Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 1 - Jan. /Feb. of 2009
Vol. 42 nº 1 - Jan. /Feb. of 2009
|
ORIGINAL ARTICLE
|
|
Non-Hodgkin's lymphoma presenting as a single liver mass |
|
|
Autho(rs): Mila Correia Góis Peixoto, Anibal Araújo Alves Peixoto Filho, Alessandra Caivano Rodrigues Ribeiro, Giuseppe D'Ippolito |
|
|
Keywords: Lymphoma, Liver, Ultrasonography, Computed tomography, Magnetic resonance imaging |
|
|
Abstract:
IMDs, Specialists at Unit of US/CT/MRI, Hospital São Luiz, São Paulo, SP, Brazil
INTRODUCTION Primary hepatic lymphomas correspond to 0.4% of extranodal lymphomas and 0.016% of cases of non-Hodgkin's lymphoma (NHL). Although primary hepatic lymphoma is extremely rare, a secondary involvement is not uncommon. If non-treated, approximately 16% of patients with NHL and 23% of those with Hodgkin's disease present hepatic involvement. The finding of hepatic involvement is more frequent in autopsies, and is reported in up to 51% of cases of NHL and in 50-80% of cases of Hodgkin's lymphoma(1-4). Most frequently, it is found in men in their fifth decade of life(3). Hepatic NHL can be successfully treated either by means of chemotherapy(5) or surgery(3). Generally, secondary hepatic lymphomatous involvement is multinodular and diffuse; on the other hand, primary hepatic lymphomas present like a single mass in more than 70% of cases(6). Up to the present, about 100 cases of hepatic lymphoma have been described, presenting as a single mass at ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI). As a single mass, hepatic lymphomas may simulate other hepatic lesions such as metastases, abscesses(7) and, exceptionally, other hepatic tumors such as hemangiomas and hepatocarcinomas(8,9) so the adoption of an appropriate treatment is delayed. Some imaging findings can be useful in the guidance of the diagnosis.
MATERIALS AND METHODS A retrospective, observational, cross-sectional study was developed by means of archives survey searching for patients with a single liver mass diagnosed and anatomo-pathologically confirmed as NHL. The survey covered the period between January and December 2006. US, CT and MRI studies were consensually reviewed by two observers for characterizing the mentioned hepatic lesions and describing the main imaging findings.
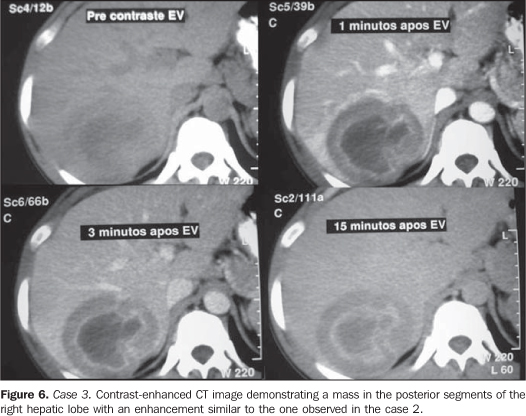
RESULTS Three cases of male patients were observed. All of them were in the fifth decade of life, presented non-specific clinical manifestations and had a single liver mass at imaging studies, histologically diagnosed as non-Hodgkin's lymphoma. Clinically, the three patients presented low fever, with abdominal pain in the right hypochondrium in two cases, and epigastric pain in one. This later patient was HIV-positive and reported weight loss for three months; and as the disease progressed, an ulcerated duodenal lesion was found and diagnosed as non-Hodgkin lymphoma. Contrarily to the other two patients, in this case the hepatic involvement was considered as secondary. The hepatic masses measured between 6 and 8 cm in diameter (mean 7 cm). In the three present cases, the lesion presented as a single liver mass with a target sign at US, CT and MRI (Figures 1 to 6), with ring enhancement after contrast agent injection at CT and MRI. In two cases, the lesion was considered as primary of the liver, and in one, as secondary to a duodenal lymphoma. No morphological difference was observed between the primary and secondary presentations. Abdominal lymphadenomegaly was not found at imaging studies in none of the cases described in the present study. Considering the small number of cases included in the present study, a detailed description of the patients and respective imaging findings will be presented. Case 1 - Male, 44-year-old, with a clinical picture of fever and mild abdominal pain for two months. At clinical examination, he presented with enlarged and mildly painful abdomen in the right hypochondrium and a palpable liver at 3 cm from the costal margin. US demonstrated a large, hyper-echogenic target-lesion, with a thick peripheral halo, and measuring approximately 7.0 cm in diameter (Figure 1). Two days later, CT demonstrated a hypo-dense, ill-defined lesion in the non con-trast-enhanced phase, and with peripheral enhancement after contrast agent injection (Figure 2). MRI demonstrated a large hypointense mass on T1-weighted images, and hyperin-tense on T2-weighted images, besides a target enhancement similar to the one found at CT (Figure 3). The anatomo-pathological study of a fragment of the lesion obtained by means of US-guided biopsy confirmed the presence of a NHL. No other lesion was found, so the hypothesis of a primary hepatic lymphoma was confirmed. Case 2 - Male, 45-year-old, HIV-positive patient presenting low fever associated with pain in the right hypochondrium, epi-gastralgia and weight loss for three months. Abdominal US demonstrated a large target-shaped mass measuring approximately 8.0 cm in diameter (Figure 4). At CT, a hypo-dense mass with peripheral contrast-enhancement in the arterial and portal phases, and progressive enhancement in the equilibrium phase (Figure 5). The patient was submitted to upper digestive endoscopy that showed a duodenal ulcerated lesion. Biopsy of the duodenal and hepatic lesions was performed, and NHL was diagnosed in both of them. This case was considered as a secondary hepatic involvement. Case 3 - Male, 40-year-old patient presenting with low fever and pain in the right hypochondrium for about three months. CT demonstrated a hypodense, ill-defined lesion in the precontrast phase, besides peripheral contrast-enhancement (Figure 6). This lesion was initially considered as an abscess and an unsuccessful drainage attempt was made. CT-guided biopsy demonstrated the presence of a NHL and, in the absence of other lymph node or parenchymal lesions, the primary hepatic involvement was determined. The lesion regressed after chemotherapy.
DISCUSSION The gastrointestinal tract is the most usual location of primary extranodal lymphomas, with stomach and small bowel being most frequently affected(10). Primary hepatic lymphomas are extremely rare with less than 100 cases described in the literature (77 cases up to 1999). However, the incidence of this disease has increased as a result of the increasing number of immune-suppressed and organ-transplanted patients(3). Generally, the non-Hodgkin's type is most frequently found, and in 70% of cases the lesion presents as a single mass(6,10,11). Secondary hepatic involvement by a lymphoma is reported in up to 50% of cases, with multinodular and diffuse presentation(1,6,11). Main clinical symptoms in patients with hepatic lymphoma are abdominal right upper quadrant (epigastrium) pain, weight loss and fever(4). Imaging methods capacity and effectiveness in the staging of lymphomas and consequent usefulness in the therapy planning and follow-up are well established(4). However, because of their uncommon presentation, lymphomas isolatedly affecting the liver can become a diagnostic dilemma(6,7). Homogeneous hepatomegaly and multinodular infiltration represent the most frequent imaging findings in cases of hepatic lymphomas(1,6,11). Presentation as a single mass is rare, and some epidemiological and imaging characteristics can be useful in the guidance of the diagnosis. Similarly to reports in the literature, the three patients included in the present study were in their fifth decade of life(3). Only one of the three patients was immune-suppressed, and none presented with signs of chronic hepatopathy. Association of primary hepatic lymphoma with cirrhosis and chronic hepatitis has been described in 30% of cases(12-15). Although the reason for this association still remains unclear, the diagnosis of NHL should be considered in cirrhotic patients with voluminous hepatic mass and normal alphafetoprotein levels. In cirrhotic patients presenting a hepatic mass, the most probable diagnosis is hepatocar-cinoma. Contrary to hepatocarcinoma that frequently presents as a hypervascularized mass(8), the present cases demonstrated predominantly hypovascular lesions which, although less frequently and usually in association with perilesional fibrotic capsules, may occur in cases of hepatocarcinoma(8). In the present cases, US detected a large, heterogeneous, solitary, target-shaped mass with central hypoechogenicity surrounded by a peripheral, thick hypoecho-genic halo, which has already been described as a quite common pattern found in patients with hepatic lymphoma(1,16). The lesions were voluminous, with diameters ranging between 5.0 cm and 8.0 cm. In the literature, lesions with up to 15.0 cm in diameter are described(17). In the three cases, CT images presented quite similar findings of a hypodense mass with ring shaped contrast-enhancement in association with a clinical picture of fever and pain in the right hypochondrium, suggesting the diagnosis of hepatic abscess that has erroneously led the authors to an attempt of drainage. These lesions presented a subtle, progressive contrast-enhancement on more delayed phases, which has been already described in primary hepatic lymphoma(17), but that is also identified in other types of lesions(18). MRI images of one of the patients with primary hepatic lymphoma, demonstrated a hypointense lesion on T1-weighted sequences, heterogeneous hypersignal on T2-weighted sequences, and peripheral enhancement after paramagnetic contrast agent injection, similarly to the findings reported by other authors in the literature(2,6,17,19,20) and considered as non-specific by some authors(6,19). Among differential diagnoses, hepato-carcinoma, intrahepatic cholangiocarci-noma, metastasis from adenocarcinoma and amebic abscess should be considered. Despite its usefulness, the correlation between clinical data and imaging findings does not rule out the necessity of histological evidence, in most of cases(3,21). The diagnosis of hepatocarcinoma can be suspected in the presence of a hypervas-cularized mass and increase in alphafeto-protein levels(8,22). Intrahepatic and peripheral cholangiocarcinoma constitute an exclusion diagnosis and generally is similar to the present cases. Even biliary tract dilatation is observed in 30% of cases(23). The appearance of amebic abscesses and hypo-vascularized metastases from hepatocarci-nomas may be closely similar to the one described in the present article, and only the correlation between clinical and laboratory data besides percutaneous biopsy can aid in the diagnostic differentiation(24). Finally, the hypothesis of hepatic lymphoma should be considered in the differential diagnosis for immune-suppressed patients with a single ring-shaped hepatic mass. In the case of male, middle-aged, cirrhotic patients, this diagnosis is extremely relevant, considering its frequency and approach that is different from the one adopted for hepatocarcinomas.
REFERENCES 1. Soyer P, Van Beers B, Teillet-Thiébaud F, et al. Hodgkin's and non-Hodgkin's hepatic lymphoma: sonographic findings. Abdom Imaging. 1993;18:339-43. [ ] 2. Soyer P, Van Beers B, Grandin C, et al. Primary lymphoma of the liver: MR findings. Eur J Radiol. 1993;16:209-12. [ ] 3. Avlonitis VS, Linos D. Primary hepatic lymphoma: a review. Eur J Surg. 1999;165:725-9. [ ] 4. Caldas FAA, Motomiya CT, Silva HC. Análise de achados de imagem e alterações clínicas em pacientes com linfoma. Radiol Bras. 2002;35:71-5. [ ] 5. Murthy SA, Singh B, Bhalla S, et al. Cure in a case of primary hepatic lymphoma. Indian J Cancer. 2000;37:165-72. [ ] 6. Gazelle GS, Lee MJ, Hahn PF, et al. US, CT, and MRI of primary and secondary liver lymphoma. J Comput Assist Tomogr. 1994;18:412-5. [ ] 7. Wu MS, Lin JT, Yang PM, et al. Hepatic lymphoma mimicking liver abscess: report of a case and review of the literature. J Formos Med Assoc. 1993;92:263-6. [ ] 8. D'Ippolito G, Abreu Jr L, Borri ML, et al. Apresentações incomuns do hepatocarcinoma: ensaio iconográfico. Radiol Bras. 2006;39:137-43. [ ] 9. D'Ippolito G, Appezzato LF, Ribeiro ACR, et al. Apresentações incomuns do hemangioma hepático: ensaio iconográfico. Radiol Bras. 2006;39: 219-25. [ ] 10. Smith C, Kubicka RA, Thomas CR Jr. Non-Hodgkin lymphoma of the gastrointestinal tract. Radiographics. 1992;12:887-99. [ ] 11. Fishman EK, Kuhlman JE, Jones RJ. CT of lymphoma: spectrum of disease. Radiographics. 1991;11:647-69. [ ] 12. Kitabayashi K, Hasegawa T, Ueno K, et al. Primary hepatic non-Hodgkin's lymphoma in a patient with chronic hepatitis C: report of a case. Surg Today. 2004;34:366-9. [ ] 13. Möhler M, Gutzler F, Kallinowski B, et al. Primary hepatic high-grade non-Hodgkin's lymphoma and chronic hepatitis C infection. Dig Dis Sci. 1997;42:2241-5. [ ] 14. Higuchi T, Nomoto K, Mori H, et al. Case report: primary hepatic lymphoma associated with chronic liver disease. J Gastroenterol Hepatol. 1997;12:237-42. [ ] 15. Clarke G, MacMathuna P, Fenlon H, et al. Primary hepatic lymphoma in a man with chronic hepatitis C. Eur J Gastroenterol Hepatol. 1997;9:87-90. [ ] 16. Ginaldi S, Bernardino ME, Jing BS, et al. Ultra-sonographic patterns of hepatic lymphoma. Radiology. 1980;136:427-31. [ ] 17. Kelekis NL, Semelka RC, Siegelman ES, et al. Focal hepatic lymphoma: magnetic resonance demonstration using current techniques including gadolinium enhancement. Magn Reson Imaging. 1997;15:625-36. [ ] 18. Freeny PC. Computed tomography in the diagnosis and staging of cholangiocarcinoma and pancreatic carcinoma. Ann Oncol. 1999;10 Suppl 4: 12-7. [ ] 19. Maher MM, McDermott SR, Fenlon HM, et al. Imaging of primary non-Hodgkin's lymphoma of the liver. Clin Radiol. 2001;56:295-301. [ ] 20. Weinreb JC, Brateman L, Maravilla KR. Magnetic resonance imaging of hepatic lymphoma. AJR Am J Roentgenol. 1984;143:1211-4. [ ] 21. Rappaport KM, DiGiuseppe JA, Busseniers AE. Primary hepatic lymphoma: report of two cases diagnosed by fine-needle aspiration. Diagn Cytopathol. 1995;13:142-5. [ ] 22. D'Ippolito G, Faria SC, Szejnfeld J. Carcinoma hepatocelular: aspectos tomográficos. Radiol Bras. 2000;33:295-9. [ ] 23. Guimarães MC, Calencautcy CR, Mello GGN, et al. Colangiocarcinoma intra-hepático periférico - relato de um caso. Rev Imagem. 1997;19:19-21. [ ] 24. Mello GGN, Meirelles GSP, Oliveira JMA, et al. Estudo comparativo dos procedimentos percutâneos orientados por métodos de imagem no tratamento das coleções hepáticas. Radiol Bras. 2001;34:83-8. [ ] Received September 29, 2008. * Study developed at Scopo Diagnóstico, Unit of US/CT/MRI, Hospital São Luiz, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554