Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 2 - Mar. / Apr. of 2008
Vol. 41 nº 2 - Mar. / Apr. of 2008
|
ORIGINAL ARTICLE
|
|
Anastomotic leaks after Roux-en-Y gastric bypass surgery by Higa's technique for treatment of morbid obesity: radiological findings |
|
|
Autho(rs): Ester Moraes Labrunie, Edson Marchiori, Jean-Michel Tubiana |
|
|
Keywords: Morbid obesity, Bariatric surgery, Anastomotic leak, Complication, Radiology, Computed tomography |
|
|
Abstract:
IPhD, Associate Professor, Universidade Federal do Rio de Janeiro (UFRJ), MD, Radiologist at Casa de Saúde São José, Rio de Janeiro, RJ, Brazil
INTRODUCTION Obesity is a chronic disease characterized by excessive body fat, frequently associated with a series of related diseases, with increased risk of physical disability and early mortality. An endemic increase of this disease has been observed worldwide(1,2). Morbid obesity is defined as a body mass index of > 40 kg/m², or yet > 35 kg/m² in patients with comorbidity(1,3). Non-surgical treatments outcomes have been disappointing, and bariatric surgery has been indicated as the only reliable method allowing significant weight loss, extended weight maintenance and management and reversion of some obesity-related comorbidities(1,4,5). Postoperative radiological evaluation, aiming at an early diagnosis of possible complications in patients submitted to bariatric surgery, is frequently part of radiologists in their daily practice. The diagnosis may be difficult because of technical limitations imposed by these patients' biotype and clinical condition. A detailed and careful analysis represents a challenge both to the surgical team and the radiologist. An incorrect evaluation or late diagnosis of complications may delay the treatment or even put the patients' life at risk. Postoperative anastomotic leak with peritonitis is the most severe early complication of the Roux-en-Y gastric bypass surgery, occurring in 1% to 6% of cases(6,7). In these cases the hospitalization period is extended, and the morbidity and mortality rates are significantly increased(7–9), particularly in cases of high output leaks(6). Patients with this complication are submitted to a higher number of diagnostic procedures and, frequently require surgical reintervention(8). The present study was aimed at evaluating the imaging findings observed in 24 patients who developed anastomotic leaks as a complication resulting from gastroplasty by the Higa's technique for treatment of morbid obesity.
MATERIALS AND METHODS Twenty-four patients submitted to Roux-em-Y gastric bypass surgery by the Higa's technique, with postoperative anastomotic leaks were studied in the period between November 2001 and April 2006. The surgeries were performed by eight different surgical teams in eight hospitals/institutions, and the study was approved by the Committee for Ethics in Research of Casa de Saúde São José, Rio de Janeiro, RJ. The sample of the present study included 20 female (83.4%) and four male (16.6%) patients with ages ranging between 23 and 56 years (mean, 38 years). Twenty-one patients underwent videolaparoscopy surgery (87.5%), and three, laparotomy (12.5%). A total of 74 iodinated-contrast enhanced radiological studies — 55 computed tomographies (CT) and 19 upper gastrointestinal series (UGIS) — were evaluated. The confirmation of the diagnoses of anastomotic leaks was based on one or more of the following criteria: image finding of oral contrast extravasation, opacification of surgical drain by oral methylene blue and/or surgical confirmation. Both direct and indirect signs of leaks were investigated. Contrast material extravasation was considered as a direct sign of leak. Indirect signs considered as suggestive of leak were: disproportionate postoperative pneumoperitoneum or progressive increase in the gas volume; intracavitary fluid collections, with or without fluid or contrast material level inside; significant amount of fluid in the subphrenic and/or perihepatic spaces. Five patients had not been radiologically diagnosed. Four of them underwent surgical reintervention, and one was submitted to conservative clinical treatment. All of them were subsequently submitted to radiological examination, with detection of contrast material extravasation in one, and indirect signs of leak in the other four patients. The leaks were classified as early (occurring up to the 7th postoperative day), and intermediate (occurring between the 8th and the 30th postoperative days).
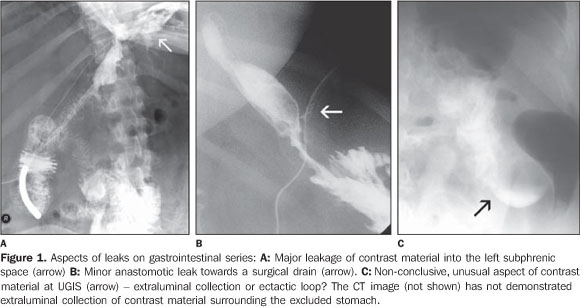
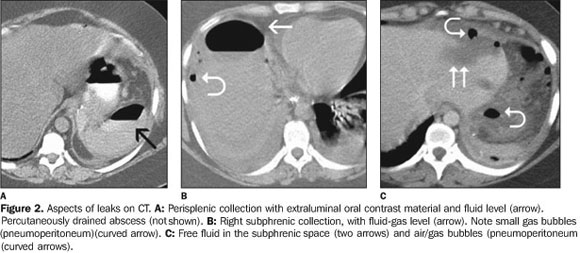
RESULTS Leakage was the first postoperative complication in 22 patients. The initial complications in the remainder two patients were bowel obstruction (one case), and anastomotic edema (one case). As regards the moment of the leak onset, the cases were divided into: early (18 cases) and intermediate (six cases). In the present casuistic, leaks onset after the 30th postoperative day was not observed. Contrast material extravasation was detected at the initial examination — either UGIS (Figure 1) or CT (Figure 2A). Subsequent studies demonstrated contrast material extravasation in eight of the other 14 patients. In four patients, only indirect sings of leaks were found (Figures 2B and 2C). Two patients were clinically/surgically diagnosed.
Fifty-five CT studies were performed in the 24 patients with anastomotic leaks (one to seven studies per patient). Seventeen CT studies were performed at the moment of the complication diagnosis, eight of them demonstrating contrast material extravasation, and three were normal. The other six patients demonstrated only indirect signs of leak. Alterations considered as indirect signs and observed at the initial examination of these 24 patients were: pneumoperitoneum (tem patients), anastomotic edema (five patients), intracavitary fluid collections (four patients) and free intraperitoneal fluid (three patients). Follow-up CT studies could demonstrate contrast material extravasation which had not been detected at the first examination in seven patients. Thirteen patients with anastomotic leaks were submitted to upper gastrointestinal series. Eight studies were performed at the time of the diagnosis, with contrast material extravasation being detect in only three. Follow-up examinations allowed the detection of the leak which had not been visualized at the initial examination in two patients. The amount and sites of contrast material extravasation were variable, these being quite evident in some studies and more subtle in others. Many times, small extravasations through the surgical drain adjacent to the stapling line were difficult to be visualized; sometimes, contrast material was permeated with gas bubbles along the drain passage. Fifteen of the 24 patients were submitted to surgery after being diagnosed with anastomotic leaks either because of the extent of contrast material extravasation, because of the complications diagnosed at this first moment, or because of the necessity to review the anastomosis and place surgical drains. In nine patients, the treatment was conservative and/or by interventional radiology. In 15 patients, the leak caused other complications, with extended hospital stays, with one case progressing to death because of septic and pulmonary complications. Eleven patients evolved with significant intracavitary fluid collections, eight of them being treated by interventional radiology (abscesses). Other complications observed were: evisceration (two cases), intracavitary hematoma after surgical reintervention (two cases), lasting leaks observed at clinical follow-up for more than two months (two cases), multiple enterocutaneous fistulas (in patients with obstruction by debris and volvulus anterior to the fistula). A patient with anastomotic dehiscence was submitted to resection of the small gastric chamber and evolved with stenosis of the esophagojejunal anastomosis, requiring endoscopic treatment.
DISCUSSION Several surgical techniques are available for the management of morbid obesity, each of them with possible complications, where radiological studies play an extremely significant role in the diagnosis and follow-up(10,11). Anastomotic leaks constitute one of the more severe and feared postoperative complications of this type of surgery, as far as its high morbidity and mortality rates are concerned(8,12). Patients with this complication require longer hospital stay, remaining in intensive care units because of septic shock, multiple organs failure or intracavitary abscesses(8). The clinical condition, including non-specific symptoms such as tachycardia, tachypnea and fever, is atypical. Performing a physical examination may be difficult and the findings may be misleading(6) so, many times, complementary imaging studies are necessary to define the diagnosis(8). Oral administration of methylene blue and subsequent staining of the intracavitary drain is a simple test frequently utilized in these cases; however, the absence of communication between the leak and the surgical drain may give false-negative results(13). Patients without a surgical drain cannot be submitted to this test. Frequently, a delay in the treatment of anastomotic leaks results in progression to sepsis, organs failure and death(14). In the present casuistic, one of the patients diagnosed with anastomotic leak by methylene blue test, had the leak demonstrated only at the follow-up UGIS, where the filiform passage of the contrast medium into the surgical drain was identified. Contrast material extravasation was not identified at the CT study performed in the same day, since a spontaneously dense surgical drain was visualized. CT plays a complementary role to the upper gastrointestinal series (UGIS) in the diagnosis of anastomotic leaks(3). CT seems to be more sensitive for this evaluation, allowing the association between direct and indirect signs, as well as the investigation of secondary complications such as fluid collections(6). On the other hand, iodinated contrast-enhanced UGIS can demonstrate small contrast material extravasations into surgical drains which cannot be visualized at CT, as observe in one of the patients in the present casuistic. Undetected small leakages may result in an extemporaneous withdrawal of the surgical drain and initiation of the oral diet, with harmful consequences for the patient. Small leaks oriented towards the surgical drain and with no sign of a resistant sepsis can be clinically treated by means of antibiotics and parenteral nutrition, and usually resolve spontaneously(15). However, they also may result in intracavitary fluid collections and development of a chronic fistulous tract(6), most frequently found in major leaks(7). Gonzalez et al.(8) have reported that the presence of a surgical drain allows the diagnosis of leaks in 50% of cases and, most of time, a clinic, conservative treatment of this complication in hemodynamically stable patients. Several signs suggestive of anastomotic leak are described in the literature. The presence of oral contrast extravasation is a direct sign of leak. Other aspects considered as indirect signs and already described in the literature(8,16) are collections (especially those adjacent to the gastric reservoir) and free fluid in the abdominal cavity. In the present casuistic, such findings have also been observed. Pneumoperitoneum may be observed, although in a small volume, in the early postoperative period by the presence of a surgical drain. A higher-than-expected volume of pneumoperitoneum, or even its increase at subsequent examinations has also been considered as an indirect sign indicating a leak. This was the indirect sign most frequently found in the present casuistic. Blachar et al.(3) have reported that the majority of leak-related collections occur in the perianastomotic region and in the upper left quadrant of the abdomen, particularly in the perisplenic region. In the present study, 13 abscesses were observed in ten patients with the following localizations: left perisplenic/subphrenic (six cases), left anterior subphrenic (two cases), right subphrenic (two cases), posterior to the excluded stomach (one case), Douglas' pouch (one case), and pararectal fossa (one case). Oral contrast extravasation into the collection was observed in two cases. Eight patients with abscesses were successfully submitted to CT-guided percutaneous puncture and drainage. Oligosymptomatic patients may not present any evidence of leakage at an early postoperative UGIS. Later complementary studies may be required to demonstrate the presence of a leak, as well as to evaluate its extent, orientation, or not, to surgical drains, presence of collections and evaluation of the possibility of treatment by means of percutaneous drainage(8,12). Ten of the 24 patients studied in the present casuistic demonstrated the presence of contrast material extravasation at the first examinations. Six of the remainder 14 patients presented solely indirect signs of leakage at the moment of the diagnosis. Subsequent CT studies and/or UGIS demonstrated the presence of extraluminal contrast material in these six patients. No abnormality was found on the initial CT/UGIS of other three patients, whose diagnosis was based on their clinical signs. Follow-up examination of one of these three patients demonstrated contrast material extravasation; the diagnosis was clinical/surgical in two patients. Five patients included in the present study were not radiologically diagnosed, and active contrast extravasation was found in one of them during a follow-up examination. In four patients the diagnosis was based on the presence of indirect signs. According to Hamilton et al.(12), the peak of tension on tissues and anastomosis occurs between the 5th and 7th postoperative day, and therefore this is the period where a leakage onset probability is highest. These data are coincidental with the present casuistic where 17 of the 24 patients with anastomotic leaks presented the complication up to the 7th postoperative day, and seven between the 8th and 12th postoperative days. No leak developed after this period. It is an assumption of these authors(12) that this can be a reason for the presence of leaks not being identified on UGIS performed within the first 48 postoperative hours. Such an argument corroborates the idea that asymptomatic patients should be submitted to early routine postoperative studies. Luján et al.(15) have highlighted that a loop distention above the intestinal obstructions either in the alimentary or biliary branch, submit the anastomosis to a higher tension with a risk for development of leaks and/or dehiscence progressing to death in some patients. In this casuistic, leakage has been observed in two patients with intestinal obstruction and in five with anastomotic edema. Finally, imaging methods play a significant role in the postoperative evaluation of bariatric surgery both for diagnosis and follow-up of these patients, with a significant contribution to the guidance for management and treatment of complications. CT and UGIS are usually the methods of choice in these cases, many times playing complementary roles in the documentation of certain abnormalities. Anastomotic leakage is the most frequent early complication of gastric bypass surgery and may determine severe outcomes with the development of secondary complications. Extraluminal contrast material is the direct sign of the presence of a leak, although this complication may not be visualized at the initial examination. Other findings should such as presence and/or increase in pneumoperitoneum as well as intracavitary collections should be taken into consideration.
REFERENCES 1. Blachar A, Federle MP. Gastrointestinal complications of laparoscopic Roux–en–Y gastric bypass surgery in patients who are morbidly obese: findings on radiography and CT. AJR Am J Roentgenol. 2002;179:1437–42. [ ] 2. Moura Jr LG, Guimarães SB, Castro–Filho HF, et al. Capella's gastroplasty: metabolites and acute phase proteins changes in midline and bilateral arciform approaches. Arq Gastroenterol. 2004;41: 215–9. [ ] 3. Blachar A, Federle MP, Pealer KM, et al. Gastrointestinal complications of laparoscopic Roux–en–Y gastric bypass surgery: clinical and imaging findings. Radiology. 2002;223:625–32. [ ] 4. Pareja JC, Pilla VF, Callejas–Neto F, et al. Gastric bypass Roux–en–Y gastrojejunostomy conversion to distal gastrojejunoileostomy for weight loss failure – experience in 41 patients. Arq Gastroenterol. 2005;42:196–200. [ ] 5. Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult–onset diabetes mellitus. Ann Surg. 1995;222:339–52. [ ] 6. Blachar A, Federle MP, Pealer KM, et al. Radiographic manifestations of normal postoperative anatomy and gastrointestinal complications of bariatric surgery, with emphasis on CT imaging findings. Semin Ultrasound CT MRI. 2004;25: 239–51. [ ] 7. Carucci LR, Turner MA. Radiologic evaluation following Roux–en–Y gastric bypass surgery for morbid obesity. Eur J Radiol. 2005;53:353–65. [ ] 8. Gonzalez R, Nelson LG, Gallagher SF, et al. Anastomotic leaks after laparoscopic gastric bypass. Obes Surg. 2004;14:1299–307. [ ] 9. See C, Carter PL, Elliott D, et al. An institutional experience with laparoscopic gastric bypass complications seen in the first year compared with open gastric bypass complications during the same period. Am J Surg. 2002;183:533–8. [ ] 10. Labrunie EM, Marchiori E. Obstrução intestinal pós–gastroplastia redutora pela técnica de Higa para tratamento da obesidade mórbida: aspectos de imagem. Radiol Bras. 2007;40:161–5. [ ] 11. Francisco MC, Barella SM, Abud TG, et al. Análise radiológica das alterações gastrintestinais após cirurgia de Fobi–Capella. Radiol Bras. 2007; 40:235–8. [ ] 12. Hamilton EC, Sims TL, Hamilton TT, et al. Clinical predictors of leak after laparoscopic Roux–en–Y gastric bypass for morbid obesity. Surg Endosc. 2003;17:679–84. [ ] 13. Onopchenko A. Radiological diagnosis of internal hernia after Roux–en–Y gastric bypass. Obes Surg. 2005;15:606–11. [ ] 14. Singh R, Fisher BL. Sensitivity and specificity of postoperative upper GI series following gastric bypass. Obes Surg. 2003;13:73–5. [ ] 15. Luján JA, Frutos MD, Hernández Q, et al. Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg. 2004;239:433–7. [ ] 16. Yu J, Turner MA, Cho SR, et al. Normal anatomy and complications after gastric bypass surgery: helical CT findings. Radiology. 2004;231:753–60. [ ] Received June 28, 2007. Accepted after revision August 6, 2007. * Study developed in the Department of Radiology at Universidade Federal do Rio de Janeiro (UFRJ) and Casa de Saúde São José, Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554