Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 2 - Mar. / Apr. of 2009
Vol. 42 nº 2 - Mar. / Apr. of 2009
|
ICONOGRAPHIC ESSAY
|
|
Epidural cystic masses associated with interspinous bursitis, synovial and discal cysts |
|
|
Autho(rs): Frederico Guilherme de Paula Lopes Santos, Ricardo André de Souza, Marcos Pama D'Almeida Brotto, Fábio Massaaki Suguita, Denise Tokechi Amaral, Lázaro Luís Faria do Amaral |
|
|
Keywords: Magnetic resonance imaging, Spinal cord compression, Spinal cord disease |
|
|
Abstract:
IMDs, Residents at MedImagem - Hospital Beneficência Portuguesa de São Paulo, São Paulo, SP, Brazil
INTRODUCTION The differentiation between pathological intramedullary conditions (originated in the spinal cord) and extramedullary lesions (external to the thecal sac [extradural] or restricted to the thecal sac [intradural]) is generally simple. Although many lesions can develop simultaneously in more than one compartment, their precise positioning in relation to the medullary canal and the evaluation of the signal characteristics at magnetic resonance imaging (MRI) may be useful for the diagnosis. MRI is the method of choice for evaluating the spinal cord and surrounding tissues because of its high spatial resolution, allowing optimum visualization of internal structures and anatomic detail for more accurate detection and characterization of spinal lesions(1). Epidural cystic masses represent one of the causes for vertebral canal stenosis or lumbar sciatic pain. Although not frequently found, these lesions should be differentiated from neurogenic tumors and disc herniation. The present pictorial essay discusses imaging findings and describes the characteristics of an array of extradural cystic lesions with the utilization of MRI.
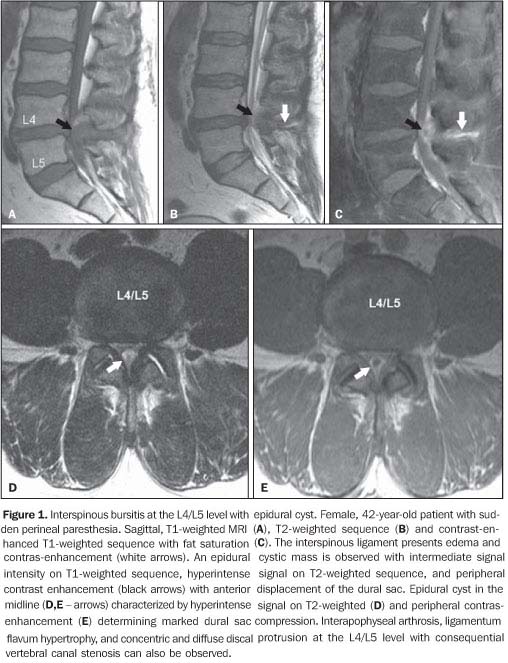
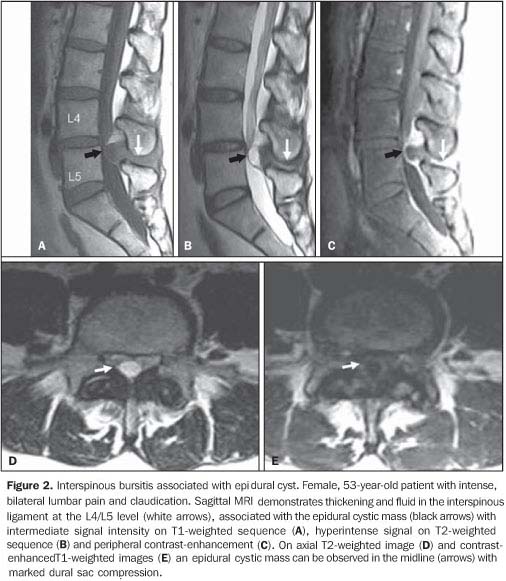
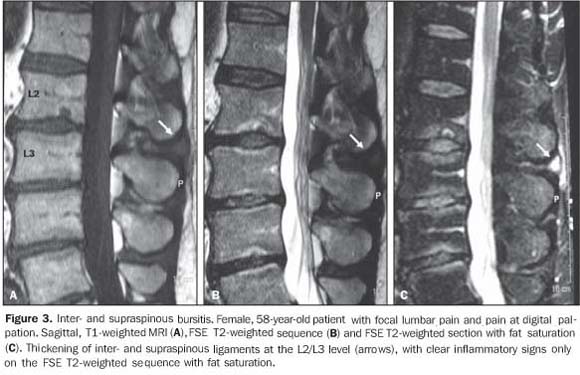
CYSTS RELATED TO INTERSPINOUS BURSITIS Autopsy studies demonstrate an increase in the incidence of cysts secondary to bursitis between lumbar spinous processes in elder individuals. Symptoms are characterized by localized pain in the lower portion of the lumbar spine exacerbated by hyperextension. In young athletes, these symptoms may mimic spondylolysis. MRI is useful in the detection of thickening and hyperintense signal of interspinous and supraspinous ligaments, as well as the formation of adventitial bursae secondary to attrition. Epidural cysts present the same characteristics of synovial cysts, but are localized in the midline. Radioscopy- or computed tomography (CT)-guided bursography can be utilized for diagnosis confirmation. Besides determining the connection with the epidural cyst, this method allows the pain management with corticoid infiltration(2).
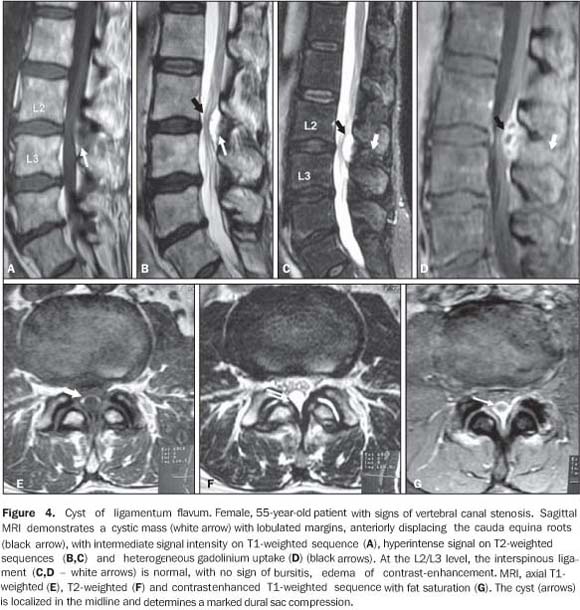
CYST OF LIGAMENTUM FLAVUM Cysts of ligamentum flavum are rare entities and, like synovial cysts and cysts of the posterior longitudinal ligament, are classified as juxtafacet cysts. Because of the absence of synovial membrane on their walls, they are considered as pseudocysts(3), resulting from degenerative alterations and spondylolisthesis, arising from the anterior margin of the ligamentum flavum(4). Anterior projection of the lesion may determine dural sac compression or vertebral canal stenosis, resulting in sciatic pain(5). At MRI, the mass is seen with hypointense signal on T1-weighted, and hyperintense signal on T2-weighted sequences, with peripheral contrast-enhancement, and usually located in the midline. These lesions should be differentiated from synovial cysts by the topographic relation with the interapophyseal joint(6).
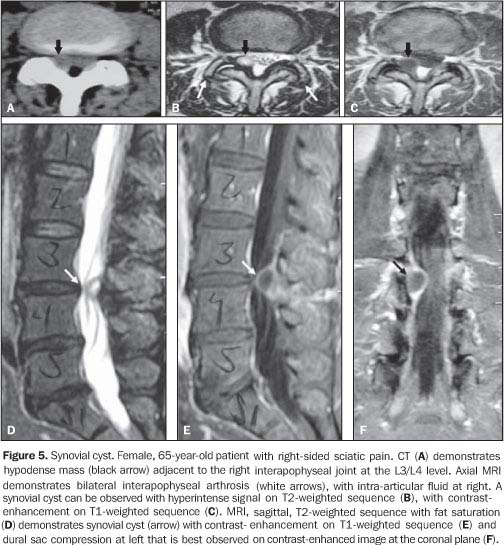
SYNOVIAL CYSTS These cysts may develop from any joint lined by synovial membrane or tendinous sheath, and are rarely seen on the vertebral spine, the L4-L5 transition being the preferential site of these lesions. There is a subtle predominance of these lesions in women, rarely appearing before the age of 30(7).
Synovial cysts are associated with osteoarthrosis, spondylolisthesis and abnormal displacement of interapophyseal joints. These lesions result from a herniation of the joint tissue through a defect of the capsule(7,8) and present a layer of synovial cells at histologic(9). Synovial cysts may be asymptomatic or, depending on their size and site, may cause symptoms of nervous compression, sciatic pain, simulating disc herniation. At CT, synovial cysts are seen as hypoattenuating lesions adjacent to the joint facet, protruding into the epidural space and determining radicular and dural sac compression. In 30% of cases, peripheral calcification and intracystic gas can be observed(9). At MRI, synovial cysts present intermediate signal intensity on T1-weighted sequences, hyperintense signal on T2-weighted with a hypointense capsule. The signal intensity may be heterogeneous as a result of hemorrhages, calcifications and spinal vacuum phenomena(6), which are better visualized at CT(10). After gadolinium injection, peripheral contrast enhancement of the cyst and adjacent interapophyseal joint is observed(9). Improvement of symptoms may be achieved by means of radioscopically or CT-guided intra-articular corticosteroid injection, postponing or even replacing the surgical procedure(7,9). Surgical decompression is indicated in the presence of refractory pain or other associated neurological symptoms.
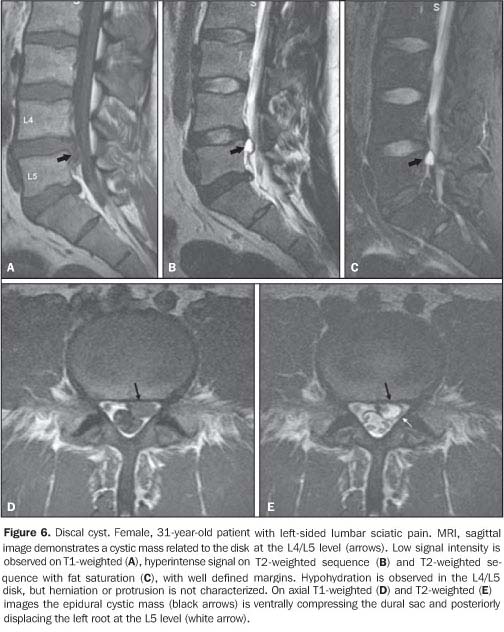
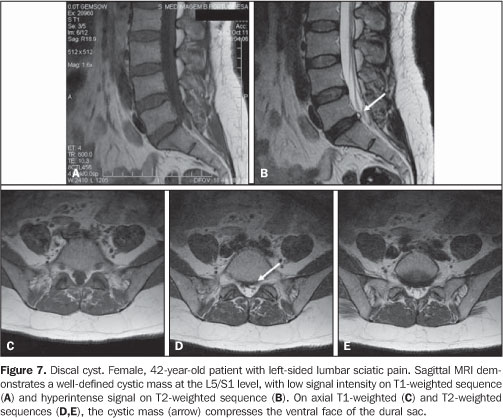
DISCAL CYSTS Discal cysts are extradural, well-defined, homogeneous masses adjacent to a herniated or non-herniated intervertebral disc. These lesions are characterized by hyperintense signal similar to liquor and peripheral contrast-enhancement. Communication with the intervertebral disc may be observed, particularly at CT-discography(11).
Two theories try to explain the development of discal cysts. According to the first one, the cyst would originate from an extradural hematoma secondary to rupture of an epidural vein determined by mechanical irritation of a discal herniation(12). This theory is defended by its authors, considering the presence of hematic content in four of the seven cases reported(12). Extradural hematomas have been reported in the literature(13) with findings similar to discal cysts although without a documented communication with adjacent intervertebral disc. The other theory refers to focal degeneration with softening of the collagen connective tissue and discal fluid leakage with formation of a pseudocapsule. According to some authors, these cysts can be erroneously diagnose or even treated as epidural hematomas or synovial cysts. The treatment for this lesion is surgical excision(11).
CONCLUSION Several types of cystic formations with different physiopathological mechanisms may affect the vertebral canal. The presence of epidural cysts must be more frequent than suggested by the few reports found in the literature. These clinical entities should be considered as possible causes for myelopathy and radiculopathy(14). Other causes for vertebral canal stenosis or lumbar sciatic pain, such as, for example, neurogenic tumors and disc herniation, should be ruled out. Magnetic resonance imaging is the main tool for the diagnosis of extradural cystic lesions(15).
REFERENCES 1. Evans A, Stoodley N, Halpin S. Magnetic resonance imaging of intraspinal cystic lesions: a pictorial review. Curr Probl Diagn Radiol. 2002;31: 79-94. [ ] 2. Chen CKH, Yeh LR, Resnick D, et al. Intraspinal posterior epidural cysts associated with Baas-trup's disease: report of 10 patients. AJR Am J Roentgenol. 2004;182:191-4. [ ] 3. Asamoto S, Jimbo H, Fukui Y, et al. Cyst of the ligamentum flavum: case report. Neurol Med Chir. 2005;45:653-6. [ ] 4. Baker JK, Hanson GW. Cyst of the ligamentum flavum. Spine. 1994;19:1092-4. [ ] 5. Vernet O, Fankhauser H, Schnyder P, et al. Cyst of the ligamentum flavum: report of six cases. Neurosurgery. 1991;29:277-83. [ ] 6. Mahallati H, Wallace CJ, Hunter KM, et al. MR imaging of a hemorrhagic and granulomatous cyst of the ligamentum flavum with pathologic correlation. AJNR Am J Neuroradiol. 1999;20:1166-8. [ ] 7. Rosa ACF, Machado MM, Figueiredo MAJ, et al. Cistos sinoviais lombares. Radiol Bras. 2002;35: 299-302. [ ] 8. Hsu KY, Zucherman JF, Shea WJ, et al. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine. 1995;20:80-9. [ ] 9. Bureau NJ, Kaplan PA, Dussault RG. Lumbar facet joint synovial cyst: percutaneous treatment with steroid injections and distention - clinical and imaging follow-up in 12 patients. Radiology. 2001;221:179-85. [ ] 10. Hagen T, Daschner H, Lensch T. Juxta-facet cysts: magnetic resonance tomography diagnosis. Radiologe. 2001;41:1056-62. [ ] 11. Kono K, Nakamura H, Inoue Y, et al. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR Am J Neuroradiol. 1999;20:1373-7. [ ] 12. Toyama Y, Kamata N, Matsumoto M. Pathogenesis and diagnostic title of intraspinal cyst communicating with intervertebral disk in the lumbar spine. Rinsho Seikei Geka. 1997;32:393-400. [ ] 13. Gundry CR, Heithoff KB. Epidural hematoma of the lumbar spine. 18 surgically confirmed cases. Radiology. 1993;187:427-31. [ ] 14. Shima Y, Rothman SL, Yasura K, et al. Degenerative intraspinal cyst of the cervical spine. case report and literature review. Spine. 2002;27:E18-22. [ ] 15. Robinson Y, Reinke M, Haschtmann D, et al. Spinal extradural meningeal cyst with spinal stenosis. Spinal Cord. 2006;44:457-60. [ ] Received November 6, 2008. * Study developed at MedImagem - Hospital Beneficência Portuguesa de São Paulo, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554