Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 1 - Jan. /Feb. of 2008
Vol. 41 nº 1 - Jan. /Feb. of 2008
|
ORIGINAL ARTICLE
|
|
Correlation between clinical and imaging findings in patients with temporomandibular disorders |
|
|
Autho(rs): Fábio Augusto Cozzolino, Abrão Rapoport, Sérgio Altino Franzi, Ricardo Pires de Souza, Clemente Augusto de Brito Pereira, Rogério Aparecido Dedivitis |
|
|
Keywords: Magnetic resonance imaging, Temporomandibular joint, Disorders |
|
|
Abstract:
IMaster in Health Sciences, Course of Post-Graduation, Hospital Heliópolis (Hosphel), São Paulo, SP, Brazil
INTRODUCTION Internal temporomandibular joint (TMJ) disorders lead to painful conditions and mandibular dysfunction, as well as symptoms primarily affecting TMJ soft tissues and the articular disk positioning. Imaging methods can significantly contribute to the final diagnosis and therapeutic evaluation in this context. Conventional radiographic methods (panoramic and transcranial radiography) and techniques dedicated to the TMJ (arthrography, arthrotomography, conventional and computed tomography) present some limitations considering the localization, composition and size of the TMJ, besides the level of ionizing radiation exposure. Magnetic resonance imaging (MRI) has revolutionized the diagnosis and treatment of temporomandibular joint disorders (TMJD), because of its high-resolution for demonstrating the TMJ tissues, without necessity of changing the patient's positioning and with no ionizing radiation. MRI has been the method of choice for the diagnosis of abnormalities in the TMJ soft tissues, because of its high accuracy in the determination of the articular disk positioning(1). The present study was aimed at correlating signs and symptoms observed in the clinical assessment of patients diagnosed with TMJD according to the results of MRI.
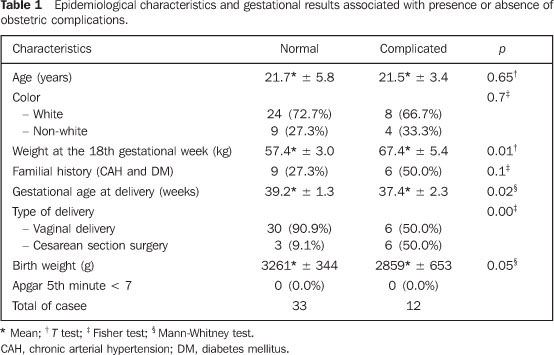
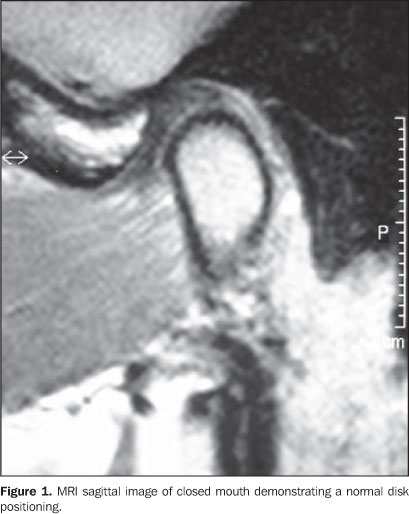
MATERIALS AND METHODS The sample of the present retrospective study included 30 patients referred to the Department of Odontology at Universidade Cruzeiro do Sul, with a diagnosis of TMJD, in the period between January 2002 and January 2006. This project was approved by the Committee for Ethics in Research of Universidade Cruzeiro do Sul, under the number 036/05. Inclusion criteria were: patients diagnosed with TMJD presenting headache, otalgia, pre-auricular and orofacial pain. Exclusion criteria were patients below the age of 18 and previously submitted to surgery for treating TMJD. The MRI studies were independently interpreted by two experienced radiologists who elaborated the diagnostic reports according to the criteria established by Nebbe et al.(2) (Table 1; Figures 1 and 2). In case of disagreement between these diagnostic reports, the final diagnosis was achieved by consensus between both radiologists.
The disease indicators consisted in a questionnaire developed by the American Academy of Orofacial Pain – Guidelines for Assessment, Diagnosis and Management of temporomandibular Joint Disorder(3). The main complaint was obtained by means of an interview as the initial step of the clinical evaluation. Then, the presence of articular pain was evaluated by means of both lateral and posterior palpation of the TMJ and auscultation for articular sounds (clicking and crepitus). The presence of muscular pain was evaluated by bilateral, extraoral palpation of the following muscles or regions: superficial masseter, deep masseter, temporal anterior, temporal posterior, frontal, vertex, posterior cervical regions, digastric and sternocleidomastoid; and intraoral palpation of temporalis, pterygoid and lateral pterygoid. According to previous studies(4–6), temporomandibular joint clicking or popping sounds are brief noises which occur in some points during opening, closing or lateral movements; and crepitus is a mildly perceptible grating sound, suggestive of subchondral sclerosis. MRI studies were performed in a 1.5 tesla Gyroscan ACS-NT apparatus (Philips; Amsterdam, Holland). Twelve 3 mm-thick slices were acquired with surface coil, on coronal T1-weighted sequences (400/20 ms, FOV = 19 cm) with the patient's mouth closed; on sagittal, T1-weighted sequences (400/20 ms, FOV = 19 cm) with the patient's mouth opened and closed, and T2-weighted sequences (2670/15 ms, FOV = 19 cm) during progressive mouth opening and closing (three positions: maximum, intermediate opening and closed mouth), at 5 mm intervals and 30° flip angle to obtain the cine effect in an attempt to reproduce the whole extent of the mandibular movement, with dynamic video images. All the images were acquired with the patient in dorsal decubitus. Descriptive statistics was utilized for summarizing the data regarding sex and age range, facial pain, articular sounds and disk positioning at MRI. The correlation between MRI and facial pain and articular sounds was based on MRI versus clinical findings respectively on the right and left sides. The statistical significance of the clinical assessment of patients with TMJD and MRI findings was evaluated with the kappa test for determining the correlation level.
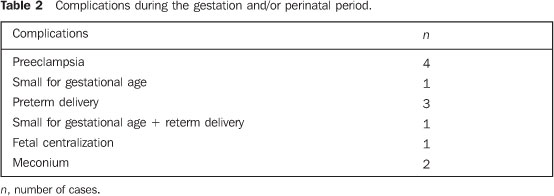
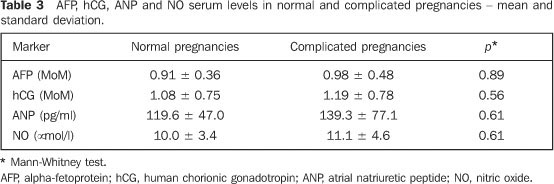
RESULTS A female predominance was observed (24 patients), with a women/men ratio equal to 3.2:1, and higher incidence in the age range between 18 and 29 years (41.7% of the patients). As regards painful symptoms, 14 patients (46.7%) presented bilateral pain, 4 (13.3%), right-sided pain, 3 (10.0%), left-sided pain, and 9 patients (30.0%) had no pain-related complaint. As regards the presence or absence of articular sounds, the right side was affected in 7 patients (23.3%), the left side in 7 (23.3%), both sides in 6 (20.0%), and absence of this symptom was observed in 10 (33.3%). The incidence of the different articular sounds was the following: on the left side — clicking in 12 patients (40.0%), crepitus in 1 (3.3%), and absence in 17 (56.7%); on the right side — clicking was observed in 12 patients (40.0%), crepitus in 1 (3.3%) and absence in 17 (56.7%). Table 2 shows the frequency of articular alterations and distribution related to their side according to the MRI diagnostic reports. Tables 3 and 4 present the frequency of articular alterations as well as the incidence in both sides of each type of alteration according to the MRI diagnostic reports. Table 5 shows the relation between the clinical and the MRI diagnosis of left-sided disk displacement while the right-sided findings are shown on Table 6.
DISCUSSION An attempt was made to combine the utilization of MRI (the method of choice for evaluating TMJ) with a clinical questionnaire. MRI is considered as the method of choice for evaluating the TMJ functioning, because of its non-invasiveness and absence of collateral effects, besides the high accuracy comparable to arthrography for visualizing functioning structures. However, the association of clinical and imaging findings is essential for an accurate diagnosis and prognostic evaluation of TMJD(4). Data collected by means of the anamnesis and clinical examination of the patients constitutes the basis for a correct diagnosis of TMJD(7). A high interobserver agreement was observed in the evaluation of TMJD by MRI, corroborating the acceptance and reliability of this diagnostic method(8–12). Many times, the clinicians are not aware of the actual nature of TMJD, as their diagnosis is based only on clinical findings(13). However, they should be aware of the imaging methods both for recommending and interpreting them. The female prevalence observed in this group is similar to the one demonstrated in other study about TMJD(14), which has evaluated 73 patients (56 women and 17 men). The patients were evaluated according to the distribution of the facial pain, and the most frequent type of facial pain occurred in both sides para 14 patients (46.7%), similarly to data described in other casuistics of TMJD(15). A study about morphological alterations of the styloid process in patients with TMJD demonstrated their presence in 74 female and 9 male patients concentrated in the age range between 41 and 50 years (32.5%)(16). A descriptive analysis demonstrated that the presence of clicking was the most frequent clinical finding — 20 cases (63.3%), 14 (46.6%) of them unilateral and six (20%) bilateral — while another study(17) with 98 patients demonstrated unilateral articular sound in 60% of cases and bilateral in 40%.. On Table 2, it can be observed that, most frequently, articular alterations occurred in both sides in a total of 13 patients, similarly to the results of another study(18). In 34 cases (70%) some type of TMJ alteration was found at MRI, the most frequent one being anterior displacement with mild reduction in 19 cases (Tables 3 and 4). In another study(19) 37.3% of the patients were diagnosed with mild disk displacement by MRI, while 74.4% presented a severe disk displacement. The correlation between right-sided MRI results and clinical diagnosis of right-sided disk displacement (Tables 5 and 6) demonstrated that of 12 patients (100%) who had normal MRI studies, nine (83.3%) had clinical diagnosis of disk displacement. Also on the right side, 18 patients (100%) were diagnosed with disk displacement by MRI, 15 of them (83.3%) with clinical diagnosis of disk displacement. Interobserver agreement for the right side was 56.7% (kappa = 0 and p = 1). On the left side, of 14 patients (100%) who had a normal MRI study, 10 (71.4%) were clinically diagnosed with disk displacement, and, of 16 patients (100%) with MRI results positive for disk displacement, 13 (81.3%) were clinically diagnosed with disk displacement. The interobserver agreement for the left side was 56.7% (kappa = 0.1 and p = 0,526). Similar results have been obtained in a study of 46 patients with disk displacement with reduction compared with clinical assessment, with an interobserver agreement of 40.7% and kappa = 0.2(20). Based on these results, it can be observed that the presence of MRI findings does not correspond to the presence of painful symptoms and vice-versa. Pain is an extremely individualized experience, whose threshold is quite variable among patients. The type or site of the pain may correspond to different etiological factors. In the case of TMJD, several factors may lead to painful symptoms. Notwithstanding, a high incidence of asymptomatic patients affected by disk displacement with and without reduction (33%) is observed. But there is a prevalence of symptomatic patients, representing up to 77% of cases with disk displacement(21,22). The present study demonstrated a high incidence of patients symptomatic for TMJD (19 TMJs) with no MRI finding. Individual observation of the MRI studies demonstrated the following situations: patients with clicking, but with MRI showing a normal disk positioning without displacement; and patients with clicking, and with MRI findings of anterior displacement with or without reduction. In another series, correlation has not been observed between the degree of disk displacement and pain at palpation of masticatory muscles, articular sounds or occlusal findings(23) neither between symptoms severity and degree of disk displacement(24). However, another series shows a significant relationship between MRI images and clinical evaluation(25). Another study of patients submitted to MRI(26) has correlated clicking with normal disk positioning in 36% of TMJs, and with anterior displacement with reduction in 82%, concluding that the clinical diagnosis of clicking cannot be considered as a rule for determining the presence and type of disk displacement. Although this is a frequent finding in patients with suspicion for TMJD, clicking should not be considered as a pathognomonic sign of disk displacement, considering that it was found in only 53% of these patients, with only 7% of crepitus(27). The present study demonstrated that the presence of clinical signs, clicking or crepitus is not sufficient for the diagnosis of anterior disk displacement.
REFERENCES 1. Ramos ACA, Sarmento VA, Campos PSF, et al. Articulação temporomandibular – aspectos normais e deslocamentos de disco: imagem por ressonância magnética. Radiol Bras. 2004;37:449–54. [ ] 2. Nebbe B, Brooks SL, Hatcher D, et al. Magnetic resonance imaging of the temporomandibular joint: interobserver agreement in subjective classification of disk status. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:102–7. [ ] 3. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–55. [ ] 4. Manfredini D, Tognini F, Zampa V, et al. Predictive value of clinical findings for temporomandibular joint effusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:521–6. [ ] 5. Lobo LFL, Nunes LJ. ATM: diagnóstico e tratamento. São Paulo: Pancast; 2000. [ ] 6. Prado SD, Pereira HP, Gonçalves A. Ruídos articulares: métodos de detecção e tratamento. Rev Serv ATM. 2003;3:60–5. [ ] 7. Brasileiro CB, Cardoso VN, Ruckert B, et al. Avaliação de processos inflamatórios na articulação temporomandibular empregando leucócitos autólogos marcados com tecnécio-99m em modelo animal. Radiol Bras. 2006;39:283–6. [ ] 8. Brandlmaier I, Grüner S, Rudisch A, et al. Validation of the clinical diagnostic criteria for temporomandibular disorders for the diagnostic subgroup of degenerative joint disease. J Oral Rehabil. 2003;30:401–6. [ ] 9. Taskaya-Yilmaz N, Ogütcen-Toller M. Clinical correlation of MRI findings of internal derangements of the temporomandibular joints. Br J Oral Maxillofac Surg. 2002;40:317–21. [ ] 10. Liedberg J, Panmekiate S, Petersson A, et al. Evidence-based evaluation of three imaging methods for the temporomandibular disc. Dentomaxillofac Radiol. 1996;25:234–41. [ ] 11. Raustia AM, Pyhtinen J, Tervonen O. Clinical and MRI findings of the temporomandibular joint in relation to occlusion in young adults. Cranio. 1995;13:99–104. [ ] 12. Sano T, Westesson PL. Magnetic resonance imaging of the temporomandibular joint. Increased T2 signal in the retrodiskal tissue of painful joints. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:511–6. [ ] 13. Pharoah MJ. The prescription of diagnostic images for temporomandibular joint disorders. J Orofac Pain. 1999;13:251–4. [ ] 14. Taskaya-Yilmaz N, Ogütcen-Toller M. Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J Oral Maxillofac Surg. 2001;59:860–6. [ ] 15. Tanaka EE. Análise dos efeitos da terapia com placas estabilizadoras em pacientes com disfunções têmporo-mandibulares por meio da ressonância magnética. (Tese de Doutorado). São Paulo: Universidade de São Paulo; 2000. [ ] 16. Guimarães SMR, Carvalho ACP, Guimarães JP, et al. Prevalência de alteração morfológica do processo estilóide em pacientes com desordem temporomandibular. Radiol Bras. 2006;39:407–11. [ ] 17. Milano V, Desiate A, Bellino R, et al. Magnetic resonance imaging of temporomandibular disorders: classification, prevalence and interpretation of disc displacement and deformation. Dentomaxillofac Radiol. 2000;29:352–61. [ ] 18. Barclay P, Hollender LG, Maravilla KR, et al. Comparison of clinical and magnetic resonance imaging diagnosis in patients with disk displacement in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:37–43. [ ] 19. Takaku S, Sano T, Yoshida M, et al. A comparison between magnetic resonance imaging and pathologic findings in patients with disc displacement. J Oral Maxillofac Surg. 1998;56:171–7. [ ] 20. Emshoff R, Innerhofer K, Rudisch A, et al. Clinical versus magnetic resonance imaging findings with internal derangement of the temporomandibular joint: an evaluation of anterior disc displacement without reduction. J Oral Maxillofac Surg. 2002;60:36–43. [ ] 21. Katzberg RW, Westesson PL, Tallents RH, et al. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996;54:147–55. [ ] 22. Kurita H, Ohtsuka A, Kobayashi H, et al. Is the morphology of the articular eminence of the temporomandibular joint a predisposing factor for disc displacement? Dentomaxillofac Radiol. 2000;29:159–62. [ ] 23. Augthun M, Müller-Leisse C, Bauer W, et al. Anterior disk displacement of the temporomandibular joint. Significance of clinical signs and symptoms in the diagnosis. J Orofac Orthop. 1998;59: 39–46. [ ] 24. Tenenbaum HC, Freeman BV, Psutka DJ, et al. Temporomandibular disorders: disc displacements. J Orofac Pain. 1999;13:285–90. [ ] 25. Toyama M, Kurita K, Koga K, et al. Magnetic resonance arthrography of the temporomandibular joint. J Oral Maxillofac Surg. 2000;58:978–84. [ ] 26. Bell KA, Miller KD, Jones JP. Cine magnetic resonance imaging of the temporomandibular joint. Cranio. 1992;10:313–7. [ ] 27. Cholitgul W, Nishiyama H, Sasai T, et al. Clinical and magnetic resonance imaging findings in temporomandibular joint disc displacement. Dentomaxillofac Radiol. 1997;26:183–8. [ ]
Received December 20, 2006. Accepted after revision June 4, 2007.
* Study developed at Hospital Heliópolis (Hosphel), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554