Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 1 - Jan. /Feb. of 2009
Vol. 42 nº 1 - Jan. /Feb. of 2009
|
CASE REPORT
|
|
Sarcomatous degeneration of Paget's disease in the calcaneus: a case report |
|
|
Autho(rs): Simone Berwig Matiotti, Conrado Silva Tramunt, Rogério Dias Duarte, Rodrigo Dias Duarte, Wolmir Lourenço Duarte, Janine Bernardi Soder |
|
|
Keywords: Paget's disease, Sarcoma, Sarcomatous degeneration, Calcaneus, Osteitis deformans |
|
|
Abstract:
IMDs, Radiologists, Clínica Serdil, Porto Alegre, RS, Brazil
INTRODUCTION Paget's disease, firstly described by Sir James Paget in 1877 as osteitis deformans, is characterized by findings of a disturbed and extremely active bone remodeling caused by reactive osteoclastic and osteoblastic activity, in a peculiar mosaic pattern(1,2). The cause for this disease still remains unknown, the viral etiology theory being the most accepted among others such as genetic origin, parathormone-induced metabolic disorder, autoimmune disease, vascular disease, conjunctive disease tissue, or even neoplastic process(3-5). Sarcomatous degeneration is rare, occurring in approximately 1% of cases of long-term disease activity(1). Osteosarcoma is the most frequently found histologic type of tumor (50-60% of cases). Most frequently, pelvis, hip or shoulder are affected(1,3,4), calcaneal involvement, like in the present case, being extremely rare(6).
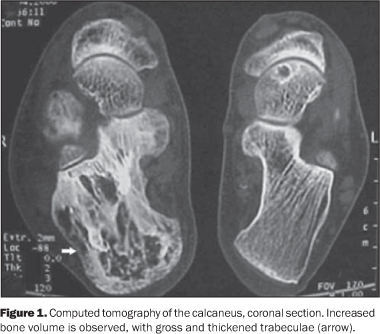
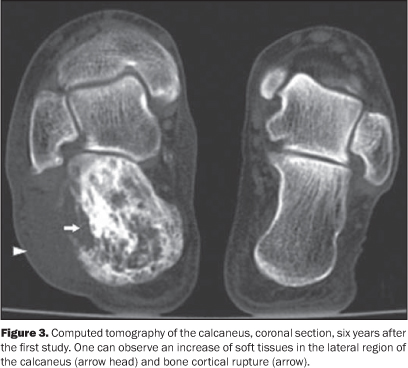
CASE REPORT The present study reports the case of a male, 85-year-old patient with history of bone Paget's disease for several years, and reporting pain and swelling in the right calcaneal region for three months. The first computed tomography (CT) study performed six years before (Figure 1) demonstrated characteristic findings of Paget's disease. Bone scintigraphy (Figure 2) and a new CT (Figure 3) were performed and demonstrated a significant increase in radiopharmaceutical uptake and subtle increase in bone volume, with cortical bone rupture on the lateroposterior surface of the calcaneus. Magnetic resonance imaging (MRI) demonstrated a volumetric increase, with heterogeneous signal intensity on all sequences, and some cystic and sclerotic areas. Cortical bone rupture and a mass in soft tissues of the lateral calcaneal region were observed, with peripheral contrast enhancement after gadolinium injection (Figure 4), and alterations suggesting malignant degeneration. The patient was submitted to biopsy of the lesion, whose result evidenced high-grade osteosarcoma.
DISCUSSION Paget's disease affects approximately 3-4% of the population aged above 40 years(1-3,7). Most frequently, the axial skeleton (pelvis, spine and skull) is involved, but proximal long bones also can be frequently affected (25-35% of cases)(1,3,4,7). Involvement of other structures such as rips, fíbula, hand and feet bones, calcaneus and patella is not frequent(1,4,7). The polyostotic presentation represents 65-90% of cases. Involvement of an appendicular segment is generally unilateral(1,3,7). In most of cases, diagnosis can be reached by means of radiological examination, presenting characteristic findings(2,8). These findings depend on the disease stage. At the osteolytic phase, radiolucent areas with well-defined margins are observed, with absence of areas of bone sclerosis. The mixed phase of the disease is characterized by the presence of gross and thickened trabeculae, as well as cortical bone thickening reflecting osteoblastic activity. The blastic phase is characterized by the presence of sclerotic areas and increased bone volume(2,3). Bone scintigraphy is a sensitive method, but poorly specific in the detection of hyperemia and osteoblastic activity, and can detect an increase in radionuclide uptake even before radiological findings become evident(3,7). Sometimes, the disease may be incidentally found at CT or MRI(9). Tomographic findings are similar to the radiographic ones, and trabecular thickening can be better depicted by CT(2,3,8). Three patterns of bone marrow images can be identified at MRI. In most of cases the yellow bone marrow presents normal signal intensity. In many cases the medullary space of the bone affected presents a larger amount of fat than a normal bone, which represents medullary atrophy. The volume of the medullary canal may be reduced by the thickening of the cortical layer(3). The second pattern identified presents heterogeneous signal intensity on T1- and T2-weighted sequences. On T1-weighted sequences, the bone marrow presents decreased signal intensity, with intermingled foci of normal bone marrow which rules out the presence of malignant degeneration by the absence of masses. On T2-weighted sequences the bone marrow signal is heterogeneously hyperintense(3,9). The third pattern is observed in the phase of decreased blastic activity, with low bone marrow signal intensity on all the sequences, corresponding to sclerosis. With the utilization of intravenous gadolinium as a contrast agent, a medullary enhancement can be observed, particularly at the most active phases of the disease(3). Sarcomatous degeneration is rarely observed, occurring in approximately 1% of cases of long-term disease activity. The highest risk is observed in patients with polyostotic disease(1,3,4,7). Swelling and pain in the region affected are symptoms indicative of this condition(1,3). The most common histologic type of lesion is osteosarcoma (50-60% of cases), besides cases of malignant fibrotic histiocytoma/fibrosarcoma and chondrosarcoma(1,3,6,10). The prognosis for patients with sarcomatous degeneration is poor, with less than 10% for three-year disease-free survival after treatment(11). Metastases, particularly the pulmonary ones, are frequent(10). Typical signs of sarcomatous degeneration are aggressive bone lysis, cortical destruction and presence of soft tissue masses(1,4,7). In most of cases, periosteal reaction is not observed(4). Neoplastic degeneration in bones affected by Paget´s disease may be hardly radiologically detected, requiring comparison with previous radiographies for identifying new osteolytic areas besides further studies by CT and MRI(3). MRI is superior to CT, allowing the visualization of replacement of bone marrow by tumor cells and cortical destruction in association with relatively large and infiltrating soft tissues mass. Sarcomatous degeneration is observed with intermediate signal intensity on T1-weighted images, with enhancement after gadolinium injection, and hyper-intense signal on T2-weighted images. Central necrosis is frequently found(1,3).
CONCLUSION Malignant bone degeneration is rarely observed in Paget's disease. However, in these cases, the main histologic types identified are osteosarcoma (50-60%) and malignant fibrotic histiocytoma/ fibrosarcoma (20-25%) and chondrosarcoma. Clinically, the findings that characterize malignant transformation are soft tissues swelling in the affected region, and radiologically, the presence of soft tissue mass and cortical bone destruction. In the suspicion of Paget's disease, CT and MRI should be performed for findings characterization, even in bones were this disease is extremely rare, such as the calcaneus. Despite the CT superiority for demonstrating cortical breakdown and changes in the bone trabecular pattern, MRI also allows the identification of changes in the signal intensity produced by bone marrow and adjacent soft tissues.
REFERENCES 1. Resnick D, Niwayama G. Paget disease. In: Resnick D, editor. Diagnosis of bone and joint disorders. 4th ed. Philadelphia: Saunders; 2002. p. 1947-2000. [ ] 2. Greenspan A. Radiologia ortopédica. 3ª ed. Rio de Janeiro: Guanabara Koogan; 2001. [ ] 3. Smith SE, Murphey MD, Motamedi K, et al. From the archives of the AFIP. Radiologic spectrum of Paget disease of bone and its complications with pathologic correlation. Radiographics. 2002;22: 1191-216. [ ] 4. Merkow RL, Lane JM. Paget's disease of bone. Orthop Clin North Am. 1990;21:171-89. [ ] 5. Mirra JM, Brien EW, Tehranzadeh J. Paget's disease of bone: review with emphasis on radiologic features, part I. Skeletal Radiol. 1995;24:163-71. [ ] 6. de Waele S, Lonneux M, Vande Berg B, et al. Paget disease and osteosarcoma of the calcaneus. Clin Nucl Med. 2001;26:244-6. [ ] 7. Resnick D. Paget disease of bone: current status and a look back to 1943 and earlier. AJR Am J Roentgenol. 1988;150:249-56. [ ] 8. Pinho MC, Lima GAF, Rodrigues MB. Qual o seu diagnóstico? (Osteossarcoma periosteal). Radiol Bras. 2005;38(6):vii-ix. [ ] 9. Boutin RD, Spitz DJ, Newman JS, et al. Complications in Paget's disease at MR imaging. Radiology. 1998;209:641-51. [ ] 10. Smith J, Botet JF, Yeh SDJ. Bone sarcomas in Paget disease: a study of 85 patients. Radiology. 1984;152:583-90. [ ] 11. Wick MR, Siegal GP, Unni KK, et al. Sarcomas of bone complicating osteitis deformans (Paget's disease): fifty years' experience. Am J Surg Pathol. 1981;5:47-59. [ ] Received February 7, 2007. * Study developed at Fundação Saint Pastous, Clínica Serdil, Porto Alegre, RS, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554