Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 3 - May / June of 2008
Vol. 41 nº 3 - May / June of 2008
|
ORIGINAL ARTICLE
|
|
Computed tomography assessment of the ethmoid roof: a relevant region at risk in endoscopic sinus surgery |
|
|
Autho(rs): Soraia Ale Souza, Marcia Maria Ale de Souza, Marcos Idagawa, Ângela Maria Borri Wolosker, Sérgio Aron Ajzen |
|
|
Keywords: Anatomy, Nose, Nasal cavity, Computed tomography, Fovea ethmoidalis, Olfactory fossa |
|
|
Abstract:
IMaster, Student of the Doctorate Program at Department of Imaging Diagnosis - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil
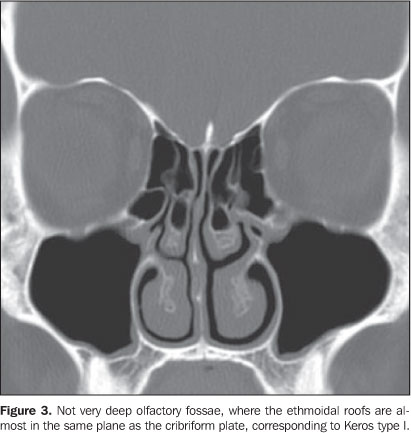
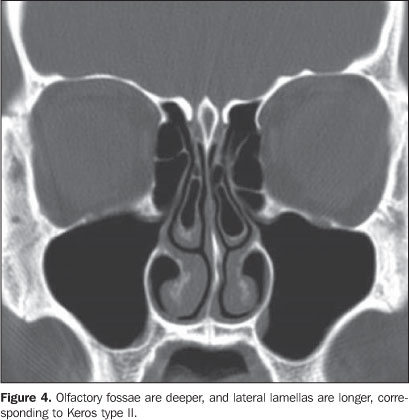
INTRODUCTION Currently, endoscopic frontal sinuses surgery is considered as the treatment of choice for chronic rhinosinusitis resistant to clinical management, as well as for approaching a number of conditions such as mucocele, choanal atresia, nasal polyposis, sellar and parasellar tumors, optic nerve decompression, management of epistaxis and epiphora caused by lower lacrimal ducts obstruction(1). Although the incidence of intraoperative complications is low, severe complications such as intraorbital hematomas with visual loss, liquoric fistula and intracranial penetration may occur(2,3). Most of major complications are related to surgical manipulation of the ethmoidal and frontal sinuses(3,4). The roof of the ethmoidal labyrinth is formed by the fovea ethmoidalis, an extension of the frontal bone orbital plate, primarily separating the ethmoidal cells from the anterior cranial fossa(59). Medially, the fovea ethmoidalis attaches to the lateral lamella of the cribriform plate, that is part of the ethmoid bone, corresponding to a very thin bone structure, much thicker than the fovea ethmoidalis(5,8-10), offering lower resistance to perforation during surgical maneuvers. The depth of the olfactory fossa is determined by the height of the lateral lamella of the cribriform plate. In 1962, Keros(11) defined three heights (Figure 1) and classified the depth of the olfactory fossa into Keros type I (< 3 mm), type II (4-7 mm) and type III (8-16 mm). Depending on the Keros type, a variable segment of the lateral wall of the olfactory fossa will be exposed during the dissection of the frontoethmoidal region. The Keros type III is the most vulnerable one, considering the major risk for iatrogenic lesion of the lateral lamella of the cribriform plate(6,8,9,12). Several studies(4,6,8-19) highlight the relevance of the evaluation of the ethmoidal roof and its value in the prevention of endoscopic surgery complications. According to the literature, in the skull base, iatrogenic lesions occur predominantly in the lateral lamella of the cribriform plate. The site where the anterior ethmoidal artery penetrates the cranial fossa is particularly interesting, considering that this is the thinnest and less resistant region of the whole skull base(6,8-10). The ethmoid roof configuration may present asymmetry in the height and angulation between sides in a same individual(6,10-13). Some studies have demonstrated that the lateral lamella of the cribriform plate is symmetrical in less than 50% of individuals, and that this asymmetry is related to flattening of the fovea ethmoidalis with angulation of the lateral lamella of the cribriform plate, which may result in surgical difficulties(20,21). The knowledge about the complex skull base anatomy and anatomical relations, including the fovea ethmoidalis and lateral lamella of the cribriform plate, is essential in the prevention of complications in endoscopic nasal surgeries(3,6-8,21). Computed tomography (CT) has contributed not only to the evaluation of sinonasal diseases, but also to the characterization of the paranasal sinuses anatomy(21-25). Coronal images can particularly be considered as maps in the evaluation of the anatomy that is highly variable even between the two sides of a same individual, demonstrating areas potentially at risk for complications in the planning of endoscopic nasal surgeries(12,14,17,19,20-32). The reasoning for the choice of this theme is associated with the evaluation of anatomical findings that may determine a higher intraoperative safety during surgeries in the frontoethmoidal region, giving the surgeon previous knowledge about the configuration of the ethmoidal roof and depth of olfactory fossae, consequently reducing the patient exposure to potential complications.
MATERIALS AND METHODS Retrospective analysis of 200 CT images of frontal sinuses acquired in the period between August and December 2006, in the São Paulo, SP, metro region. The following exclusion criteria were adopted: patients under the age of ten, previous history of surgery or trauma in the paranasal sinuses or skull base, congenital abnormalities of the face, malignant disease of the frontal sinus, osteofibrotic lesions and sinusopathy determining opacification of the frontal recess and/or anterior ethmoid cells. In the above mentioned period, 540 CT images of frontal sinuses were evaluated, and 340 of them were excluded according to the already described exclusion criteria. All of the CT images were acquired in a helical Hi-Speed tomograph (GE Medical Systems; Milwaukee, USA). Only coronal images were utilized in the present study. These images were acquired perpendicularly to the hard palate, from the anterior margin of the frontal sinus to the anterior margin of the clivus, with the patient positioned in ventral decubitus. Technical parameters adopted for acquisition and analysis of tomographic images are shown on Chart 1.
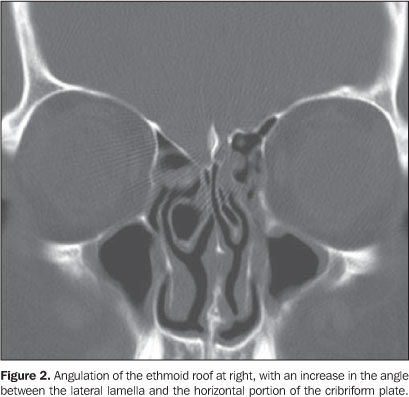
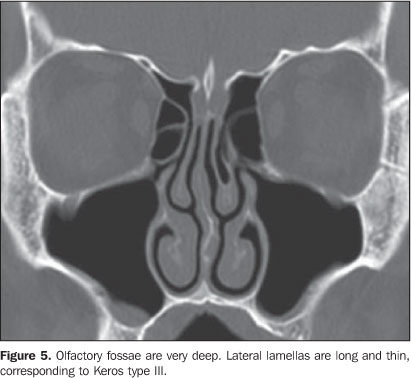
The CT studies interpretation involved morphological analysis of the ethmoid sinus roof as regards symmetry in height and presence of angulation of the lateral lamella of the cribriform plate. Angulation corresponded to the presence of an increase in the angle formed between the lateral lamella and the horizontal portion of the cribriform plate (Figure 2). The depth of the olfactory fossa was determined by the length of the highest lateral lamella and classified into types I, II or III, according to the Keros criteria (Figures 3, 4 and 5).
RESULTS The sample of this study included 200 patients (83 [41.5%] men and 117 [58.5%] women) with ages ranging between 12 and 88 years (mean = 34.33 years). Table 1 shows the distribution of depths of olfactory fossae according to the Keros classification. Only one patient was found with Keros type III anatomical variation, with the greatest majority of patients being classified as Keros type II.
In the majority of CT studies (88%) symmetry was observed in the height of the lateral lamellas between left and right sides in a same individual. In cases where asymmetry was observed, 5.5% (11 CT studies) presented a lower lateral lamella at left, and 6.5% (13 studies), at right. Table 2 shows that in 48.5% of cases there was angulation of the lateral lamella in one of the sides, most frequently at left.
In the association between categories, considering that only one patient had a Keros type III anatomical variation, and only one presented with different categories for left and right sides according to the Keros classification, both patients were excluded for the purpose of statistical analysis. Statistically significant association was not observed between the variation of the symmetry in the height of the lateral lamellas of the cribriform plates and the depth of olfactory fossae, but a statistically significant association was observed between the presence of angulation of the lateral lamellas of the cribriform plate and depth of olfactory fossae according to the Keros type found (Table 3).
DISCUSSION The relevance of evaluating the ethmoid roof, both by means of endoscopy and CT, for preventing surgical complications has been approached by several studies in the medical literature(24,7,8,10,14,30,31). Coronal CT images were selected, considering that the coronal plane is the best for evaluating the ethmoid roof anatomy, providing detailed information about this segment that usually presents many variations even between left and right sides in a same individual, and consequently minimizing risks in surgical interventions. Lesions in the skull base with laceration of the dura mater followed by liquoric fistula occur more easily in cases where the cribriform plate is thin and longer(6-10,18, 23,27,29,33). It is already well established that the area at risk is not in the highest point of the ethmoid sinus formed by the fovea ethmoidalis, but in the lateral lamella of the cribriform plate in the region of the ethmoidal sulcus. This is the most vulnerable site in the whole skull base where the anterior ethmoidal artery leaves the ethmoid sinus and courses anteriorly in the ethmoidal sulcus of the olfactory fossa(6,8-10). Studies about depth of the olfactory fossae have demonstrated divergences in relation to the distribution of frequency of Keros types. Basak et al.(28), evaluating 64 children, have found a higher frequency of Keros type II (53%), followed by type III (38%) and type I (9%). Jang et al.(34), in a study with 205 predominantly adult patients, have observed that Keros type II was most frequently found (69.5%), followed by type I (53.8%). In this latest series, no Keros type III olfactory fossa has been found. In another study developed with children in the age range between 0 and 14 years, Anderhuber et al.(33) have found 14.2% of Keros type I, 70.6% type II, and 15.2% type III. The present study, predominantly with adult patients, has also evidenced that Keros type II is the most frequently found (73.3%), followed by type I (26.2%), with type III being the type of anatomical variation less frequently found (0.5%). Despite the inter-study agreement regarding the Keros type II prevalence, there was a high variance in the frequency of type I, and remarkably in the frequency of type III. In the literature review, few studies were found reporting the frequency of asymmetry in the height of the lateral lamella of the cribriform plate. Wormald(35) has observed that the right fovea ethmoidalis was lower in 59% of cases. Dessi et al.(18), analyzing the height of the ethmoidal roof on 150 CT studies, have observed asymmetry in 15 patients (10%). Lebowitz et al.(36), in a review of 200 CT studies, have observed asymmetry in 19 cases (9.5%). In these three studies, ethmoidal roofs were lower at right. Similarly to the results of these two latest studies, the present study has found asymmetry in 24 patients (12%), 13 (54.1%) of them with lower ethmoidal roofs at right, and 11 (49.5%), at left. In the present study, asymmetry related to the angulation of the lateral lamella of the cribriform plate was observed in 48.5% of cases, in agreement with Lebowitz et al.(36), who have also demonstrated this finding in 48% of cases in their tomographic studies series. Both in the present study and in the one developed by Lebowitz, there was a prevalence of lateral angulation to the left. No study was found in the literature, correlating the presence of angulation of the lateral lamella of the cribriform plate with the Keros type of anatomical variation. In the present study, association of angulation of the lateral lamella of the cribriform plate with Keros type II was more frequently found than with Keros type I.
CONCLUSION Ethmoid roof asymmetry is a frequent anatomical variation that may occur as a result of the association of differences in the height of the lateral lamella and/or contour of the ethmoidal roof, with angulation of the lateral lamella. Symmetry in the ethmoid roof contour was found in a little more than 50% of individuals, and asymmetry, in most of cases resulted in difference in the ethmoid roof contour, with unilateral flattening. Most frequently, this finding was associated with the Keros type II. These findings emphasize the relevance of a careful evaluation, particularly in those individuals elected for endoscopic nasal surgery. The evaluation of the depth of the olfactory fossae and presence of ethmoidal roof asymmetry represents a significant aspect in tomographic studies, and should be included in the routine description of tomographic reports, considering the significant implication of these structures in the risk at endoscopic nasal surgeries.
REFERENCES 1. Luong A, Marple BF. Sinus surgery: indications and techniques. Clin Rev Allergy Immunol. 2006; 30:217-22. [ ] 2. Hemmerdinger SA, Jacobs JB, Lebowitz RA. Accuracy and cost analysis of image-guided sinus surgery. Otolaryngol Clin North Am. 2005; 38:453-60. [ ] 3. Schnipper D, Spiegel JH. Management of intracranial complications of sinus surgery. Otolaryngol Clin North Am. 2004;37:453-72, ix. [ ] 4. Stankiewicz JA. Complications of endoscopic intranasal ethmoidectomy. Laryngoscope. 1987; 97:1270-3. [ ] 5. Stammberger HR, Kennedy DW. Paranasal sinuses: anatomic terminology and nomenclature. The Anatomic Terminology Group. Ann Otol Rhinol Laryngol Suppl. 1995;167:7-16. [ ] 6. Kainz J, Stammberger H. The roof of the anterior ethmoid: a locus minoris resistentiae in the skull base. Laryngol Rhinol Otol (Stuttg). 1988;67: 142-9. [ ] 7. Ohnishi T. Bony defects and dehiscences of the roof of the ethmoid cells. Rhinology. 1981;19:195-202. [ ] 8. Ohnishi T, Tachibana T, Kaneko Y, et al. High-risk areas in endoscopic sinus surgery and prevention of complications. Laryngoscope. 1993;103:1181-5. [ ] 9. Stammberger H. Endoscopic anatomy of lateral wall and ethmoidal sinuses. In: Stammberger H, Hawke M, editors. Essentials of functional endoscopic sinus surgery. St. Louis: Mosby-Year Book; 1993. p. 13-42. [ ] 10. Ohnishi T, Yanagisawa E. Lateral lamella of the cribriform plate - an important high-risk area in endoscopic sinus surgery. Ear Nose Throat J. 1995;74:688-90. [ ] 11. Keros P. On the practical value of differences in the level of the lamina cribrosa of the ethmoid. Z Laryngol Rhinol Otol. 1962;41:809-13. [ ] 12. Basak S, Karaman CZ, Akdilli A, et al. Evaluation of some important anatomical variations and dangerous areas of the paranasal sinuses by CT for safer endonasal surgery. Rhinology. 1998;36: 162-7. [ ] 13. Lee JC, Song YJ, Chung YS, et al. Height and shape of the skull base as risk factors for skull base penetration during endoscopic sinus surgery. Ann Otol Rhinol Laryngol. 2007;116:199-205. [ ] 14. Bayram M, Sirikci A, Bayazit YA. Important anatomic variations of the sinonasal anatomy in light of endoscopic surgery: a pictorial review. Eur Radiol. 2001;11:1991-7. [ ] 15. Stankiewicz JA, Chow JM. The low skull base: an invitation to disaster. Am J Rhinol. 2004;18: 35-40. [ ] 16. Arslan H, Aydinlioglu A, Bozkurt M, et al. Anatomic variations of the paranasal sinuses: CT examination for endoscopic sinus surgery. Auris Nasus Larynx. 1999;26:39-48. [ ] 17. Zacharek MA, Han JK, Allen R, et al. Sagittal and coronal dimensions of the ethmoid roof: a radioanatomic study. Am J Rhinol. 2005;19:348-52. [ ] 18. Dessi P, Moulin G, Triglia JM, et al. Difference in the height of the right and left ethmoidal roofs: a possible risk factor for ethmoidal surgery. Prospective study of 150 CT scans. J Laryngol Otol. 1994;108:261-2. [ ] 19. Stankiewicz JA, Chow JM. The low skull base-is it important? Curr Opin Otolaryngol Head Neck Surg. 2005;13:19-21. [ ] 20. Ohnishi T, Yanagisawa E. Endoscopic anatomy of the anterior ethmoidal artery. Ear Nose Throat J. 1994;73:634-6. [ ] 21. Grevers G. Anterior skull base trauma during endoscopic sinus surgery for nasal polyposis preferred sites for iatrogenic injuries. Rhinology. 2001;39:1-4. [ ] 22. Sharp HR, Crutchfield L, Rowe-Jones JM, et al. Major complications and consent prior to endoscopic sinus surgery. Clin Otolaryngol Allied Sci. 2001;26:33-8. [ ] 23. Hudgins PA. Complications of endoscopic sinus surgery. The role of the radiologist in prevention. Radiol Clin North Am. 1993;31:21-32. [ ] 24. Rao VM, el-Noueam KI. Sinonasal imaging. Anatomy and pathology. Radiol Clin North Am. 1998;36:921-39, vi. [ ] 25. Araújo Neto SA, Martins PSL, Souza AS, et al. O papel das variantes anatômicas do complexo ostiomeatal na rinossinusite crônica. Radiol Bras. 2006;39:227-32. [ ] 26. Souza RP, Brito Júnior JP, Tornin OS, et al. Complexo nasossinusal: anatomia radiológica. Radiol Bras. 2006;39:367-72. [ ] 27. Melhem ER, Oliverio PJ, Benson ML, et al. Optimal CT evaluation for functional endoscopic sinus surgery. AJNR Am J Neuroradiol. 1996;17: 181-8. [ ] 28. Basak S, Akdilli A, Karaman CZ, et al. Assessment of some important anatomical variations and dangerous areas of the paranasal sinuses by computed tomography in children. Int J Pediatr Otorhinolaryngol. 2000;55:81-9. [ ] 29. Chong VF, Fan YF, Lau D, et al. Functional endoscopic sinus surgery (FESS): what radiologists need to know. Clin Radiol. 1998;53:650-8. [ ] 30. Kaluskar SK, Patil NP, Sharkey AN. The role of CT in functional endoscopic sinus surgery. Rhinology. 1993;31:49-52. [ ] 31. Teatini G, Simonetti G, Salvolini U, et al. Computed tomography of the ethmoid labyrinth and adjacent structures. Ann Otol Rhinol Laryngol. 1987;96(3 Pt 1):239-50. [ ] 32. Araujo Filho BC, Weber R, Pinheiro Neto CD, et al. Endoscopic anatomy of the anterior ethmoidal artery: a cadaveric dissection study. Rev Bras Otorrinolaringol. 2006;72:303-8. [ ] 33. Anderhuber W, Walch C, Fock C. Configuration of ethmoid roof in children 0-14 years of age. Laryngorhinootologie. 2001;80:509-11. [ ] 34.Jang YJ, Park HM, Kim HG. The radiographic incidence of bony defects in the lateral lamella of the cribriform plate. Clin Otolaryngol Allied Sci. 1999;24:440-2. [ ] 35. Wormald PJ. Surgery of the frontal recess and frontal sinus. Rhinology. 2005;43:82-5. [ ] 36. Lebowitz RA, Terk A, Jacobs JB, et al. Asymmetry of the ethmoid roof: analysis using coronal computed tomography. Laryngoscope. 2001;111: 2122-4. [ ] Received May 26, 2007. Accepted after revision September 4, 2007. * Study developed at Laboratório Diagnósticos da América, and Department of Imaging Diagnosis - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554