Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 1 - Jan. /Feb. of 2010
Vol. 43 nº 1 - Jan. /Feb. of 2010
|
CASE REPORT
|
|
Giant gastric trichobezoar: a case report and literature review |
|
|
Autho(rs): Rony Klaus Isberner, Carlos Antônio da Silva Couto, Bruno Lorenzo Scolaro, Gustavo Becker Pereira, Renan Oliveira |
|
|
Keywords: Bezoars, Gastric dilatation, Gastric outlet obstruction, Dyspepsia |
|
|
Abstract:
ITitular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Professor in the Discipline of Diagnostic Imaging at Universidade do Vale do Itajaí, Physician at Unit of Diagnostic Imaging - Hospital Maternidade Marieta Konder Bornhausen, Itajaí, SC, Brazil
INTRODUCTION The word "bezoar" corresponds to accumulation of undigestible foreign substances along the digestive tract, most commonly found in the stomach and proximal portions of the small bowel(1,2). Bezoars may present different compositions, although classically the most frequently found forms correspond to trichobezoars (agglomeration of hair) and phytobezoars (agglomeration of vegetable fibers)(1,3,4). The finding of bezoars is associated with patients presenting hypokinetic/hyposecretory gastric conditions, gastric resections and underlying psychiatric disorders, that constitute the main cause for development of trichobezoars resulting from the habit of hair swallowing by young women(1,3,5). Bezoars symptoms are highly variable, depending on their site and size. Trichobezoars, generally confined to the stomach, may cause symptoms resulting from mechanical obstructive processes, parietal compression and, most rarely, gastric wall perforation(1,4). The present report describes the case of a female, 18-year-old patient with a large epigastric mass who was submitted to clinical and imaging investigation and subsequent surgical management.
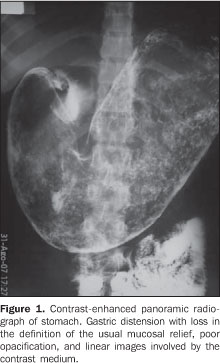
CASE REPORT A.A.S., a female 18-year-old housewife presenting epigastric pain in association with dyspeptic symptoms. No other complaint neither pathological history were reported. The patient reported a normal term delivery one month ago. At clinical examination, the patient presented stable vital signs, with a large (10 × 7.5 cm), hardened and painful epigastric mass at abdominal palpation, with no sign of acute abdomen. Laboratory tests were compatible with normality. The patient was referred to the center of diagnostic imaging, undergoing abdominal sonographic study that demonstrated an echogenic mass in the epigastric region with intense posterior acoustic shadowing. Seriography of the esophagus, stomach and duodenum demonstrated the stomach hyperdistended with heterogeneous material occupying the whole gastric lumen and duodenum. The fist intestinal loops were free (Figure 1).
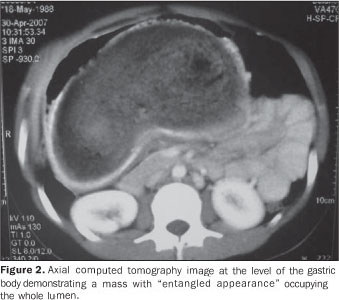
Tomographic sections of the abdomen demonstrated a mass with "entangled appearance" occupying the whole gastric lumen (Figure 2).
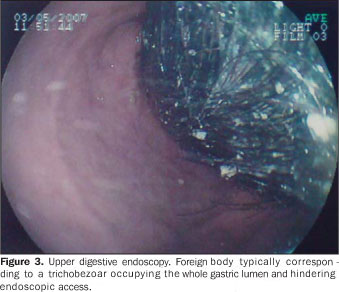
The suspicion of a trichobezoar was confirmed by upper digestive endoscopy that demonstrated the presence of a foreign body described as a "hair bolus" hindering endoscopic access (Figure 3).
Surgical management was indicated once the diagnosis was confirmed. The patient was submitted to laparotomy and gastrotomy for removal of the gastric foreign body, with transoperative finding of a large stomach with intact walls and preserved mucosa. No other abnormality was found in her abdominal cavity. A dark, "J-shaped" specimen with putrid odor and weighing 1950 grams was removed (Figure 4). The patient presented a satisfactory progression and was discharged at the third postoperative day, being referred to the psychiatric ambulatory for follow-up.
DISCUSSION Bezoars were originally described by reports dated 1000 years BC as found in the stomach of mountain goats in the Western region of Persia. At that time, it was commonly believed that bezoars extracted from animals had purifying and healing properties in cases of arsenic poisoning. Bezoars were considered as extremely powerful amulets. Currently, bezoars can be found in the gastrointestinal tract of several ruminants such as sheep, llamas, etc.(1,5). Additionally to the classical trichobezoar (hair bolus) and phytobezoar (concretion of vegetable fibers), bezoars may also present different compositions such as stones, plastic, cotton, medicines (anti-acids) and resin fibers(1,3,4). In the clinical practice, bezoars correspond to rare findings. Trichobezoars incidence is highest in women aged under 30 years, with history of trichophagia present in 50% of cases, generally from early childhood and considered by specialists as a personality disorder analogous to finger nail biting(1). It is known that patients with mild pathological psychiatric symptoms, such as sporadic trichophagia, may present worsening of symptoms as they are submitted to strong emotional burden like during gestation(4). In the present case, the pregnancy may have accelerated the development of the trichobezoar resulting from the trichophagia worsening in association with the gastrointestinal hypomotility that is a typical physiological phenomenon during gestation. Additionally it must be considered that the finding of a palpable mass during the gestation is masked by the large uterine volume. Trichobezoar symptoms depend on the site and size of the mass, besides the degree of functional involvement of the affected segment. Stomach trichobezoars may cause nonspecific dyspeptic symptoms such as post-prandial abdominal pain, nausea and emesis, halitosis, gastrointestinal bleeding, anemia and malnutrition(2,5). Upper digestive endoscopy is the technique of choice for diagnosing gastric bezoars, constituting a therapeutic method in selected cases(1,5). Contrast-enhanced radiography frequently demonstrates a non-adherent, spindle-shaped mass in the stomach, with the contrast mean surrounding, coating and infiltrating the trichobezoar, excluding the diagnosis of neoplasia. However, this method can identify only 25% of bezoars in this topography(5). Computed tomography plays a relevant role in the diagnosis of such cases, demonstrating expansile, concentric and compressive mass in the stomach lumen, filled with air and debris(5). Basically, the treatment consists of surgical resection and recurrence prevention(5). Large trichobezoars require surgical management by means of gastrotomy as the method of choice, always in association with psychiatric follow-up(1,4).
REFERENCES 1. Barbosa AL, Bromberg SH, Amorim FC, et al. Obstrução intestinal por tricobezoar. Relato de caso e revisão da literatura. Rev Bras Coloproct. 1998;18:190-3. [ ] 2. Correa Antúnez MI, Serrano Calle A, Pimentel Leo JJ, et al. Bezoar gástrico. Cir Pediátr. 2001;14:82-4. [ ] 3. Ruiz HD, Palermo M, Ritondale O, et al. Tricobezoares gastroduodenales: una causa poco frecuente de obstrucción del tracto de salida. Acta Gastroenterol Latinoam. 2005;35:24-7. [ ] 4. Contreras-Parada L, Figueroa-Quiñónez J, Rueda-Mendoza S. Presentación de un caso de tricobezoar en el Hospital Erasmo Meoz de la ciudad de San José de Cúcuta (Colombia). Salud Uninorte. 2004;18:46-50. [ ] 5. Ibuowo AA, Saad A, Okonkwo T. Giant gastric trichobezoar in a young female. Int J Surg. 2006;6:e4-e6. [ ] Received April 19, 2008. * Study developed at Hospital Maternidade Marieta Konder Bornhausen, Itajaí, SC, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554