
 |
|
Rony Klaus Isberner, Carlos Antônio da Silva Couto, Bruno Lorenzo Scolaro, Gustavo Becker Pereira, Renan Oliveira
RESUMO
Os autores descrevem um caso de massa abdominal epigástrica palpável associada a sintomas dispépticos em uma paciente jovem sem antecedentes patológicos. Estudos por imagem evidenciaram corpo estranho gástrico de "aspecto enovelado". A paciente foi submetida a gastrotomia via laparotomia, com retirada de um tricobezoar de 1.950 gramas.
Palavras-chave: Bezoares, Dilatação gástrica, Obstrução da saída gástrica, Dispepsia
ABSTRACT
The authors describe the case of a palpable epigastric mass associated with dyspeptic symptoms in a young female patient with no previous pathologic history. Imaging studies demonstrated the presence of a gastric foreign body with an "entangled appearance". The patient underwent laparotomy and gastrotomy for removal of a trichobezoar weighing 1,950 grams.
Keywords: Bezoars, Gastric dilatation, Gastric outlet obstruction, Dyspepsia
VMédico Residente do Serviço de Cirurgia Geral do Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brasil
INTRODUÇÃO
O termo bezoar refere-se ao acúmulo de substâncias estranhas indigeríveis ao longo do tubo digestivo, mais comumente encontradas no estômago e porções proximais do delgado(1,2). Podem apresentar diversas composições, porém as mais conhecidas, classicamente, correspondem ao tricobezoar (aglomerado de cabelos) e ao fitobezoar (aglomerado de fibras vegetais)(1,3,4).
Estão associados a pacientes com afecções gástricas hipocinéticas-hipossecretoras, ressecções gástricas e distúrbios psiquiátricos, principal causa de formação dos tricobezoares devido à ingestão do próprio cabelo por mulheres jovens(1,3,5).
Os sintomas dos bezoares são muito variáveis e dependem de sua localização e tamanho. Os tricobezoares, geralmente confinados ao estômago, podem gerar sintomas resultantes de processos obstrutivos mecânicos, da compressão parietal e, mais raramente, da perfuração da parede gástrica(1,4).
Neste relato apresentamos o caso de uma paciente de 18 anos de idade com volumosa massa epigástrica submetida a investigação clínico-imaginológica e tratamento cirúrgico.
RELATO DO CASO
A.A.S., sexo feminino, 18 anos de idade, apresentando dor epigástrica e sintomas dispépticos. Sem outras queixas ou antecedentes patológicos. Referia parto normal há um mês. Ao exame físico apresentava sinais vitais estáveis. No exame abdominal evidenciou-se massa na região epigástrica, de grandes dimensões (10 × 7,5 cm), endurecida, homogênea e dolorosa à palpação, sem sinais de abdome agudo. Exames laboratoriais compatíveis com a normalidade.
A paciente foi encaminhada ao centro de diagnóstico por imagem, onde foi submetida a exame ultrassonográfico de abdome, que demonstrou uma formação ecogênica localizada na região epigástrica com intensa produção de sombra acústica posterior.
Foi realizada seriografia esôfago-estômago-duodeno, que evidenciou estômago hiperdistendido contendo material heterogêneo ocupando todo o lúmen gástrico, e duodeno e primeiras alças intestinais livres (Figura 1).

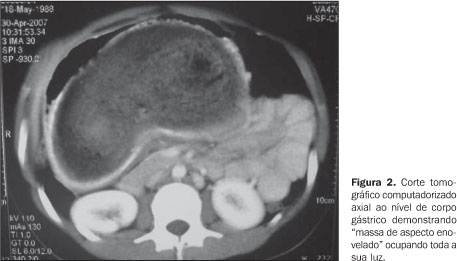
Cortes tomográficos abdominais demonstraram "massa de aspecto enovelado" ocupando toda a luz gástrica (Figura 2).
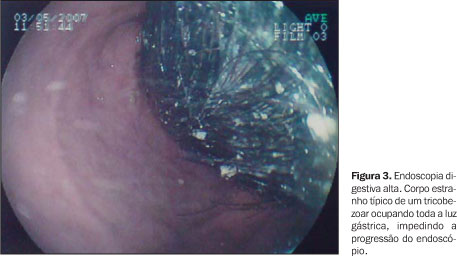
A suspeita de tricobezoar foi confirmada por endoscopia digestiva alta, que constatou a presença de corpo estranho descrito como "bolo de cabelo" impedindo a progressão do endoscópio (Figura 3).
Após diagnóstico firmado, foi indicado tratamento cirúrgico. A paciente foi submetida a laparotomia seguida de gastrotomia para retirada de corpo estranho gástrico. Durante o transoperatório evidenciou-se estômago com grandes dimensões, paredes íntegras e mucosa preservada. Cavidade abdominal sem outros achados anormais. Retirada peça escura, de odor pútrido, em forma de "J" e pesando 1.950 gramas (Figura 4). A paciente apresentou boa evolução, recebendo alta no terceiro dia pós-operatório, sendo encaminhada ao ambulatório de psiquiatria para acompanhamento.

DISCUSSÃO
Os bezoares foram originalmente descritos em relatos datados de 1000 anos a.C., quando encontrados em estômagos de cabras da montanha ao oeste da Pérsia. Era comum, na época, o uso dos bezoares retirados dos animais para "purificar" bebidas e "curar" envenenamentos por arsênico. Sua posse era tida como amuleto de grande poder. Atualmente, podem ser encontrados no trato gastrintestinal de diversos animais ruminantes como ovelhas, lhamas, etc.(1,5).
Além dos clássicos tricobezoar (aglomerado de cabelos) e fitobezoar (aglomerados de fibras), os bezoares podem ainda apresentar diversas composições como pedras, plástico, algodão, medicamentos (antiácidos) e resina(1,3,4).
Na prática médica correspondem a achados raros. A incidência dos tricobezoares é maior em mulheres jovens com menos de 30 anos, nas quais a história de tricofagia está presente em 50% dos casos, sendo geralmente uma condição iniciada na infância, encarada por especialistas como distúrbio de personalidade análogo ao hábito de roer unhas(1). Sabe-se que pacientes com leves condutas psiquiátricas patológicas, como tricofagia esporádica, podem ter seus sintomas agravados quando submetidas a fortes cargas emocionais, como ocorre durante uma gestação(4). No caso de nossa paciente, a gravidez pode ter acelerado a formação do tricobezoar devido ao agravo da tricofagia associada à hipomotilidade gastrintestinal característica da fisiologia gestacional, além da gestação mascarar o achado da massa palpável em epigástrico por causa do grande volume uterino.
Os sintomas dos tricobezoares dependem de sua localização, do seu tamanho e do grau de comprometimento funcional do segmento afetado. Quando localizados no estômago, podem causar sintomas dispépticos inespecíficos como dor abdominal pós-prandial, náuseas e vômitos, halitose, sangramento gastrintestinal, anemia e desnutrição(2,5).
A endoscopia digestiva alta corresponde à técnica de escolha para o diagnóstico dos bezoares gástricos e constitui um método terapêutico em casos selecionados(1,5). A radiografia contrastada frequentemente mostra massa não aderente ao estômago e fusiforme, sendo que o contraste circunda, reveste e infiltra o tricobezoar, excluindo o diagnóstico de neoplasia. Porém, esse método identifica somente 25% dos bezoares nessa localização(5). A tomografia computadorizada possuiu papel importante no diagnóstico nestes casos, evidenciando formação expansiva na luz do estômago, concêntrica e compressiva, com ar e débris em seu interior(5).
A base do tratamento consiste na retirada do bezoar e prevenção de sua recorrência(5). Para tricobezoares volumosos, o tratamento cirúrgico via gastrotomia é o método de eleição, sempre acompanhado de seguimento psiquiátrico(1,4).
REFERÊNCIAS
1. Barbosa AL, Bromberg SH, Amorim FC, et al. Obstrução intestinal por tricobezoar. Relato de caso e revisão da literatura. Rev Bras Coloproct. 1998;18:190-3. [ ]
2. Correa Antúnez MI, Serrano Calle A, Pimentel Leo JJ, et al. Bezoar gástrico. Cir Pediátr. 2001;14:82-4. [ ]
3. Ruiz HD, Palermo M, Ritondale O, et al. Tricobezoares gastroduodenales: una causa poco frecuente de obstrucción del tracto de salida. Acta Gastroenterol Latinoam. 2005;35:24-7. [ ]
4. Contreras-Parada L, Figueroa-Quiñónez J, Rueda-Mendoza S. Presentación de un caso de tricobezoar en el Hospital Erasmo Meoz de la ciudad de San José de Cúcuta (Colombia). Salud Uninorte. 2004;18:46-50. [ ]
5. Ibuowo AA, Saad A, Okonkwo T. Giant gastric trichobezoar in a young female. Int J Surg. 2006;6:e4-e6. [ ]
 Endereço para correspondência:
Endereço para correspondência:
Dr. Renan Oliveira
Rua Frederico Lubke, 161, Velha
Blumenau, SC, Brasil, 88036-418
E-mail: specialize_@hotmail.com
Recebido para publicação em 19/4/2008.
Aceito, após revisão, em 4/7/2008.
* Trabalho realizado no Hospital Maternidade Marieta Konder Bornhausen, Itajaí, SC, Brasil.
