Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 2 - Mar. / Apr. of 2008
Vol. 41 nº 2 - Mar. / Apr. of 2008
|
ORIGINAL ARTICLE
|
|
Ultrasonographic assessment of splenic siderotic nodules in schistosomal patients with portal hypertension |
|
|
Autho(rs): Thais Dias Gonzalez, José Eduardo Mourão Santos, Danilo Moulin Sales, Kenji Takemoto, Júlia Capobianco, Paulo Eugênio Brant, Ramiro Colleoni, Munneb Ahmed, Giuseppe D'Ippolito |
|
|
Keywords: Schistosomiasis mansoni, Ultrasonography, Spleen |
|
|
Abstract:
IMD, Residents, Department of Imaging Diagnosis of Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil
INTRODUCTION Schistosomiasis still remains as a relevant problem of public health both in Brazil and worldwide, where it is estimated that, respectively, 18 and 200 million persons are infected(1–3). Ultrasonography (US) is the method most frequently utilized for assessing schistosomal patients in the hepatosplenic phase of the disease characterized by portal hypertension secondary to the development of periportal fibrosis(4–6). Siderotic nodules, or Gamna-Gandy bodies, consist in small fibrotic nodules impregnated with hemosiderin, resulting from focal micro-hemorrhages in the splenic parenchyma caused by vascular congestion in this organ. Portal hypertension is the most frequent cause of splenic siderotic nodules(7). Gamna-Gandy bodies may be evaluated by different imaging methods(8), but presently magnetic resonance imaging (MRI)m especially with gradient-echo sequences is considered as the method of choice in the detection of these nodules(9,10). The US value in the assessment of Gamna-Gandy bodies has been discussed in the literature with controversial results and sensitivity ranging between 12% and 70.6%(10,11). As regards diagnostic tests, a decisive parameter to be taken into consideration is the method accuracy that can be evaluated by means of its reproducibility. No study is available in the current literature evaluating the US reproducibility based on the measurement of interobserver agreement for detection of splenic siderotic nodules. The present study was aimed at measuring the sensitivity and reproducibility of US in the detection of splenic siderotic nodules in comparison with magnetic resonance imaging as standard method.
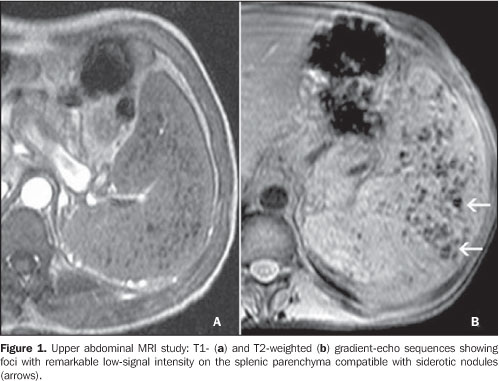
MATERIALS AND METHODS Patients' selection In the first phase of the present study, 20 patients with hepatosplenic schistosomiasis (11 men and nine women in the age range between 23 and 87 years, mean age = 44 years), diagnosed with siderotic nodules at MRI and submitted to ultrasonographic evaluation in a term of less than three months for determining the sensitivity of the method. MRI studies were utilized as a reference standard in the research, and evaluated in consensus by two experienced observers with more than five years of practice in abdominal radiology. The second phase of the study was aimed at evaluating the US reproducibility in the detection and quantification of siderotic nodules in other 30 patients diagnosed with hepatosplenic schistosomiasis (15 men and 15 women with ages ranging between 25 and 68 years, mean age = 45 years) submitted to ultrasonographic evaluation. All of the US studies were performed by two observers with four-year residency in imaging diagnosis and previously trained to identify and quantify splenic siderotic nodules. All of the selected patients were above 18 years of age and being followed-up in the departments of Clinical and/or Surgical Gastroenterology at Hospital São Paulo – Universidade Federal de São Paulo. Exclusion criteria were the following: continued utilization hepatotoxic pharmaceuticals, positive serology for hepatitis B or C viruses, and history of chronic alcoholism. The present study was previously approved by the Committee for Ethics in Research of the Institution and a term of free and informed consent was signed by all of the patients. MRI evaluation MRI studies were performed in high magnetic field (1.5 tesla) Magnetom Symphony™ system (Siemens; Erlangen, Germany), with multiplanar (axial and coronal), turbo spin-echo and gradient-echo T1- and T2-weighted sequences, before and after intravenous paramagnetic contrast injection. The diagnosis of siderotic nodules was defined by the presence of small foci of lowintensity signal on all of the sequences, especially on gradient-echo T2*-weighted sequences without significant enhancement after contrast injection (Figure 1)(9,10). The MRI studies analysis was performed on a Leonardo (Siemens) workstation.
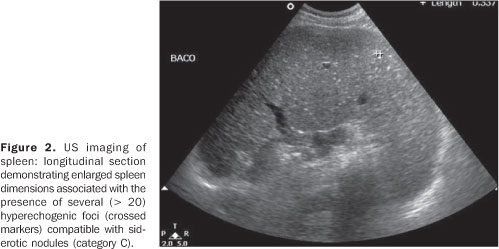
Ultrasonographic evaluation Ultrasonography studies were performed on an EnVisor™ (Philips Medical Systems; Bothell, WA, USA) equipment coupled with a convex, multi-frequency transducer. The diagnosis was considered as positive for siderotic nodules in the presence of dispersed, hyperechogenic, parenchymal foci non-attributable to thickened vessels walls in the spleen (Figure 2). Siderotic nodules identified were classified according to methodology already proposed(12), as follows:
– Category A: a transverse section of the spleen demonstrating < 5 nodules (focal); – category B: a transverse section of the spleen demonstrating 6-20 nodules (scattered); – category C: a transverse section of the spleen demonstrating > 20 nodules (diffuse). Statistical analysis The interobserver agreement was measured by means of kappa index, an useful test for classifying the variability in the interpretation of different data sets including categorical variables(13). Kappa indices were classified as follows: non-significant (0.0–0.2), median (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80), and almost-perfect (0.81–1.00).
RESULTS Twenty of the 21 patients with siderotic nodules detected by MRI were correctly evaluated by US, whereas in only one patient ultrasound could not detect these nodules, giving the method a sensitivity of 95.2% (confidence interval at 95% [77.3%; 99.2%]). The evaluation of the US reproducibility in determining the presence of siderotic nodules in the 30 patients included in the present study demonstrated an interobserver agreement of 96.7% (confidence interval at 95% [82.8%; 99.9%]). The reproducibility of the classification of siderotic nodules into categories according to their quantity, demonstrated a substantial interobserver agreement (kappa = 0.672; confidence interval at 95% [0.374; 0.970]).
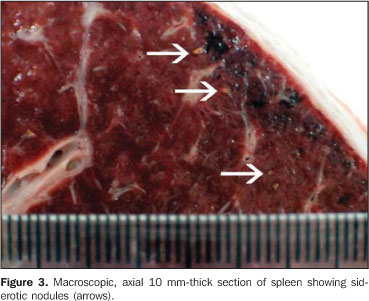
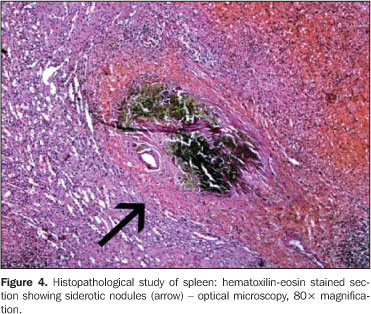
DISCUSSION US is considered as the method of choice in the evaluation of schistosomal patients, considering its wide availability, excellent cost-benefit ratio, and non-invasiveness(6). Sonographic alterations detected in these patients have already been described and currently are widely utilized both for evaluating the hepatic involvement, determining the level of portal hypertension and characterizing splenic siderotic nodules(4,6,14). However, for establishing the validity of a diagnostic test, it is important to define, besides its efficacy, its accuracy, which can be determined by calculating the method reproducibility. The present study has been driven particularly by the absence, in the medical literature, of a systematic evaluation of the US reproducibility by means of the measurement of interobserver agreement as regards the detection of splenic siderotic nodules. Siderotic nodules, or Gamna-Gandy bodies, were firstly described by Marini, in 1902, but this entity became actually known with the studies developed in 1905 and 1921 by Charles Gandy and Carlo Gamna, giving rise to the eponym(9). Siderotic nodules consist in small fibrotic nodules impregnated with hemosiderin and, in some cases with calcifications resulting from focal microhemorrhages in the splenic parenchyma, generally related to congestive splenomegaly (Figures 3 and 4). Most rarely, siderotic nodules may be found in other tissues such as thymus, lymphonodi, liver, heart, and in conditions such as paroxysmal nocturnal hemoglobinuria, leukemia and lymphoma(7,15–19). However, portal hypertension is the most frequent cause of these nodules, which are present in about 9% to 12% of patients with portal hypertension for causes unrelated to schistosomiasis(9,10).
The relevance of detecting the presence of splenic siderotic nodules by means of imaging methods is related to the fact that these nodules represent a morphological evidence of a long lasting portal hypertension process(20). Currently the relevant role of MRI as a reference method in the detection of siderotic nodules is a consensus in the literature(8–10,20–23). MRI is extremely sensitive to paramagnetic contrast agents; hemoglobin products (for example, hemosiderin) have a paramagnetic effect, being easily detected on RM images (especially the high field ones), were they appear like low-signal intensity nodules or absent signal on spin-echo and especially gradient-echo T1- and T2-weighted images(8,9,20) (Figure 1). These nodules also can be evaluated by other imaging methods such as computed tomography (CT) and US. On US images, the nodules appear as small, punctate hyperechogenic foci sparsely scattered in the splenic parenchyma, with or without posterior acoustic shadowing, non-attributable to small vessels walls(7) (Figure 2). The incidence of these nodules initially described in the literature for schistosomal patients in the hepatosplenic phase, was of 7% in studies utilizing US as imaging method(14). Most recently, studies utilizing MRI have found a much higher incidence of siderotic nodules (84.2%) in schistosomal patients(21). In the present study, the frequency of detection of siderotic nodules by US and MRI in patients with hepatosplenic schistosomiasis was also very high, ranging between 96.6% and 100%. Ultrasonography sensitivity in the detection of siderotic nodules also has been discussed. Differently from previous studies developed in the eighties, reporting sensitivities between 10.5% and 25%(9,10), the current literature describes a high diagnostic accuracy for this method, with 70.6% sensitivity, 78.9% specificity, and 85.7% positive predictive value(11). The results of the present study surpassed these latter, with 95.2% sensitivity. This discrepancy in relation to the US frequency and sensitivity in detecting siderotic nodules can be attributed to the utilization of observers specifically trained for researching these nodules, and, also, to the technological developments of US systems over the last two decades, with an expressive improvement in their images resolution. Apparently, in cirrhotic patients, the presence and number of siderotic nodules are associated with their level of portal hypertension(20). The quantification of these nodules and their classification into categories according to the number of nodules found had been already proposed for the liver(12), but had not been utilized for the spleen yet. The present study found a high interobserver agreement as to the overall presence or absence of siderotic nodules (96.7%). Regarding the US reproducibility for the quantification and classification of siderotic nodules into categories, the kappa index showed a substantial interobserver agreement (0.67). Additional studies are required for determining the significance of this quantification and its actual correlation with the level of portal hypertension. In addition, in the present study, a tendency towards a higher interobserver agreement was observed in relation to patients with a higher number of siderotic nodules (category C). In the patients with lower number of siderotic nodules (especially in those of category A), the main difficulty found by the observers was the differentiation between true nodules and small vessels walls; color Doppler US may be useful in this differentiation. In the present study, however, color Doppler US could not be utilized, considering that this previously unforeseen difficulty occurred only with some patients evaluated late in the development of the study. Amongst the differential diagnoses for splenic siderotic nodules observed at US, tuberculotic calcified granulomas should be considered. These granulomas tend to be larger and more hyperechogenic than siderotic nodules, besides presenting an evident acoustic shadowing, a feature that is not present in the case of non-calcified siderotic nodules(9), which represented the majority in the present study. Additionally, because of the paramagnetic effect of hemosiderin products, siderotic nodules are clearly visualized on T1- and T2-weighted images as small foci of lowintensity or absent signal and without contrast-enhancement after intravenous gadolinium injection(9,10). Conversely, non-calcified tuberculotic nodules tend to present a variable signal on T1- and T2-weighted images, and most frequently with hyper-intense signal and ring-shaped contrastenhancement after gadolinium injection(24). Calcified siderotic nodules may not be distinguishable from different types of calcified granulomas, like those resulting from tuberculosis and histoplasmosis(9). Amongst the limitations of the present study, it is important to note the restricted number of patients included in the sample, as well as the absence of a control group which would allow the addition of other useful information (for example, specificity, positive and negative predictive values) for determining the US diagnostic accuracy in the detection of these nodules. Certainly, MRI cost and availability represent a limiting factor for the further expansion of the sample. Notwithstanding, it is important to note that the group of patients included in the present study reflects the reality of our institution, as it may be evidenced by other studies in this same research line(25,26). Considering the lack of previous experiments, the quantitative classification of splenic siderotic nodules was adapted from a classification proposed for hepatic siderotic nodules in cirrhotic patients(12), and that was not previously validated in schistosomal patients. Another type of classification could demonstrate results different from the ones in the present study. Finally, just as demonstrated by other authors(4), the present study demonstrated that ultrasonography, besides being a low-cost, non-invasive and widely available imaging method, is highly sensitive and reproducible in the evaluation of splenic siderotic nodules in patients affected by schistosomal portal hypertension.
REFERENCES 1. Alves Jr A, Fontes DA, Melo VA, et al. Hipertensão portal esquistossomótica: influência do fluxo sangüíneo portal nos níveis séricos das enzimas hepáticas. Arq Gastroenterol. 2003;40:203–8. [ ] 2. Henri S, Chevillard C, Mergani A, et al. Cytokine regulation of periportal fibrosis in humans infected with Schistosoma mansoni: IFN-gamma is associated with protection against fibrosis and TNF-alpha with aggravation of disease. J Immunol. 2002;169:929–36. [ ] 3. Oliveira-e-Silva A, D'Albuquerque LAC. Esquistossomose mansônica hepatoesplênica: uma doença trágica. Arq Gastroenterol. 2003;40:201–2. [ ] 4. Machado MM, Rosa ACF, Oliveira IRS, et al. Aspectos ultra-sonográficos da esquistossomose hepatoesplênica.Radiol Bras. 2002;35:41–5. [ ] 5. Andrade ZA. The situation of hepatosplenic schistosomiasis in Brazil today. Mem Inst Oswaldo Cruz. 1998;93:313–6. [ ] 6. Hatz C, Jenkins JM, Ali QM, et al. A review of the literature on the use of ultrasonography in schistosomiasis with special reference to its use in field studies. 2. Schistosoma mansoni. Acta Trop. 1992;51:15–28. [ ] 7. Bhatt S, Simon R, Dogra VS. Gamna-Gandy bodies sonographic features with histopathologic correlation. J Ultrasound Med. 2006;25:1625–9. [ ] 8. Selçuk D, Demirel K, Kantarci F, et al. Gamna-Gandy bodies: a sign of portal hypertension. Turk J Gastroenterol. 2005;16:150–2. [ ] 9. Minami M, Itai Y, Ohtomo K, et al. Siderotic nodules in the spleen: MR imaging of portal hypertension. Radiology. 1989;172:681–4. [ ] 10. Sagoh T, Itoh K, Togashi K, et al. Gamna-Gandy bodies of the spleen: evaluation with MR imaging. Radiology. 1989;172:685–7. [ ] 11. Chan YL, Yang WT, Sung JJY, et al. Diagnostic accuracy of abdominal ultrasonography compared to magnetic resonance imaging in siderosis of the spleen. J Ultrasound Med. 2000;19: 543–7. [ ] 12. Krinsky GA, Lee VS, Nguyen MT, et al. Siderotic nodules at MR imaging: regenerative or dysplastic? J Comput Assist Tomogr. 2000;24:773–6. [ ] 13. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [ ] 14. Cerri GG, Alves VAF, Magalhães A. Hepatosplenic schistosomiasis mansoni: ultrasound manifestations. Radiology. 1984;153:777–80. [ ] 15. Krinsky GA, Lee VS, Nguyen MT, et al. Siderotic nodules in the cirrhotic liver at MR imaging with explant correlation: no increased frequency of dysplastic nodules and hepatocellular carcinoma. Radiology. 2001;218:47–53. [ ] 16. Kim MJ, Mitchell DG, Ito K, et al. Hepatic iron deposition on MR imaging in patients with chronic liver disease: correlation with serial serum ferritin concentration. Abdom Imaging. 2001;26:149–56. [ ] 17. Roubidoux MA. MR of the kidneys, liver and spleen in paroxysmal nocturnal hemoglobinuria. Abdom Imaging. 1994;19:168–73. [ ] 18. Watanabe M, Takazawa K, Wada A, et al. Cardiac myxoma with Gamna-Gandy bodies: case report with MR imaging. J Thorac Imaging. 1994;9: 185–7. [ ] 19. Kaneko K, Onitsuka H, Murakami J, et al. MRI of primary spleen angiosarcoma with iron accumulation. J Comput Assist Tomogr. 1992;16:298–300. [ ] 20. Ünsal NH, Erden A, Erden I. Evaluation of the spleenic vein diameter and longitudinal size of the spleen in patients with Gamna-Gandy bodies. Diagn Interv Radiol. 2006;12:125–8. [ ] 21. Bezerra ASA, D'Ippolito G, Caldana RP, et al. Chronic hepatosplenic schistosomiasis mansoni: magnetic resonance imaging and magnetic resonance angiography findings. Acta Radiol. 2007;48:125–34. [ ] 22. Dobritz M, Nömayr A, Bautz W, et al. Gamna-Gandy bodies of the spleen detected with MR imaging: a case report. Magn Reson Imaging. 2001;19:1249–51. [ ] 23. Elsayes KM, Narra VR, Mukundan G, et al. MR imaging of the spleen: spectrum of abnormalities. Radiographics. 2005;25:967–82. [ ] 24. De Backer AI, Vanhoenacker FM, Mortelé KJ, et al. MRI features of focal splenic lesions in patients with disseminated tuberculosis. AJR Am J Roentgenol. 2006;186:1097–102. [ ] 25. Bezerra ASA, D'Ippolito G, Caldana RP, et al. Avaliação hepática e esplênica por ressonância magnética em pacientes portadores de esquistossomose mansônica crônica. Radiol Bras. 2004; 37:313–21. [ ] 26. Caldana RP, Bezerra ASA, D'Ippolito G, et al. Estudo da circulação hepatomesentérica pela angiografia por ressonância magnética com gadolínio: comparação entre doses simples e dupla no estudo de pacientes esquistossomóticos. Radiol Bras. 2006;39:243–51. [ ] Received August 27, 2007. Accepted after revision October 1st, 2007. * Study developed in the Department of Imaging Diagnosis of Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554