Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 3 - May / June of 2008
Vol. 41 nº 3 - May / June of 2008
|
ICONOGRAPHIC ESSAY
|
|
Imaging of growth plate injuries |
|
|
Autho(rs): Matiko Yanaguizawa, Gustavo Sobreira Taberner, André Yui Aihara, Cláudia Kazue Yamaguchi, Maria Carolina Guimarães, André Rosenfeld, João Luiz Fernandes, Artur da Rocha Corrêa Fernandes |
|
|
Keywords: Growth plate, Fracture, Physeal bar, Bone bridge, Magnetic resonance imaging, Radiography, Computed tomography |
|
|
Abstract:
ICourse of Specialization in Musculoskeletal Radiology, MDs, Radiologists at Diagnósticos da América, São Paulo, SP, Collaborators at Department of Imaging Diagnosis - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil
INTRODUCTION The structures responsible for the bone growth include the physis (growth plate) and epiphysis. By means of the endochondral ossification process, the cartilaginous structures of these regions are responsible for both the longitudinal growth and shape of the bone(1). Several pathological conditions affecting patients with an immature skeleton may involve the physis and epiphysis, causing complications such as growth arrest, limb shortening, development of bone bridges and angular deformities(1). Acute traumatic conditions, many times resulting in fracture, represent the primary cause for physeal injuries in children. Other conditions may affect the physis, as follows: repetitive stress injuries, infections, tumors, metabolic diseases, thermal and radiation injuries, etc.(1). The assessment of these patients by means of currently available imaging methods is indispensable and well established. Radiography, computed tomography (CT) and magnetic resonance imaging (MRI) are essential for this evaluation, considering that they allow the early diagnosis of the involvement of structures responsible for the bone growth, besides its extent and severity. All these factors are essential for an appropriate management and follow-up, minimizing or even preventing the onset of complications(2).
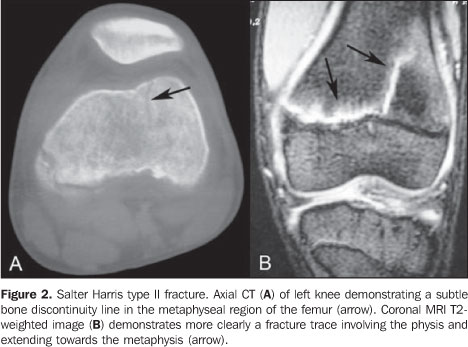
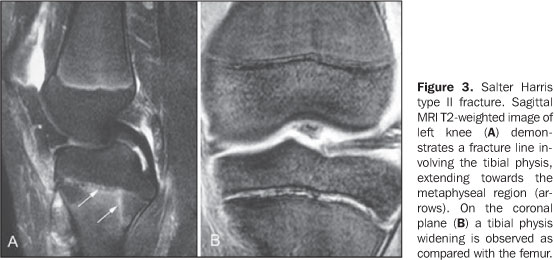
TRAUMATIC EPIPHYSEAL INJURIES Epiphyseal fractures play a relevant role in the context of traumatic injuries, considering that they correspond to approximately 15% of all fractures occurring in children(3). The system most widely accepted for classifying these fractures has been proposed by Salter and Harris, describing five classical types of fractures, the SH II type being the most frequent of them(4). Methods for imaging diagnosis represent essential elements in the evaluation of these patients, considering their capacity of providing relevant information such as type of fracture, localization and degree of physeal involvement, besides detecting the presence of bone bridge(5). Although radiography allows a reasonable evaluation of epiphyseal fractures and is the initial method for evaluation, additional imaging studies may be requested. CT is useful for evaluating the alignment of joint surfaces and presence of bone bridges(2). MRI (Figures 1, 2 and 3) presents advantages such as identification of occult fractures and better definition of the fracture extent, besides the capacity of demonstrating associated alterations such as ligamentous lesions(2).
The involvement of children and adolescents in sports practices is increasingly frequent. Many of these youngsters initiate their practice at a very early age, and the longer duration and higher intensity of training may result in an overload of a still immature skeleton(1). The physeal overload changes the metaphyseal perfusion and affects the chondrocytes mineralization. Initially, a physeal widening occurs and, with the persistence of the ischemic insult, irregularity of the epiphyseal and metaphyseal margins is observed. These alterations may be focal or involve the whole physis(1). Physeal injuries of the distal portion of the radius in young gymnasts(6) (Figure 4), femur in runners, and proximal portions of the humerus in baseball pitchers have been described among repetitive stress injuries(1).
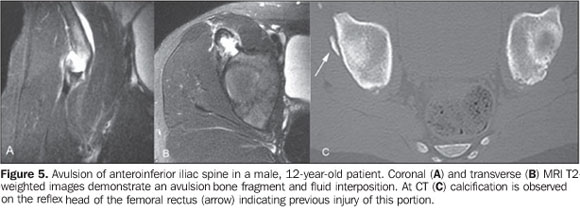
TRAUMATIC APOPHYSEAL INJURIES There are two types of epiphyses: traction epiphysis and pressure epiphysis, each of them with their respective physes. Traction epiphyses, also called apophyses, are ossification centers at the site of tendinous insertion, whereas the pressure epiphyses are localized at long bones ends and are responsible for the longitudinal bone s growth(1). Acute (avulsion) or chronic injuries affecting the apophysis also may occur and are not typically associated with alteration in the longitudinal bone growth. Most frequently, acute traumatic injuries in children and adolescents usually affect the apophyses (Figure 5), because of their highest fragility; on the other hand, in adults, myotendinous junctions are preferably affected(7).
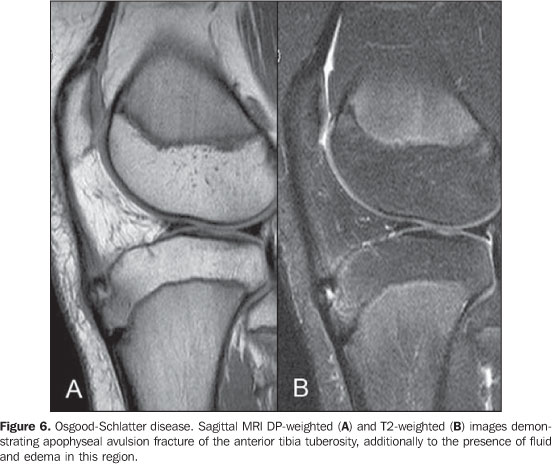
Overload-related conditions such as Osgood-Schlatter disease (Figure 6) and Sever disease frequently occur in young athletes may be a source of discomfort, besides causing interruption of physical activities(1).
FEMORAL HEAD EPIPHYSIOLYSIS Slipped capital femoral epiphysis is the most frequent hip abnormality in adolescents and, in the absence of appropriate management, may result in chronic pain and early osteoarthrosis. It is characterized by the inferior and posterior displacement of the femoral head in relation to the metaphysis(8). The typical patient is a generally overweight adolescent presenting with claudication, attitude in external rotation of the affected lower limb, and pain, usually in the inguinal region or hip, sometimes irradiating to the anteromedial portion of the hip and knee. Evaluation of the contralateral side is important, considering that bilateral involvement is reported in up to about 50% of cases(9). The clinical diagnosis requires confirmation by imaging methods demonstrating displacement of the femoral head epiphysis (Figure 7). Radiography is the method for initial evaluation. On the anteroposterior view, the Klein line can be drawn along the lateral neck of the proximal femur which, in normal hips, passes through a portion of the femoral head. The true lateral view of the hip may be useful in cases of low slip severity, with predominance of posterior displacement. CT can be utilized for determining the degree of displacement, and MRI, despite its low utility in the diagnosis and management of epiphysiolysis, is useful in the evaluation of femoral head chondrolysis or osteonecrosis, both possible complications(9).
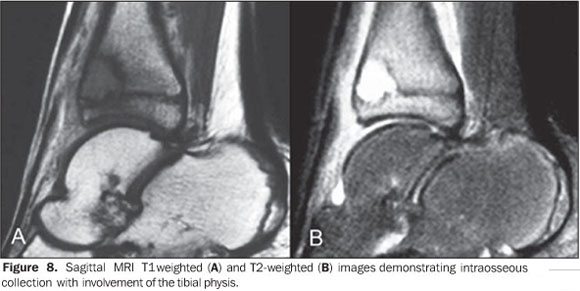
INFECTION In children with less than 18 months of age, blood vessels pass through the growth plate nourishing the epiphysis that is the most frequent site of infection in this age group. Above this age, the number of vessels passing through the physis decrease, and the metaphysis becomes the most frequent site of infection. The degree of growth disturbance is directly related to the area and site of physeal destruction, the amount of destructed cartilage, and extent of injury of the chondroepiphyseal vascular system(10). Radiography may demonstrate bone alterations associated with osteomyelitis (changes in the bone texture, periosteal reaction, enlargement of adjacent soft tissues), besides physeal widening. CT can demonstrate the presence of abscesses, being particularly useful in the detection of sequestra, while MRI presents a high sensitivity and specificity for detecting physeal involvement(10) (Figure 8).
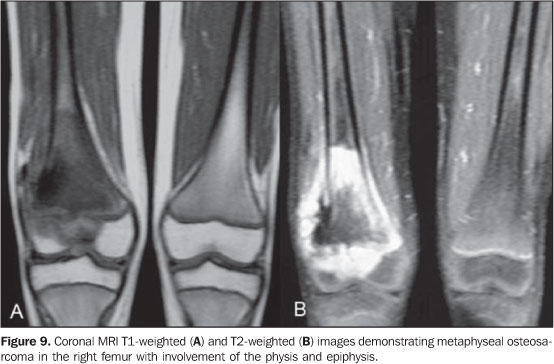
TUMORS Many benign tumors, such as simple bone cyst, endochondroma, chondroblastoma(11), osteoid osteoma, aneurysmal bone cyst, chondromyxoid fibroma and fibrous dysplasia may occur near the physis. Physeal injury may occur because of the presence of the injury itself, or during surgical procedures including curettage of bone graft implantation(12). Although it was believed that the physis could act as a natural barrier to malignant primary bone tumors such as osteosarcomas and Ewing´s sarcoma, it has been already established that its involvement may occur, affecting the epiphysis and the adjacent joint(13). The detection of epiphyseal and joint involvement is essential in the surgical planning, considering that, with the development of neoadjuvant chemotherapic drugs, the epiphyseal preservation results in a better recovery, with consequential better residual functioning of the limb(14). MRI can demonstrate the physeal and epiphyseal involvement (Figure 9), with higher specificity and utility on coronal and sagittal T1-wieghted images. STIR-weighted sequences demonstrate peritumoral edematous alterations and eventual residual foci of red bone marrow(13).
METABOLIC DISEASES Amongst the metabolic diseases involving the physis, rickets is the most widely known. Rickets is a disease caused by deficiency of, or resistance to vitamin D and its derivatives. Endochondral ossification, a process involving chondrocytes hypertrophy and death, cartilaginous matrix mineralization, and cartilage invasion by metaphyseal blood vessels, depends on the normal metabolism of this vitamin. In cases where this metabolism is affected, an abnormal mineralization of the physeal cartilage is observed, with persistence of this cartilage in the metaphyseal region(15). Radiography and MRI findings reflect the hystopathology of the junction between the physeal cartilage and the metaphyseal bone presents as a physeal widening. As the disease progresses, the metaphysis, as well as the adjacent epiphyseal margins, becomes irregular (Figure 10). Although MRI is not necessary in the diagnosis and follow-up of rickets, and aiming at avoiding confusion with other metaepiphyseal bone diseases, it is important to know the main features of this disease demonstrated by this method: physeal widening with high signal intensity on T2-weighted sequences, absence of a transitory calcification zone and similar alterations on the periphery of the adjacent ossification center(15).
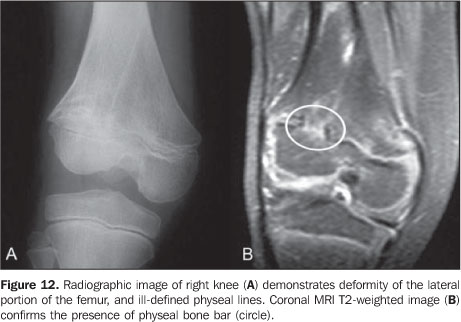
COMPLICATIONS Growth plate injury may result in the development of a (bone or fibrotic) bar. Depending on the size and localization, the growth may become slower or even be arrested, resulting in discrepancies between the limbs length and angular deformities. The early diagnosis, localization and the size of the physeal bar represent relevant factors in the prognosis and indication for surgical management(16). The most frequent cause is related to epiphyseal fractures, but the physeal bar may result from infection, iatrogenic lesion, tumor invasion, thermal injuries (Figure 11), among other causes(3).
Radiography can demonstrate the bone bridge as foci of osteocondensation of with a starry appearance or even bone structures in the metaphyseal interface. Also, radiography may raise the suspicion for this complication based on indirect findings such as angular deformities and illdefined physeal lines (Figure 12), unfortunately, relatively late findings(17).
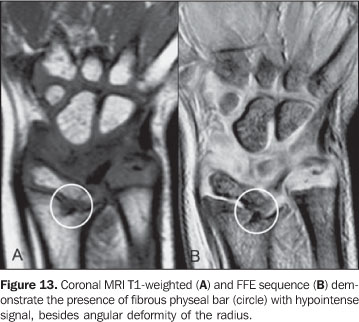
CT also allows evaluating the interface between the metaphysis and epiphysis, demonstrating the localization and dimension of the bone bridges. Coronal, sagittal and 3D reconstructions are quite useful in the preoperative planning(17). Currently, MRI is the most sensitive method for its detection, particularly in the case of fibrovascularized, still non-ossified tissues (Figure 13)(16).
CONCLUSIONS Amongst the different conditions involving the growth plate, traumatic injuries resulting in epiphyseal fractures are the most frequent ones. The possibility of a determined injury progressing to complications such as physeal bone bar development, bone shortening or angular deformities depends on several factors like patient´s age, localization and extent of the physeal injury, and intensity of the trauma. Depending on the disease involved, the different imaging diagnosis methods represent indispensable tools in the evaluation of these patients, considering their capacity of providing relevant information for an early diagnosis and appropriate therapy planning, so reducing the probability of complications development. Radiography should be the initial method for evaluation, providing relevant diagnostic information in the majority of cases. CT is useful for evaluating complex fractures and detecting physeal bone bars. MRI plays a significant role in the evaluation of tumor-like lesions and physeal bone bars.
REFERENCES 1. Caine D, DiFiori J, Maffulli N. Physeal injuries in children's and youth sports: reasons for concern? Br J Sports Med. 2006;40:749-60. [ ] 2. Carey J, Spence L, Blickman H, et al. MRI of pediatric growth plate injury: correlation with plain film radiographs and clinical outcome. Skeletal Radiol. 1998;27:250-5. [ ] 3. Rogers LF, Poznanski AK. Imaging of epiphyseal injuries. Radiology. 1994;191:297-308. [ ] 4. Nanni M, Butt S, Mansour R, et al. Stress-induced Salter Harris I growth plate injury of the proximal tibia: first report. Skeletal Radiol. 2005;34: 405-10. [ ] 5. Kodron AEV, Hernandez AJ, Costa AJF, et al. Importância da ressonância magnética na avaliação das lesões traumáticas da placa de crescimento epifisária. Rev Bras Ortop. 1996;31:435-40. [ ] 6. DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34: 840-9. [ ] 7. Stevens MA, El-Khoury GY, Kathol MH, et al. Imaging features of avulsion injuries. Radiographics. 1999;19:655-72. [ ] 8. Boles CA, El-Khoury GY. Slipped capital femoral epiphysis. Radiographics. 1997;17:809-23. [ ] 9. Umans H, Liebling MS, Moy L, et al. Slipped capital femoral epiphysis: a physeal lesion diagnosed by MRI, with radiographic and CT correlation. Skeletal Radiol. 1998;27:139-44. [ ] 10. Marin C, Sanchez-Alegre ML, Gallego C, et al. Magnetic resonance imaging of osteoarticular infections in children. Curr Probl Diagn Radiol. 2004;33:43-59. [ ] 11. Souza FF, Rodrigues MB. Qual o seu diagnóstico? Radiol Bras. 2006;39(3):v-vi. [ ] 12. Panuel M, Gentet JC, Scheiner C, et al. Physeal and epiphyseal extent of primary malignant bone tumors in childhood. Correlation of preoperative MRI and the pathologic examination. Pediatr Radiol. 1993;23:421-4. [ ] 13. Jesus-Garcia R, Seixas MT, Costa SR, et al. Invasão da placa epifisária pelo osteossarcoma. É a placa uma barreira ao crescimento do tumor? Rev Bras Ortop. 1997;32:870-4. [ ] 14. Hoffer FA, Nikanorov AY, Reddick WE, et al. Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol. 2000; 30:289-98. [ ] 15. Ecklund K, Doria AS, Jaramillo D. Rickets on MR images. Pediatr Radiol. 1999;29:673-5. [ ] 16. Lohman M, Kivisaari A, Vehmas T, et al. MRI in the assessment of growth arrest. Pediatr Radiol. 2002;32:41-5. [ ] 17. Lourenço RB, Rodrigues MB. Qual o seu diagnóstico? Radiol Bras. 2006;39(4):v-vi. [ ] Received July 16, 2007. Accepted after revision February 14, 2008. * Study developed at Diagnósticos da América, São Paulo, SP, and Department of Imaging Diagnosis - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554