Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 3 - May / June of 2010
Vol. 43 nº 3 - May / June of 2010
|
CASE REPORT
|
|
Importance of gallium-67 scintigraphy in primary cutaneous B-cell lymphoma: report of two cases |
|
|
Autho(rs): Cyomara Sanches Attab, Sônia Marta Moriguchi, Eduardo José Alencar Paton, Mário Henrique Leite de Alencar, Euclides Timóteo da Rocha |
|
|
Keywords: Lymphoma, Scintigraphy, Gallium |
|
|
Abstract:
IMD, Nuclear Physician, Assistant at Centro Brasileiro de Medicina Nuclear - Cebramen, Goiânia, GO, Brazil
INTRODUCTION Lymphomas may affect the skin either as a primary or secondary disease. Cutaneous T-cell lymphoma is the most common type of lymphoproliferative disorder, with mycosis fungoides and Sézary syndrome being main representative examples of this disease. Cutaneous B-cell lymphoma, a rare nosological entity, is observed in less than 10% of cases o non-Hodgkin lymphomas(1). The diagnosis and management of this disease is based on the results of clinical and histological tests, besides conventional imaging findings. In dubious cases, invasive procedures can elucidate the diagnosis. The utilization of gallium-67 scintigraphy in cases of cutaneous B-cell lymphoma has been poorly described in the literature(1), particularly after the adoption of 18F-fluorodeoxyglucose positron emission tomography in the clinical practice of great European centers that demonstrated the high sensitivity and specificity of the method(2). Gallium-67 scintigraphy still remains as a relevant, complementary resource in the pre- and post-treatment clinical management, allowing a functional and metabolic tissues characterization, as a complement to anatomical data. Additionally to the diagnosis and staging, information provided by gallium-67 scintigraphy is useful in the follow-up and evaluation of the therapeutic response of patients with lymphoma. An evaluation of anatomical characteristics alone is insufficient in the presence of a residual mass following chemotherapy, or small-sized lymph nodes infiltration. Such evaluation can be completed with the utilization of gallium-67 scintigraphy, considering that PET-FDG is not easily accessible yet in Brazilian centers.
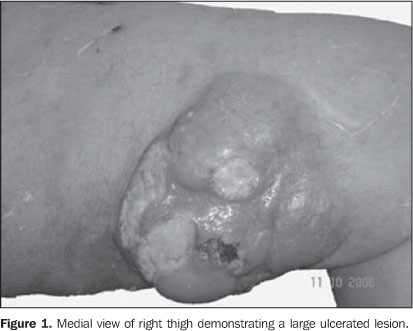
CASES REPORT Case 1 A male, white, 65-year-old patient referred to the Division of Hematology, presenting a lesion on the left thigh with progressive growth for one year and unresponsive to home treatment. Later, the patient had observed the emergence of nodules in the inguinal region. No fever or weight loss was observed. Clinical examination demonstrated the presence of an ulcerovegetating tumor with 15 cm in diameter on the medial aspect of the left thigh, besides bilateral painless inguinal lumps, the ipsilateral one with 6 cm, and the other, at right, with 3 cm, with no sign of inflammation and mobile to palpation (Figure 1). Tests and imaging studies were performed for diagnosis and staging, as follows: chest, abdomen and pelvis computed tomography, myelogram, protein electrophoresis blood test, open biopsy of the lesion and gallium-67 scintigraphy.
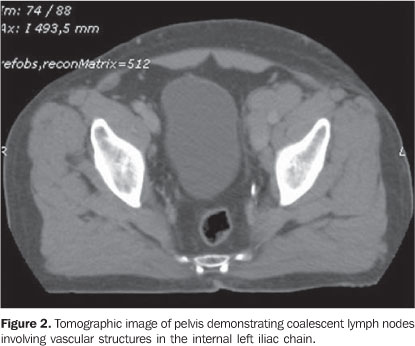
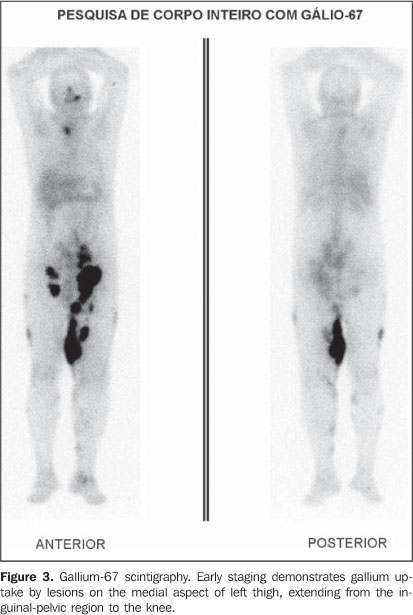
Anatomopathological and immunohistochemical results were compatible with diffuse large B-cell non-Hodgkin's lymphoma. Tomographic images demonstrated only a group of coalescent, ovoid nodules in the left internal iliac chain, the largest one measuring 2.8 × 2.5 cm, and a lobular, homogeneous mass in the inguinal regions, the largest one at left (7.4 × 4.3 cm) (Figure 2). Gallium-67 citrate scintigraphy was performed, with images being acquired 48 hours after radiotracer injection at a dose of 296 MBq (8 mCi), and demonstrated an unusual radiotracer uptake, from the inguinal-pelvic to the medial aspect of the left knee, besides multiple hyper-uptake areas in the left maxilla, manubrium, left inguinal-pelvic region, right gluteus, at left in the intergluteal area, thighs, legs and left ankle (Figure 3).
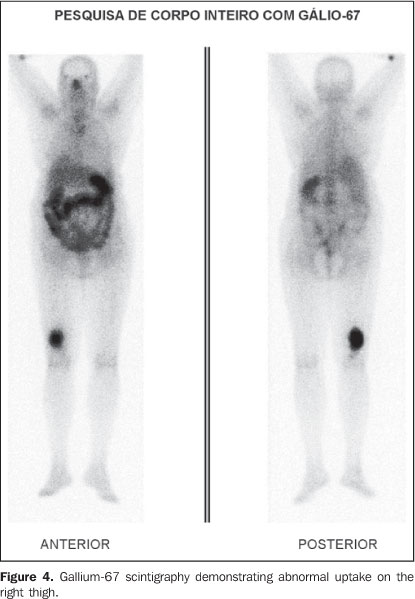
A total coincidence was observed between the lesions detected at physical examination and the scintigraphic findings. Bone marrow biopsy as well as protein electrophoresis results were normal. The proposed chemotherapy scheme included cyclophosphamide, hydroxydoxorubicin (doxorubicin), vincristine (Oncovin) and prednisone (CHOP), the whole regimen comprising eight cycles. After chemotherapy completion, a new staging was made by means of the same tests and imaging studies previously performed. Noninvasive imaging methods demonstrated the presence of amorphous tissue with soft tissue density in the left inguinal region (4.5 × 1.5 cm) and at right (1.8 × 1.2 cm), besides the absence of pelvic adenopathy. Follow-up gallium-67 scintigraphy results were normal, demonstrating the disappearance of the lesions. Complete regression of the thigh lesion was observed, with substitution by cicatricial tissue confirmed at gallium-67 scintigraphy. Case 2 A female, white, 71-year-old patient was referred with a history of a left thigh lesion with progressive growth for three months. The patient denied fever and night sweats. Her previous pathological history did not include any surgery; the patient only had hypertension and diabetes, with a familial history negative for neoplasia. At clinical examination, the patient presented a good general condition, with body mass índex of 26 and performance status of 1. There was a hard patchy lesion measuring 10 × 9 cm, on the posterior aspect of her thigh, with infiltration into deep planes, and with no satellite adenopathy. Incisional skin biopsy result was consistent with cutaneous B-cell lymphoma. Conventional imaging methods (chest and abdomen computed tomography) did not demonstrate the presence of disease in other sites. Gallium-67 scintigraphy with high-energy collimator, with images acquisition 48 hours after 67-gallium citrate injection at a dose of 296 MBq (8 mCi), demonstrated an abnormal radiotracer uptake on the distal third of the right leg (Figure 4). Bone marrow biopsy and protein electrophoresis results were normal.
The patient received six cycles of CHOP chemotherapeutic regimen, additionally to locoregional radiotherapy (total dose = 3600 cGy (20 × 180 cGy)). The patient progressed with improvement and complete lesion regression after the treatment. Post-therapy follow-up gallium-67 scintigraphy did not demonstrate any abnormality.
DISCUSSION Cutaneous involvement by a lymphoma may be primary or secondary to a metastatic disease. Primary cutaneous lymphoma corresponds to the second most frequent group of extranodal involvement of non-Hodgkin lymphomas, preceded only by the gastrointestinal tract (about 10%)(3). It is classified according to the involved cell type, i.e., T-cell (CTCL) with 65% of cases, and B-cell (CBCL) with 20-25% of cases. Cutaneous T-cell lymphomas predominantly affect men with ages ranging from 40 and 60 years. Both tumor types present a histological architecture similar to the systemic lymphoma, but with a completely different prognosis and behavior. Usually, such tumors originate from mature cutaneous T-helper cells, with mycosis fungoides and Sézary syndrome being the most frequent ones in this group. In this case, the disease tends to spare the bone marrow, is hematogenically disseminated, and presents a high rate of recurrence. On the other hand, cutaneous B-cell lymphomas originate from centrofollicular cells and are characterized by their locoregional extent. These tumors are rarely found (8%) and, in truth, they represent a secondary cutaneous involvement by a systemic lymphoma in most of cases(3). The lesions are characterized by nodules with a glossy surface, and rare desquamation or ulceration. The surrounding skin may be hyperemic, with small papular lesions or plaque infiltrates, with dimensions ranging from small sizes to 15 cm(1). Generally, these tumors present an indolent pattern, and may remain stable for months or years before presenting an abrupt development and growth. Extracutaneous dissemination is not frequently observed, but is described in up 13% of cases, usually limited to the site of lymph node drainage(1). The correct determination of the disease extent and classification plays a relevant role in the definition of cutaneous lymphomas management and prognosis; therefore, several diagnostic modalities should be utilized in the attempt to rule out extracutaneous lesions. According to the Ann Arbor system, the staging itself justifies the utilization of imaging methods, considering that this system is based on the analysis of the disease extent. Computed tomography, as compared with magnetic resonance imaging, allows an early and comprehensive staging, because of the rapid images acquisition(4). However, in spite of computed tomography being the method of choice in these cases, the presence of a post-chemotherapy residual mass or small-sized lymph nodes infiltration constitute examples of situations where an evaluation of anatomical characteristics alone is insufficient, besides failing in the provision of accurate information about malignant cutaneous lesions(5,6). The mechanism by which gallium-67 scintigraphy demonstrates the lesion is based on the gallium ion transport into the cell through the plasmatic membrane, after gallium-transferrin complex binds to transferrin receptors on the tumor cell surface(7). Factors such as vascularization, vascular patency and increased ion-exchange due to increased membrane porosity, contribute for the final gallium uptake by the malignant cell. Gallium-67 scintigraphy demonstrated multiple uptake areas with a good correlation in all lesions of both patients, being useful in the diagnosis, staging and therapy planning(6), considering that, in association with conventional imaging methods, gallium-67 scintigraphy constitutes a relevant complementary method for detecting occult lesions and guiding changes in the management of patients with post-chemotherapy residual tumor activity. Therefore, the present cases demonstrate the relevant role of gallium-67 scintigraphy in the detection of the disease extent and in the evaluation of the patient's response to therapy, by demonstrating, or not, the tumor activity(8). In the authors' institution gallium-67 scintigraphy is also utilized in the follow-up of these patients for monitoring residual disease. Many of gallium-67 scintigraphy and computed tomography limitations can be resolved with the utilization of PET-FDG that has demonstrated high accuracy, sensitivity and specificity in the detection of both nodal and extranodal involvement in patients with lymphoma. However, only a restricted number of studies with few patients and variable results have reported the utilization of PET-FDG in the diagnosis of cutaneous lymphoma, as well as the difficult access of patients to the procedure. In summary, PET-FDG has demonstrated a potential value in the early staging as well in the post-therapy restaging in these patients. Although a consensus on this theme is still to be achieved by specialists, and the low number of cases reported is still a limiting factor, gallium-67 scintigraphy remains among the diagnostic methods in the protocol for both the initial staging and post-therapy restaging for cutaneous B-cell lymphomas, to differentiate between the presence of residual disease and possible sequelae, thus allowing an early intervention in accordance with the therapy response.
REFERENCES 1. Assassa GS, Siegel ME, Chen DC, et al. Ga-67 uptake in cutaneous B-cell lymphoma. Clin Nucl Med. 1994;19:614-6. [ ] 2. Sapienza MT, Marone MMS, Chiattone CS. Contribuição da medicina nuclear para a avaliação dos linfomas. Rev Bras Hematol Hemoter. 2001; 23:79-92. [ ] 3. Kumar R, Xiu Y, Zhuang HM, et al. 18F-fluoro-deoxyglucose-positron emission tomography in evaluation of primary cutaneous lymphoma. Br J Dermatol. 2006;155:357-63. [ ] 4. Borba AMV, Monteiro AMV, Lima CMAO, et al. Aspectos da tomografia computadorizada no linfoma em pacientes abaixo de 20 anos de idade. Radiol Bras. 2007;40:87-92. [ ] 5. Delcambre C, Reman O, Henry-Amar M, et al. Clinical relevance of gallium-67 scintigraphy in lymphoma before and after therapy. Eur J Nucl Med. 2000;27:176-84. [ ] 6. Israel O, Front D, Lam M, et al. Gallium 67 imaging in monitoring lymphoma response to treatment. Cancer. 1988;61:2439-43. [ ] 7. van Amsterdam JA, Kluin-Nelemans JC, van Eck-Smit BL, et al. Role of 67Ga scintigraphy in localization of lymphoma. Ann Hematol. 1996;72: 202-7. [ ] 8. Hod N, Pinkas L, Horne T. Multiple focal uptake of (67)Ga in cutaneous tissue. Semin Nucl Med. 2002;32:220-2. [ ] Received October 23, 2008. * Study developed at Hospital de Câncer de Barretos - Fundação Pio XII, Barretos, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554