Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 1 - Jan. /Feb. of 2009
Vol. 42 nº 1 - Jan. /Feb. of 2009
|
ORIGINAL ARTICLE
|
|
Correlation among scapular positioning, functional postural analysis and upper extremities disability degree in sonographers (DASH Brazil) |
|
|
Autho(rs): Geraldo Fabiano de Souza Moraes, Fernanda Moreira Gonçalves, Júnia Darth Silva, Natália Spindola Soares |
|
|
Keywords: Biomechanics, Shoulder joint complex, Scapular positioning, Scapulohumeral rhythm, Sonographer |
|
|
Abstract:
IMaster, Physiotherapist, Associate Professor and Coordinator for the Course of Physiotherapy, Centro Universitário Newton Paiva, Belo Horizonte, MG, Brazil
INTRODUCTION Currently, there is a great concern about preventing diseases and lesions involving the shoulder joint as a result from postural alterations and that lead to musculoskeletal system compensation to the detriment of the functionality(1). The prevalence of shoulder pain in association with disability is present in about 20% of the general population(2). Multifactorial situations cause overload of this joint complex, as follows: marked repetitiveness of movements; upper limb positioning, especially with shoulder abduction; muscular fatigue; work organization factors and annulling of mechanisms of work regulation, such as overload (reduction or lack of intervals) and psychosocial factors which generate tension and stress(3). One has observed the relevance of perception for the quality of life and health of a great part of the population which are frequently impaired by acute and chronic musculoskeletal disorders(4). The association of scapular and humeral movements allows amplitude of the movement of flexion and abduction of the arm between 150° and 180°. The typical mobility in asymptomatic individuals generally occurs with 2° of glenohumeral movement for 1° of scapular rotation, determining a 2:1 ratio for the scapulohumeral rhythm(5,6). Several athletes, particularly swimmers(7), and practitioners whose activities involve abduction of the upper limbs present a higher predisposition to develop alterations in the mobility-stability relationship(8). For example, the professional activity of the sonographer is characterized by the high probability of altered mobility-stability relationship because of long-lasting sustained upper limb abduction(9,10). Diagnosis by ultrasonography is a relatively new medical activity introduced early in the 1940's(9). With the introduction of new technologies and the recognition of the ultrasound diagnostic capabilities, the number of US procedures and examination times have increased from year to year(9,10). Despite technological developments allowing the acquisition of high-resolution images, ergonomic conditions observed during examinations are not so favorable for the musculoskeletal system of the sono-grapher(11). Approximately 80% of these practitioners report discomfort or incapacity to perform an appropriate examination because of the presence of symptoms in their upper limbs. One of the factors that apparently interferes in the origin of symptoms experimented by the sonographer is the high number US examinations which started being performed on a routine basis, besides risks resulting from electric shock, low illumination levels, stress and musculoskeletal overload in upper limbs and vertebral spine(2,12). Static and dynamic overloads imposed on the muscles of the scapular cingulum and on the upper limbs occur as a result from the necessity of sustaining the shoulder abduction for a better function of the wrist and hand as the transducer is positioned perpendicularly to the skin of the patient over the examination(2,9,11,13). Impairment of the functionality and time spent by the professional away from his/her daily activities leads to an overload of the health system in several countries. It is important that preventive measures be developed and for this purpose it is necessary to identify and understand the occupational overload and its consequences in order to minimize the effects on the functional capacity of the individual(1). Although it is recognized that occupational diseases result from a set of three factors, namely, physical load, psychological load, and cognitive load, the present study was aimed primarily at evaluating and measuring the scapular positioning and correlating it with the degree of upper limbs disability and postural functional analysis of sonographers, focusing on their physical workload.
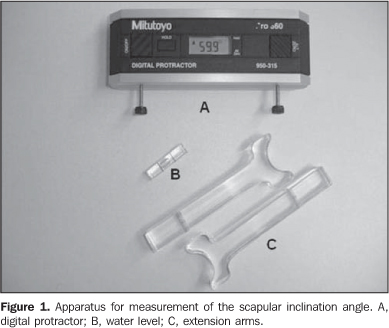
MATERIALS AND METHODS Study design and sampling Cross-sectional study approved by the Committee for Ethics in Research of Cen-tro Universitário Newton Paiva under No. 40/2005. The sample included 18 sedentary volunteers in the age range between 27 and 52 years, nine of them included in the asymptomatic group and nine in the symptomatic group. All the physicians performed abdominal ultrasonography. Time of profession ranged from 18 months to 20 years and the amount of examinations/day ranged from 10 to 30. All the eighteen patients had both shoulders evaluated (36 shoulders). Among the individuals included in the symptomatic group, five were women (55.6%) and four were men (44.4%), with mean age of 33.67 ± 8.89 years (27 to 52 years), mean body mass of 69.66 ± 13.10 kg (57.0 to 95.0 kg) and mean height of 1.73 ± 0.07 m (1.63 to 1.83 m). For the sample as whole, the mean body mass index was 22.97 ± 3.5 kg/m2 (19.14 to 31.04 kg/m2). Among the individuals included in the asymptomatic group, four were women (44.4%) and five were men (55.6%) with mean age of 38.78 ± 7.79 years (30 to 49 years), mean body mass of 76.11 ± 22.7 kg (49.0 to 115.0 kg), and mean height of 1.69 ± 0.07 m (1.54 to 1.85 m). For the sample as whole, the mean body mass index was 26.17 ± 6.5 kg/m2 (18.9 to 38.46 kg/m2). Digital protractor A Mitutoyo Digital Protractor (Mitu-toyo Evaluation Instruments; Chicago, USA) was utilized for measuring the scapular positioning. Two extension arms made of acrylic, each of them measuring 10.0 cm in length, were adapted aiming at a correct accommodation of the device on the scapula and reading of the scapular inclination degrees. Additionally, a water level was coupled perpendicularly to the device to assure the correct alignment in relation to the planes of evaluation (Figure 1). The validity and reliability of the utilization of this digital protractor as a means for measuring the scapular positioning were described by Johnson et al.(6), who have utilized the same tool and measurements.
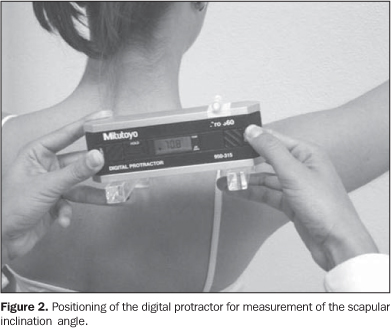
The Brazilian version of the Disability Arm Shoulder Hand questionnaire The authors utilized the Brazilian version of the Disability Arm Shoulder Hand questionnaire transculturally adapted and translated into Brazilian Portuguese by Orfale et al.(14). This questionnaire was originally developed in English and called DASH Questionnaire by Hudak et al. in 1996, with the objective of measuring the physical disability and symptoms of upper limbs in a heterogeneous population. Additionally, it was proposed for evaluating disabilities and symptoms of a single or several conditions in upper limbs. Evaluation of the functional angle of the upper limb Aiming at measuring the functional angle of the upper limb, skin markers made of acrylic were attached with double-sided tape over the following anatomical references: 7th cervical vertebra (C7), 7th thoracic vertebra (T7), acromion and lateral epicondyle. A digital photo camera Sony Mavica MVC-FD 200 (Sony Electronics, Inc.; San Diego, USA) was utilized for the functional positioning image recording. The data were observed at the rest position of the upper limb (anatomical position) at 30°, 60°, 90° and 120° of shoulder elevation in the frontal, scapular and sagittal planes. The most frequently positioning adopted while performing US scans was adopted for evaluation. Data collection All the volunteers were informed about the objectives and procedures and signed a term of free and informed consent. Subsequently, a single observer who had been duly trained for this purpose performed individual interviews, physical evaluation and applied the Brazilian version of the DASH questionnaire with all the volunteers included in the present study. The data were recorded for later analysis. With the individual in the seated position, a second observer who had also been duly trained for this purpose, positioned the digital protractor on the scapular spine. The extension arms were coupled to the medial border of the scapular spine and inferiorly to the acromion for a correct positioning and accommodation of the device to the anatomical reference (Figure 2). A third observer performed the reading and recorded the values observed in the rest position of the upper limb (anatomical position) at 30°, 60°, 90° and 120° of shoulder elevation in the frontal, scapular and sagittal planes. A support was utilized for normalizing the positioning of the upper limb during the examination in order to assure its correct positioning in these planes.
Then, skin markers were positioned on the anatomical references for photographic recording of the functional angle of the upper limb positioning during the US examination. The volunteer was asked to simulate his/her functional positioning adopted while performing an US scan. The upper limb positioning was recorded instructing the volunteer to adopt his/her most frequent positioning while performing US scans. The images were stored and the upper limbs positioning was evaluated with the aid of the software AutoCAD 2004 (Autodesk, Inc.; San Rafael, USA). Straight lines were traced to connect the points from C7 to T7 and from the acromion to the lateral epicondyle. The functional angle of the upper limb positioning for the examination was determined by the angle formed by this two straight lines (Figure 3). Statistical analysis Descriptive statistics, normality tests (Shapiro-Wilk) and variance equality tests (Levene) were applied for all of the variables utilizing the SPSS (Statistical Package for Social Sciences). The ANOVA analysis of variance was utilized for investigating statistically significant differences between groups and the sides for all the variables, scapular inclination angles and functional evaluation of the upper limbs. The Student's t-test was utilized to compare the values found by the Brazilian version of the DASH questionnaire. The Spear-man's coefficient was utilized for determining the correlation between the evaluation of upper limbs positioning and disability degree. The significance level established was α = 0.05.
RESULTS The mean profession time in the asymptomatic group corresponded to ten years, and four years and nine months. The average number of US scans/day in the asymptomatic group was of 17.8, and in the symptomatic group, 22.7. No statistically significant difference was observed in time of profession (p = 0.092) and number of US scans/day (p = 0.186), between the symptomatic and asymptomatic groups. Variables analyzed Brazilian version of the DASH questionnaire - Statistically significant difference was observed for the first 30 questions (p = 0.001) and for the optional work module (p = 0.012), in the comparison between the symptomatic and the asymptomatic groups, as shown respectively on Figures 4 and 5. The mean score for the first 30 questions of the DASH questionnaire in the symptomatic group was 16.16 ± 13.18 points (2.5 to 45.5 points) and in the four study-related questions was 27.08 ± 20.96 (0 to 56.25 points). The mean score for the first 30 questions in the asymptomatic group was 1.11 ± 1.81 points (0 to 5 points) and 4.16 ± 8.83 points (0 to 25 points) in the study-related questions.
Scapular inclination angle - There was a statistically significant difference of 6.65° (p = 0.016) and 5.87° (p = 0.033) in the scapular inclination angle in the frontal plane at 90° and 120°, respectively, in the comparison between the right shoulder in the symptomatic group and the right shoulder in the asymptomatic group. Also, a statistically significant difference of 4.43° (p = 0.028) was observed in the asymptomatic group, in the comparison of the left shoulder in relation to the right shoulder in rest position (0), frontal plane. Functional angle of the upper limb - According to Figure 6, the functional positioning of the upper limb did not present any statistically significant difference between the symptomatic and asymptomatic groups (p = 0.765), with a movement amplitude > 50° in both groups. The mean upper limb positioning angle in the symptomatic group during the US scan simulation was of 51.78 ± 15.11° (38 to 78°). The mean upper limb positioning angle in the asymptomatic group during the US scan simulation was of 53.89 ± 14.3° (34 to 76°). As regards the measurement of the scapular inclination angle (functional positioning) of upper limbs, and between the disability degree for the symptomatic group, the correlation as mildly negative (r = -0.473; p = 0.199) and for the asymptomatic group the correlation was weakly negative (r = -0.092; p = 0.814).
DISCUSSION In the present study no statistically significant difference was observed between time of profession and number of examinations performed per day, comparing the asymptomatic group with the symptomatic one. So, no direct relationship was observed between time of profession and symptoms. One can infer that this may be occurred due to a physiological adaptation of the musculature as a result of necessities of the occupational activity. In the evaluation of the Brazilian version of the DASH questionnaire, the first 30 questions presented statistically significant differences between the symptomatic and asymptomatic groups. In the present study, the results obtained with the questionnaire indicated pain and/or discomfort in the shoulder of the individuals of the symptomatic group. One can infer that these symptoms result from the sustained shoulder abduction by the sonographer during the US scan corroborated by the measurement of the upper limb positioning angle during the US scan simulation. The necessity of holding the transducer with arm abduction positioning with no support, particularly for visualizing structures in the left side half of the patient's body, and the extended time of the US scanning indicate a direct relationship with the symptoms reported by the volunteers enrolled in the present study. According to the results of the Brazilian version of the DASH questionnaire, the authors could establish a parallel with the approach of the International Classification of Functionality, Disability and Health (ICF). The authors observed that the activity and participation in the symptomatic group was impaired because of the structural and functional alteration of upper limb itself, which may have led to a certain degree of disability for both occupational and daily life activities. However, the disability should ever be seen in a bio-psychosocial context, considering that these three factors are directly related with the ICF topics(15,16). In the present study, the upper limb positioning angle during the US scan simulation did not present any statistically significant difference between the symptomatic and asymptomatic groups. The authors observed that in the majority of ultrasonography clinics evaluated, the US equipment was in compliance with a certain standardization in relation to the height of the sono-grapher's chair and the patient's bed and distance of the monitor screen. This is not an ideal standardization, considering that each sonographer has a different biotype, and this factor may have interfered in the abduction angulation among individuals. Jakes(17) and Muir et al.(18) have demonstrated that the posture adopted for the upper limb during the occupational activity represents an indicator for overload and risk for development of shoulder disorders. Jakes(17) reports that the main causes of musculoskeletal lesions in sonographers are: the necessity of sustained shoulder abduction for a better positioning of the transducer on the patient's skin; the US scanning performance associated with the manipulation of the monitor screen, and ergonomic conditions such as inappropriate height and tilt of the monitor screen, height of the sonographer's chair and height of the patient's bed during examination. All these factors associated with reduced intervals between examinations, may contribute to functional alterations and permanent disability(12,18,19). A mean abduction of 20° is considered as acceptable for continuous activities with a little overload(15). Considering that the averages observed in the present study were higher than the recommended 20°, the risk for development of muscular imbalance as well as postural alterations and dynamic overload, is high for the individuals included in the present study. As far as the measurements performed with the protractor are concerned, statistically significant differences were found between the symptomatic and asymptomatic groups in the frontal plane at 90° and 120°. The difference observed at 90° was of 6.65° in the right shoulder of the symptomatic volunteers as compared with the right shoulder of the asymptomatic ones; and at 120°, a difference of 5.87° was observed in the right shoulder of the symptomatic individuals as compared with the right shoulder of the asymptomatic ones. Also, there was a significant difference in the asymptomatic group in the frontal plane at rest position corresponding to 4.43° of the left shoulder in relation to the right shoulder. With a sustained abduction at approximately 90°, the musculature may present fatigue with consequential incapacity for sustaining this position for long periods, related to the occupational activity (ultrasonography). This factor can lead to a muscular adaptation to assure the functionality; moreover, this may trigger muscular imbalances in muscular arcs where there is a difficulty for muscular groups to sustain an appropriate stabilization or positioning of bodily segments during the development of a specific activity such as sports and occupational activities. Barbosa et al.(11) have affirmed that during the US scanning, the sonographer must sustain shoulder abduction without any support, which causes an isometric contraction of the upper limb muscles, mainly the scapular cingulum, in an attempt to provide a stabilization capable of allowing a precise movement of the wrist and hand, increasing the effectiveness in the accomplishment of the required motor task. In the present study, the difference observed in the comparison between groups of shoulders utilized during US scanning may be due to the muscular fatigue resulting from the posture adopted to sustain the upper limb abduction for performing the examination. In association with the examination time and the compensation required to sustain the system functionality, this imbalance may affect the movements' continuity in upper muscular arcs. The authors observed a scapular dyskinesia at 120° abduction, that seems to be directly associated with the difficulties reported by the volunteers participating in the present study through their answers to some items of the Brazilian version of the DASH questionnaire related to daily life activities (DLA), for example, "wash the back", "change an overhead bulb". As regards the difference observed in the asymptomatic group, at rest (0) in frontal plane, one can infer that the symptomatic individuals may have adopted an antalgic positioning during the scapular measurement, which may have interfered in the values of angles observed between the right and left shoulders. Such adaptations change both the passive and active forces which act on the shoulder during the movement. In the present study, there was no correlation between the variables analyzed. This fact may be due to an accommodation of the individual to his/her professional activity. Also, it is important to note that the objective evaluation is not always coincident with individual's perception of his/her own disability. Therefore, postural alterations may impair the musculoskeletal system ability to perform precise movements so, with the time and frequency of repetition of the task, the pain arises as a result of these imprecise movements, which may specifically impair the system functionality depending on the capacity of each individual and of the system apparatus to cope with and adapt to this new context.
CONCLUSION Based on the results of the present study, the authors could observe that there is a relationship between changes in the scapular inclination angle and the degree of upper limbs disability in sonographers during US scans. Alterations in the scapular inclination complicate the upper limbs stability, impairing their functionality during occupational and daily life activities. It is ideal that priority be given to the performance of the US scanning in the scapular plane, where the scapular muscles act in mechanical advantage, which could avoid the muscular imbalance between these muscles and the glenohumeral muscles. Also, ergonomic changes must be implemented besides emphasizing the strengthening of the stabilizing musculature of the scapula, aiming at preventing these alterations to allow the physicians a better functional performance in their daily occupational activities.
REFERENCES 1. Moraes GFS, Faria CDCM, Teixeira-Salmela LF. Scapular muscle recruitment patterns and iso-kinetic strength ratios of the shoulder rotator muscles in individuals with and without impingement syndrome. J Shoulder Elbow Surg. 2008; 17(1 Suppl):48S-53. [ ] 2. Pope DP, Croft PR, Pritchard CM, et al. Prevalence of shoulder pain in the community: the incidence of case definition. Ann Rheum Dis. 1997; 56:308-12. [ ] 3. Côté JN, Raymond D, Mathieu PA, et al. Differences in multi-joint kinematic patterns of repetitive hammering in healthy, fatigued and shoulder-injured individuals. Clin Biomech (Bristol, Avon). 2005;20:581-90. [ ] 4. Svendsen SW, Bonde JP, Mathiassen SE, et al. Work related shoulder disorders: quantitative exposure-response relations with reference to arm posture. Occup Environ Med. 2004;61:844-53. [ ] 5. Faria CDCM, Teixeira-Salmela LF, Goulart FRP, et al. Scapular muscular activity with shoulder impingement syndrome during lowering of the arms. Clin J Sports Med. 2008;18:130-6. [ ] 6. Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31:81-9. [ ] 7. Cunha GM, Marchiori E, Ribeiro EJ. Avaliação ultra-sonográfica da articulação do ombro em nadadores de nível competitivo. Radiol Bras. 2007;40:403-8. [ ] 8. Downar JM, Sauers EL. Clinical measures of shoulder mobility in the professional baseball player. J Athl Train. 2005;40:23-9. [ ] 9. Wihlidal LM, Kumar S. An injury profile of practicing diagnostic medical sonographers in Alberta. Int J Ind Ergonomics. 1997;19:205-16. [ ] 10. Schoenfeld A, Goverman J, Weiss DM, et al. Transducer user syndrome: an occupational hazard of the ultrasonographer. Eur J Ultrasound. 1999;10:41-5. [ ] 11. Barbosa LH, Coury HJCG. A atividade do médico ultra-sonografista apresenta riscos para o sistema músculo-esquelético? Radiol Bras. 2004;37:187-91. [ ] 12. David S. Importance of sonographers reporting work-related musculoskeletal injury: a qualitative view. J Diag Med Sonography. 2005;21:234-7. [ ] 13. Matias R, Pascoal AG. The unstable shoulder in arm elevation: a three-dimensional and electromyographic study in subjects with glenohumeral instability. Clin Biomech (Bristol, Avon). 2006;21(Suppl 1):S52-8. [ ] 14. Orfale AG, Araújo PMP, Ferraz MB, et al. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the disabilities of the arm, shoulder and hand questionnaire. Braz J Med Biol Res. 2005;38:293-302. [ ] 15. Dahl TH. International Classification of Functioning, Disability and Health: an introduction and discussion of its potential impact on rehabilitation services and research. J Rehab Med. 2002; 34:201-4. [ ] 16. Sampaio RF, Mancini MC, Gonçalves GGP, et al. Aplicação da Classificação Internacional de Funcionalidade, Incapacidade e de Saúde (CIF) na prática clínica do fisioterapeuta. Rev Bras Fisioter. 2005;9:129-36. [ ] 17. Jakes C. Sonographers and occupational overuse syndrome: cause, effect, and solutions. J Diag Med Sonography. 2001;17:312-20. [ ] 18. Muir M, Hrynkow P, Chase R, et al. The nature, cause, and extent of occupational musculoskeletal injuries among sonographers - recommendations for treatment and prevention. J Diag Med Sonography. 2004;20:317-25. [ ] 19. Bravo KL, Coffin CT, Murphey SL. The potential reduction in musculoskeletal injury in the nonscanning arm by using voicescan technology during sonographic examinations. J Diag Med Sonography. 2005;21:304-8. [ ] Received June 25, 2007. * Study developed at Centro Universitário Newton Paiva, Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554