Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 1 - Jan. /Feb. of 2008
Vol. 41 nº 1 - Jan. /Feb. of 2008
|
ORIGINAL ARTICLE
|
|
Evaluation of urogenital fistulas by magnetic resonance urography |
|
|
Autho(rs): Augusto Elias Mamere, Rafael Darahem Souza Coelho, Alexandre Oliveira Cecin, Leonir Terezinha Feltrin, Fabiano Rubião Lucchesi, Marco Antônio Lopes Pinheiro, Ana Karina Nascimento Borges, Gustavo Fabene Garcia, Daniel Seabra |
|
|
Keywords: Urinary fistula, Vesicovaginal fistula, Urological diagnostic techniques, Magnetic resonance imaging, Vaginal fistula - diagnosis |
|
|
Abstract:
IMaster, MDs, Radiologists at Hospital de Câncer de Barretos – Fundação Pio XII, Barretos, SP, Brazil
INTRODUCTION Several types of pelvic fistulas secondary to pelvic diseases or surgeries have already been described: vesicovaginal, vesicouterine, ureterovaginal, ureteroenteric, enterovaginal and rectovaginal fistulas(1–3). The close proximity of pelvic organs makes the genitourinary system susceptible to injury, so the majority of fistulas occur in the pelvic cavity(1). Main causes of pelvic fistulas are surgical or obstetric procedures, malignant tumors, radiotherapy, pelvic infections, traumas and inflammatory intestinal diseases(2,4,5). Vesicovaginal and ureterovaginal are some of the most frequent types of fistulas. The most frequent predisposing factor for vesicovaginal fistula is uterine cervix cancer treated with radiotherapy, with an incidence ranging between 1% and 10%(6). Ureterovaginal fistulas occur most frequently after gynecologic or obstetric surgeries, usually as a sequela of an iatrogenic lesion of the ureter, but also may appear after a pelvic radiotherapy(1). These fistulas subtypes occurring in the female lower urinary tract (vesicovaginal and ureterovaginal) cause social and psychological anguish, and frequently represent a therapeutic problem for the surgeon(7), particularly when they appear after radiotherapy, associated with involvement of the vascular supply and difficulty in cicatrization and regeneration of the irradiated tissue(8). The main symptom of patients with ureterovaginal or vesicovaginal fistulas secondary to pelvic surgery or disease is a continuous involuntary discharge of urine into the vaginal vault(1,7). Hematuria, urinary infections or perineal dermatitis may be associated(1,2). The following procedures can be utilized in the diagnosis of these fistulas: cystoscopy, vaginoscopy, computed tomography and magnetic resonance imaging(1,4). Magnetic resonance imaging allows the identification of the fistulous tract, as well as the evaluation, by means of sections in different planes, of alterations which eventually may be present in the adjacent pelvic structures, allowing an appropriate surgical planning. Magnetic resonance urography images allow a global, non-invasive visualization of the whole urinary tract, without the need for ionizing radiation and administration of contrast agents. In the medical literature review, few studies were found investigating the utilization of magnetic resonance imaging for the diagnosis and evaluation of urogenital fistulas(1–5). In these studies, the patients have been evaluated only with axial and sagittal sections on conventional sequences, with no magnetic resonance urography sequence. The present study is aimed at demonstrating the potential and applicability of magnetic resonance urography in the diagnosis of vesicovaginal and ureterovaginal fistulas as well as in the visualization of fistulous tracts.
MATERIALS AND METHODS Dossiers, radiological and magnetic resonance urography images of seven female patients diagnosed with vesicovaginal or ureterovaginal fistulas were retrospectively evaluated. The clinicalpathological profiles of these patients are summarized on Table 1.
Magnetic resonance imaging studies were performed in a 1.5 tesla Magnetom Symphony equipment (Siemens®; Erlangen, Germany), with 30 mT/m gradient amplitude and surface coil. All the patients received intravenous furosemide (10 mg) 30 minutes prior the examination. For the magnetic resonance urography studies, three-dimensional half-Fourier acquisition single-shot turbo spin echo (3D-HASTE) T2-weighted sequences with fat saturation were performed with 2800 ms repetition time, 1080 ms echo time, 512 matrix, 2.0 s acquisition time, and block thickness (slab) ranging between 7 cm and 10 cm to include the whole urinary tract and bladder, at different angles in relation to the transverse axis to obtain anterior, lateral (sagittal) and oblique views. The breathhold acquisition time was short (2.0 s) and, consequently, was well tolerated by the patients. This sequence is the same utilized in magnetic resonance cholangiography. In the evaluation of patients 2 and 5, only the magnetic resonance urography sequence was performed. For the other patients, besides magnetic resonance urography, conventional axial, sagittal and coronal turbo spin echo (TSE) sequences were acquired for evaluation of their pelvic structures. The study of the patients 4 and 6 also included conventional TSE T1-weighted sequences both before and after intravenous contrast agent (gadolinium) administration. The cystoscopy reports, excretory urography and cystography images of the patients also were reviewed and utilized for comparison.
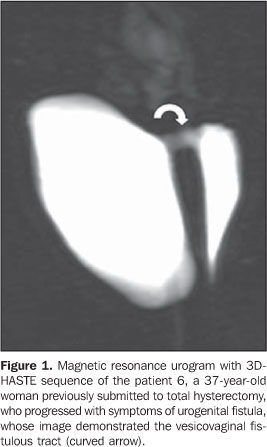
RESULTS Six patients presented vesicovaginal fistulas (patients 1, 2, 4, 5, 6 and 7 – see Table 1); the patient 3 was diagnosed with right-sided ureterovaginal fistula. The fistulous tract could be visualized on magnetic resonance urography images of five (1, 2, 5, 6 and 7 – see table 1) of the six patients diagnosed with vesicovaginal fistulas. The patients 1 and 6 were submitted only to this study (Figure 1), and the patients 2, 5 and 7, besides magnetic resonance urography, also were submitted to cystography (Figures 2 and 3).
The vesicovaginal fistulous tract of the patient 4 could not be visualized on the magnetic resonance urography neither on the conventional magnetic resonance images. However, after intravenous paramagnetic contrast injection, the contrast uptake could be detected in the vaginal vault on the delayed sequences after renal excretion, allowing the diagnosis of urogenital fistula, despite the non-visualization of the fistulous tract. In this patient, the fistulous tract could not be visualized also on the cystography neither on the excretory urography; the fistula orifice was visualized only during cystoscopy. Also in the patients 1, 2 and 6, the vesicovaginal fistula orifice was visualized during cystoscopy. The magnetic resonance urography images of the patient 3 demonstrated a right-sided ureterovaginal fistula (Figure 4). This patient was also submitted to excretory urography, which failed in the diagnosis of the fistula.
Additionally, the patient 4 presented right-sided renal hypotrophy, and the patients 2, 3 and 5, bilateral hydronephrosis. The patient 5 had been previously submitted to bilateral ureteral surgery (uretero-ileal-vesicoplasty), which also could be appropriately demonstrated by magnetic resonance urography (Figure 3).
DISCUSSION Vesicovaginal and ureterovaginal fistulas are infrequent complications secondary to inflammatory diseases, neoplasms, radiotherapy or pelvic surgeries, which cause severe psychosocial problems for affected patients(7). The therapeutic strategies success depends on an appropriate preoperative evaluation for diagnosis and visualization of the fistulous tract. Classically, the imaging methods for evaluation of these fistulas include excretory urography, cystography and vaginography(1). In the last years the increasing utilization of computed tomography urography and magnetic resonance urography for the urinary system evaluation has been reported. Besides demonstrating abnormalities in the urinary tract, these methods allow the visualization of adjacent abdominal and pelvic structures on conventional images. Excretory urography and computed tomography urography present the disadvantage of requiring intravenous iodinated contrast injection and ionizing radiation; for this reason, magnetic resonance imaging is the method of choice for children, pregnant women and patients with any contraindication to iodinated contrast agents, such as previous allergic reaction, severe cardiopathy, asthma or renal failure(9). Magnetic resonance urography allows acquisition of images with a diagnostic quality that has been continuously improved with the development of sequences technically more sophisticated and with increasingly shorter acquisition times(10). Presently, two techniques can be utilized for this study: non-contrast enhanced, T2-weighted sequences (hydrographic sequences), or contrast-enhanced (intravenous paramagnetic contrast – gadolinium – injection) T1-weighted sequences demonstrating contrast excretion(11). Magnetic resonance urography T2-weighted sequence has already proved be an excellent technique for investigating a dilated urinary tract, even in the absence of renal excretion (severe renal failure). T1-weighted sequences with intravenous contrast (gadolinium) injection demonstrate the renal excretory function and the urinary flow through the urinary tract to the bladder(12). Both MR urography techniques may be combined as necessary(13). These techniques have been utilized for investigating congenital anomalies of the urinary system, in the evaluation of hydronephrosis and obstructive uropathies(10,11,14–20). With the utilization of magnetic resonance urography, the fistulous tract could be demonstrated in six of the seven patients evaluated in the present study (85.7%) without the necessity of vesical probing or contrast agent injection. The vesicovaginal fistulous tracts were appropriately demonstrated by magnetic resonance urography in the patients 2, 5 and 7, and the images presented a perfect correlation with cystographic images. In the patients 1 and 6, the fistulous tracts were also appropriately demonstrated on magnetic resonance urography, and the fistulas orifices were visualized on cystoscopy in agreement with the clinical diagnosis, despite de absence of correlation with cystography. The fistulous tract of the patient 4 was not demonstrated by magnetic resonance urography, and also could not be visualized on the cystography, probably because of the narrow caliber and low output of the fistula. Therefore, in four of the patients with vesicovaginal fistulas included in the present study there was a total agreement between the findings on magnetic resonance urography and cystography images; and in the other two patients who were not submitted to radiological study, also there was agreement between the magnetic resonance urography and the clinical diagnosis of urogenital fistula. In the single patient diagnosed with ureterovaginal fistula, the fistulous tract can be perfectly visualized on the magnetic resonance urography sequences confirmed by the conventional TSE sequences, although it could not be appropriately visualized at the excretory urography. So, the magnetic resonance images were decisive for the diagnosis in this patient. Despite the feasibility of urogenital fistula diagnosis by conventional magnetic resonance imaging with multiplanar, thick slices sequences, the magnetic resonance urography with 3D-HASTE sequences allows the acquisition of images quite similar to those usually seem by clinicians and surgeons on conventional radiographic studies (excretory urography, cystography and pyelography, with a broad, non-invasive fast and safe visualization of the whole urinary tract.
CONCLUSION Considering that urogenital fistula is an infrequent condition, the number of patients evaluated in the present study is not sufficient to determine the sensitivity, specificity and accuracy of this diagnostic method. Additional controlled studies with a higher number of patients are necessary to determine conclusive results. However, the images obtained in this study demonstrate the potential capacity and applicability of magnetic resonance urography in the evaluation of urogenital fistulas.
REFERENCES 1. Moon SG, Kim SH, Lee HJ, et al. Pelvic fistulas complicating pelvic surgery or diseases: spectrum of imaging findings. Korean J Radiol. 2001;2:97–104. [ ] 2. Outwater E, Schiebler ML. Pelvic fistulas: findings on MR images. AJR Am J Roentgenol. 1993; 160:327–30. [ ] 3. Murphy JM, Lee G, Sharma SD, et al. Vesicouterine fistula: MRI diagnosis. Eur Radiol. 1999; 9:1876–8. [ ] 4. Semelka RC, Hricak H, Kim B, et al. Pelvic fistulas: appearances on MR images. Abdom Imaging. 1997;22:91–5. [ ] 5. Blomlie V, Rofstad EK, Tropé C, et al. Critical soft tissues of the female pelvis: serial MR imaging before, during, and after radiation therapy. Radiology. 1997;203:391–7. [ ] 6. Kuhlman JE, Fishman EK. CT evaluation of enterovaginal and vesicovaginal fistulas. J Comput Assist Tomogr. 1990;14:390–4. [ ] 7. Akman RY, Sargin S, Ozdemir G, et al. Vesicovaginal and ureterovaginal fistulas: a review of 39 cases. Int Urol Nephrol. 1999;31:321–6. [ ] 8. Tabakov ID, Slavchev BN. Large post-hysterectomy and post-radiation vesicovaginal fistulas: repair by ileocystoplasty. J Urol. 2004;171:272–4. [ ] 9. Kawashima A, Glockner JF, King BF Jr. CT urography and MR urography. Radiol Clin North Am. 2003;41:945–61. [ ] 10. Regan F, Bohlman ME, Khazan R, et al. MR urography using HASTE imaging in the assessment of ureteric obstruction. AJR Am J Roentgenol. 1996;167:1115–20. [ ] 11. Blandino A, Gaeta M, Minutoli F, et al. MR urography of the ureter. AJR Am J Roentgenol. 2002;179:1307–14. [ ] 12. Nolte-Ernsting C, Staatz G, Wildberger J, et al. MR-urography and CT-urography: principles, examination techniques, applications. Rofo. 2003; 175:211–22. [ ] 13. Nolte-Ernsting CC, Staatz G, Tacke J, et al. MR urography today. Abdom Imaging. 2003;28:191–209. [ ] 14. Khanna PC, Karnik ND, Jankharia BG, et al. Magnetic resonance urography (MRU) versus intravenous urography (IVU) in obstructive uropathy: a prospective study of 30 cases. J Assoc Physicians India. 2005;53:527–34. [ ] 15. Chahal R, Taylor K, Eardley I, et al. Patients at high risk for upper tract urothelial cancer: evaluation of hydronephrosis using high-resolution magnetic resonance urography. J Urol.2005;174: 478–82. [ ] 16. Erdogmus B, Bozkurt M, Bakir Z. Diagnostic value of HASTE technique and excretory MR urography in urinary system obstructions. Tani Girisim Radyol. 2004;10:309–15. [ ] 17. Karabacakoglu A, Karakose S, Ince O, et al. Diagnostic value of diuretic-enhanced excretory MR urography in patients with obstructive uropathy. Eur J Radiol. 2004;52:320–7. [ ] 18. Magno C, Blandino A, Anastasi G, et al. Lithiasic obstructive uropathy. Hydronephrosis characterization by magnetic resonance pyelography. Urol Int. 2004;72 Suppl 1:40–2. [ ] 19. Shokeir AA, El-Diasty T, Eassa W, et al. Diagnosis of ureteral obstruction in patients with compromised renal function: the role of noninvasive imaging modalities. J Urol. 2004;171(6 Pt 1): 2303–6. [ ] 20. Blandino A, Minutoli F, Gaeta M, et al. MR pyelography in the assessment of hydroureteronephrosis: single-shot thick-slab RARE versus multislice HASTE sequences. Abdom Imaging. 2003; 28:433–9. [ ]
Received January 23, 2007. Accepted after revision July 13, 2007.
* Study developed in the Departamento de Diagnóstico por Imagem do Hospital de Câncer de Barretos – Fundação Pio XII, Barretos, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554