for MRI acquisition to evaluate patients under suspicion of endometriosis in the lower urinary tract. At the "Clínicas de Diagnóstico Por Imagem e Multi-Imagem" the examination is performed during the menstrual period because of the higher likelihood of identifying hemorrhage foci, thus facilitating the tissue characterization of such lesions. Moderate bladder repletion is required, considering that the identification of small lesions becomes more difficult with a completely distended or empty bladder. Additionally, immediately before the examination, a venous antispasmodic agent (butylbromide scopalamine) is administered. Most recently the vaginal (50 ml) aqueous gel and rectal (250 ml) saline solution introduction has been adopted to facilitate the identification of other foci of deep endometriosis, particularly in the retrocervical region, uterosacral ligaments and rectal walls, in a possible association. The introduction of vaginal aqueous gel and rectal saline solution does not cause any considerable discomfort or pain for the patients, in spite of the menstrual period. No bowel preparation was required. The imaging protocol icludes the following sequences: T1-weighted (TR: 589; TE: 10; FOV: 240; slice thickness: 3 mm; interval: 10%; matrix: 256 × 256) in the axial plane, T1-weighted with fat suppression (TR: 706; TE: 14; FOV: 250; slice thickness: 5 mm; interval: 45%; matrix: 230 × 256) in the sagittal and axial planes, T2-weighted (TR: 3610; TE: 108; FOV: 240; slice thickness: 3.5 mm; interval: 10%; matrix: 384 × 326) in the sagittal, coronal and axial planes. After intravenous gadolinium injection, T1-weighted sequences with fat suppression are performed in the sagittal and axial planes. Contrast agent injection may be useful in the detection of lesions on the abdominal wall, since peritoneal/serous surfaces surrounding foci of deep endometriosis can enhance(8) most probably because of the intense inflammatory process associated with endometriosis. In cases of ureteral involvement, uro-resonance techniques may be utilized for a better anatomical characterization of ureterohydronephrosis as a result of the larger field of view and urographic effect.
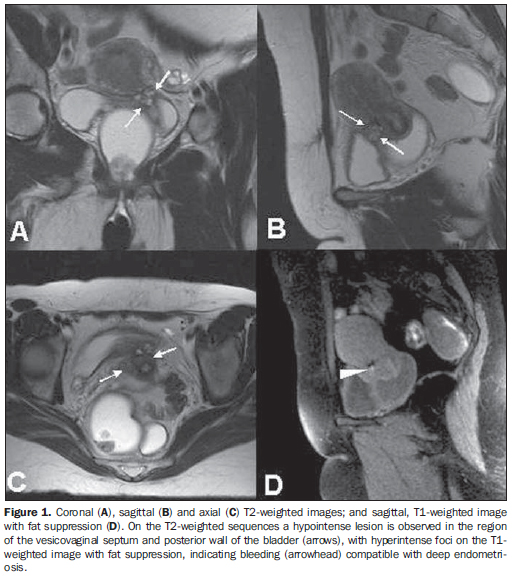
MRI FINDINGS The involvement of the vesicouterine space is demonstrated as nodular formations with low signal on T2- weighted sequences, generally attached to the anterior uterine surface, forming an obtuse angle with the bladder wall(4,5) (Figure 1).
Vesical endometriosis may be of an intrinsic nature, primarily involving musculature (detrusor), or extrinsic, when lesions in the vesicouterine space involving the serous/peritoneal surfaces infiltrate the vesical walls. A predominantly hypointense, diffuse or focal thickening of the vesical wall related to the fibrotic component may be observed on T2-weighted sequences, substituting the characteristic signal of the detrusor musculature. Eventually, intermingled, hyperintense foci may be observed on T2-weighted sequences, corresponding to ectatic endometrial glands with or without hematic contents(5,6) (Figure 2). Bladder mucosa invasion is not frequent in cases of vesical endometriosis, and MRI can demonstrate alteration even in asymptomatic patients with normal cystoscopy(9). MRI plays a significant role in the diagnosis of vesical endometriosis (88% sensitivity, 98.9% specificity, 88% positive predictive value, 98.9% negative predictive value, and 97.9% accuracy), particularly for allowing the identification of submucosal lesions, even in cases with normal cystoscopy and associations with other subperitoneal foci and /or intermingled with extensive adhesions(2). In accordance with the literature, in the present essay a highly variable signal intensity was observed with a high frequency of hemorrhagic foci intermingled with these lesions, probably because these examinations were performed during the menstrual period, and also for the remarkable predilection for the posterior vesical wall and dome. In endometriosis, ureteral as well as vesical involvement may be of intrinsic or extrinsic nature, the latter being four times more frequent. In the intrinsic disease, the ectopic endometrial tissue directly infiltrates the bladder muscular layer, the lamina propria or the ureteral lumen, and is probably originated by venous or lymphatic dissemination. In case of extrinsic involvement, the endometrial tissue invades only the ureteral adventitia or the adjacent connective tissue and probably originates from ovary, broad ligament or uterosacral involvement. The presence of fibrotic/cicatricial tissue without a true endometriotic involvement of the ureter may also be classified as extrinsic involvement(5,6). Frequently, endometriosis involves the pelvic ureter (Figure 3). Most affected women are in the premenopausal period(5,6). Ureteral obstruction (Figure 4) may be slow and progressive, eventually causing renal failure(10). Intrinsic involvement of the ureter is rare, with periureteral fibrosis, either in association or not with bleeding foci, being the most frequent finding. Urethral involvement is rare, usually with periurethral lesion simulating diverticula (Figure 5), either with hematic contents or not(10). Many times, foci of deep endometriosis are simultaneously observed in different sites, among them the retrocervical region, the uterosacral ligaments, the rectovaginal and vesicovaginal septa and other hollow viscus(4-6) (Figure 6). The gold standard for management of endometriosis is complete resection of these lesions. Therefore, the preoperative evaluation plays a relevant role, generally being limited to clinical and sonographic data(6,7). MRI plays a relevant role in the diagnosis of lower urinary tract endometriosis, with high sensitivity, specificity, accuracy and positive predictive value, mainly for allowing the identification of subperitoneal lesions and/or lesions intermingled with extensive adhesions, besides demonstrating and evaluating the extent of subperitoneal and/or visceral lesions that cannot be visualized at laparoscopy and/or cystoscopy. Acknowledgements To Dr. Romeu Côrtes Domingues, for encouragement and for making this and other scientific studies possible, and to Dr. Emerson L. Gasparetto, for his valuable help.
REFERENCES 1. Wong-You-Cheong JJ, Woodward PJ, Manning MA, et al. From the archives of the AFIP: Inflammatory and nonneoplastic bladder masses: radio-logic-pathologic correlation. Radiographics. 2006;26:1847-68. [ ] 2. Bazot M, Darai E, Hourani R, et al. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology. 2004;232:379-89. [ ] 3. Generao SE, Keene KD, Das S. Endoscopic diagnosis and management of ureteral endometriosis. J Endourol. 2005;19:1177-9. [ ] 4. Coutinho Jr AC, Lima CMAO, Coutinho EPD, et al. Ressonância magnética na endometriose pélvica profunda: ensaio iconográfico. Radiol Bras. 2008;41:129-34. [ ] 5. Deval B, Danoy X, Buy JN, et al. Bladder endometriosis. Apropos of 4 cases and review of the literature. Gynecol Obstet Fertil. 2000;28:385-90. [ ] 6. Comiter CV. Endometriosis of the urinary tract. Urol Clin North Am. 2002;29:625-35. [ ] 7. Woodward PJ, Sohaey R, Mezzetti TP Jr. Endometriosis: radiologic-pathologic correlation. Radiographics. 2001;21:193-216. [ ] 8. Ghattamaneni S, Weston MJ, Spencer JA. Imaging in endometriosis. Imaging. 2007;19:345-68. [ ] 9. Del Frate C, Girometti R, Pittino M, et al. Deep retroperitoneal pelvic endometriosis: MR imaging appearance with laparoscopic correlation. Radiographics. 2006;26:1705-18. [ ] 10. Prasad SR, Menias CO, Narra VR, et al. Cross-sectional imaging of the female urethra: technique and results. Radiographics. 2005;25:749-61. [ ] Received February 14, 2009. * Study developed at Clínicas de Diagnóstico Por Imagem (CDPI) and Multi-Imagem, Rio de Janeiro, RJ, and Centro de Diagnóstico por Imagem Fátima Digittal, Nova Iguaçu, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554