Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 3 - May / June of 2010
Vol. 43 nº 3 - May / June of 2010
|
ORIGINAL ARTICLE
|
|
Type 1 neurofibromatosis: radiological findings of the chest |
|
|
Autho(rs): Marcos Pontes Muniz, Antonio Soares Souza, Divanei Aparecida Bottaro Criado, José Roberto Lopes Ferraz Filho, Rafael Marinelli Brandão, Luciana Vargas Cardoso, Eny Maria Goloni Bertollo |
|
|
Keywords: Type 1 neurofibromatosis, Radiology, Chest radiography, Bone abnormalities, Mediastinal neoplasms |
|
|
Abstract:
IPhD, Professor in Diagnostic Imaging Department, Head of Radiology Service - Hospital de Base in São José do Rio Preto, SP, Brazil
INTRODUCTION Neurofibromatosis (NF) is an autosomal dominant disease that was first described by Friedrich von Recklinghausen in 1882. Several types of NF have been described, and type 1 (NF1), also denominated peripheral or classic NF, is the most common, occuring in 1:3,000 individuals(1). One of the main characteristics of this disease is systemic and progressive involvement, with impaired neurological functions(2) and physical deformity(3). The diagnostic criteria for NF1 were defined by the National Institutes of Health (NIH)(4) in 1987 and updated three years later(5). Main clinical presentations of NF1 include café-au-lait spots, cutaneous neurofibromas, ephelides or freckling in axillary and/or inguinal regions, plexiform neurofibromas and Lisch nodules(1,6,7). Bone abnormalities observed in NF1 have been receiving increasing attention and must be recognized by the radiologist as some are typical of the disease and others are strongly suggestive of NF1(8,9). In NF patients, the most frequent skeletal abnormalities are observed in the spine and may directly affect the skeletal system due to mesodermal dysplasia (dural ectasia and bone dysplasia), or indirectly by secondary complications such as tumor compression, in particular of neurofibromas and meningoceles(10). The commonest alterations include scoliosis, kyphoscoliosis, erosion of the posterior wall of vertebral bodies, erosion of the anterior wall of vertebral bodies, widening of intervertebral foramina, growth disorders, pseudoarthrosis, thinning of long bone cortices, bone cystic lesions, costal arch erosion, thinning of pedicles, sphenoid wing dysplasia, cranial osteolytic lesions, facial/mandibular deformities, subperiosteal bone proliferation, bone compression due to soft-tissue tumors (neurofibromas, dura mater dysplasias, intrathoracic meningocele)(11). Erosion of the lower borders and irregularities of costal arches, rib cage deformities (pectus excavatum and kyphoscoliosis) and mediastinal masses (meningocele and neurofibroma)(10) may be detected on the chest radiographs of NF1 patients. Costal arch erosion is sometimes caused by extrinsic compression by neurofibromas which produces cortical erosion of the lower borders of the ribs, or as a consequence of a primary dysplastic defects in bone formation(12). Thoracic deformities, such as pectus excavatum, observed at physical examination in 31% to 50% of NF1 patients, represents a depression of the lower portion of the sternum, causing excavation of the anterior thoracic region(11). Another thoracic deformity, caused by kyphoscoliosis, may result in evaluation distortions(11). Thoracic meningocele is an abnormality of the vertebral spine corresponding to herniation of the meninges through the intervertebral foramen with a benign course which remains asymptomatic in most cases(13). Approximately 70% to 80% of all cases of thoracic meningocele occur in NF patients(13). Thoracic neurofibromas are benign tumors involving the nerve roots of the spinal cord unilaterally or bilaterally and may affect several segments of the spine. The presence of such posterior mediastinal masses in both postero-anterior and lateral plain chest radiographs is not enough for diagnostic differentiation, thus further investigations using computed tomography (CT) or magnetic resonance imaging (MRI) are required(14). Several studies have described different imaging methods for the diagnosis of NF1(15-18). The observation of thoracic findings and the respective sensitivity of the technique used are valid in the application of such concepts, particularly with regards to early diagnosis of the disease. The justification of the current study took into account that chest radiography is a low-cost, easy-to-perform method. Thus, this study aimed at identifying alterations suggestive of NF1 on postero-anterior and lateral views of plain chest radiographs, establishing their frequency and evaluating the possibility of including the presence of a posterior mediastinal mass as a criterion for the diagnosis of NF1. With these elements, the present study may serve as a warning to health professionals on the importance of this finding with consequent referral of their patients for more specific investigations.
MATERIALS AND METHODS This study included 141 NF1 patients assisted in the Centro de Pesquisa e Atendimento em Neurofibromatose - Cepan (Research and Assistance Center for Neurofibromatosis), a multidisciplinary center of Hospital de Base and the College of Medicine in São José do Rio Preto (Famerp), Brazil, who were evaluated and later referred to the Diagnostic Imaging Department of the same institution. The patients underwent both postero-anterior and lateral chest radiography, performed with the standard technique, i.e., with the bucky focused at 1.80 m in a Philips equipment, with 35 × 35 (postero-anterior view) and 30 × 40 (lateral view) green X-ray films, developed in an automatic Kodak-90® processing unit. The ages of the patients ranged from 2 to 72 years (mean age, 33.1 years; standard deviation, 18.2 years). The study was double-blinded and was approved by the Committee for Ethics in Research of Famerp. The variables analyzed were the presence or absence of typical thoracic bone alterations found in patients diagnosed with NF1. The obtained data were qualitatively and quantitatively evaluated by means of non-parametric statistical methods, with the significance level being set at 0.05.
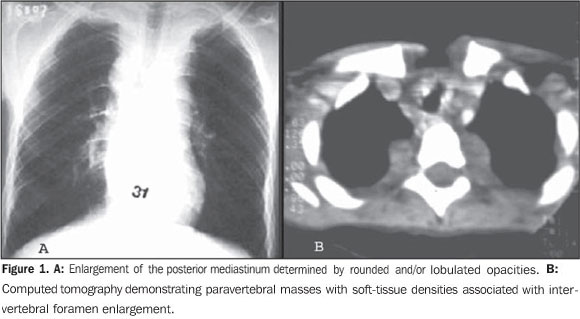
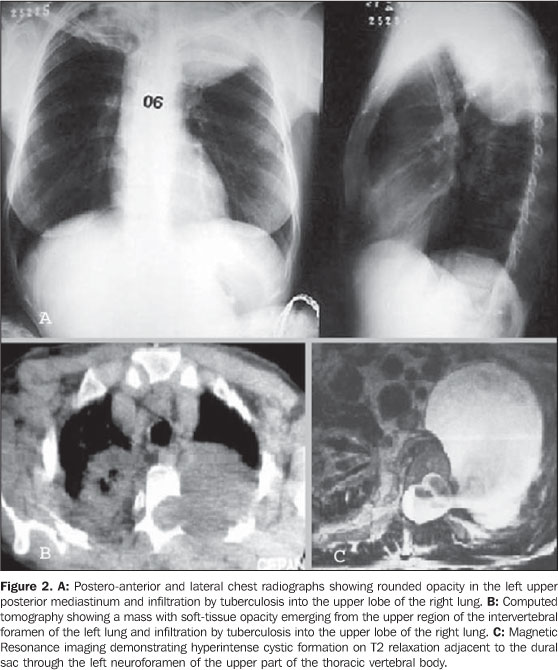
RESULTS Among the patients studied, 39% (n = 55) presented alterations at radiography, with 21 of these patients (14.9%) presenting with more than one alteration. Pectus excavatum was observed in 17 patients (12%), costal arch alterations (irregularities and deformities) in 28 patients (19.8%) and kyphoscoliosis in five patients (3.5%). Kyphoscoliosis determines deformity of the rib cage, with reduction in the volume of the lungs and false enlargement of the cardiac area. Posterior mediastinal enlargement determined by rounded and/or lobulated opacities with soft tissue densities next to the spine, was found in ten of the patients (7.1%) who were later submitted to CT (Figure 1), demonstrating the presence of a solid homogeneous masses in nine patients and a cystic mass in one patient. The patient with the cystic mass was submitted to MRI, which demonstrated it to be a meningocele (Figure 2).
DISCUSSION Due to the large variation in clinical expressiveness and genetic heterogeneity of NF1 patients, the diagnosis of this disease is very difficult, particularly during childhood(19,20). The clinical signs are not always typical. Thus radiology may contribute to demonstrate typical findings of the disease such as sphenoid wing dysplasia, pseudoarthrosis and thinning of the long bones cortex(11). Chest radiography is a complementary study that, in association with the clinical history and physical examination, is the main tool for evaluating thoracic alterations and is highly sensitive. In patients with a posterior mediastinal mass associated with other clinical signs, such as café-au-lait spots, a plain chest radiography may help in the diagnosis of NF1. Whenever a posterior mediastinal mass is present at chest radiography, the patient must be referred for an investigation using more complex imaging methods (CT and MRI), which, besides confirming the diagnosis, may provide data on possible complications. Among the alterations found in the analysis of chest radiographs, costal arch irregularities were the most common ones (19.1%). This abnormality may occur due to a primary dysplastic defect in bone formation or by erosion of an intercostal neurofibroma(8,10,14). A "twisted-ribbon" appearance of the ribs is frequently reported(8-11). Data on the incidence of costal arch lesions were not found in the literature review. Pectus excavatum was observed on the lateral radiographic views of 17 patients (12.0%), while at physical examination this finding was observed in 31 patients. This alteration may cause clinical symptoms such as paradoxical breathing or angina-like pain(11,21,22). Posterior mediastinal masses found in ten of the 141 patients (7.1%) were rounded or lobulated masses with soft-tissue density that emerged from the vertebral canal. Following the division of the mediastinum in compartments(23) on plain chest radiographs of the 141 NF1 patients, masses were only identified in the posterior mediastinal compartment, i.e., no masses were found in the middle and anterior mediastina. Posterior mediastinal masses are associated with NF1 and may be caused by neurofibromas that originate in spinal cord nerve roots or by intrathoracic meningoceles(10,11,24). Plain chest radiography is not enough for a clear differentiation between neurofibromas and meningoceles, thus there is a need for an investigation using more advanced methods, such as CT or MRI. Among the 10 patients with posterior mediastinal masses confirmed by CT, 9 presented with solid masses suggesting neurofibroma as they were related to the neuroforamen, and one patient presented with a cystic mass which was subsequently identified as a left-sided intrathoracic meningocele by MRI; this patient presented with residual lesions of tuberculosis on the right pulmonary apex. About 80% of patients presenting with intrathoracic meningoceles have NF1(25,26). Two or more skin neurofibromas or one plexiform neurofibroma are diagnostic criteria of NF1 as defined by the NIH(4). Thus, the presence of neurofibromas in the paravertebral regions should be considered as of equal value in the diagnosis of NF1. No information on the incidence of posterior mediastinal masses in the general population was found in the literature. Among the criteria for typical bone lesions as defined by the NIH, sphenoid wing dysplasia was found in 1% of the cases. This finding, observed by radiography or CT, is highly specific, but is not common. The frequency of pseudoarthrosis is 1:250,000 births with approximately 50% to 90% of the cases being associated with NF1. This is considered as a relatively rare finding, with an incidence of about 3%. Thinning of the long bones cortex, observed in 8.5% of patients, is not a very specific finding and requires radiography of the entire appendicular skeleton, i.e., upper and lower limbs(4,11). The identification of posterior mediastinal masses by either skeletal radiography or chest radiography may make these findings of typical bone lesions more valuable. Thus, the inclusion of posterior mediastinal masses as an additional criterion in the diagnosis of NF1 is suggested. At plain chest radiography, it is possible to identify bone alterations in NF1 patients, and the presence of posterior mediastinal masses, in addition to the characteristic bone alterations defined by the NIH(4) indicate that this is a consistent finding to be proposed as a criterion for the diagnosis of NF1.
CONCLUSION Posterior mediastinal masses associated with the characteristic bone lesions as defined by the NIH, is a consistent finding and should be considered as a criterion for the diagnosis of type 1 neurofibromatosis.
REFERENCES 1. Ruggieri M. The different forms of neurofibromatosis. Childs Nerv Syst. 1999;15:295-308. [ ] 2. Mariaud-Schmidt RP, Rosales-Quintana S, Bitar E, et al. Hamartoma involving the pseudoarthrosis site in patients with neurofibromatosis type 1. Pediatr Dev Pathol. 2005;8:190-6. [ ] 3. Trovó-Marqui AB, Goloni-Bertollo EM, Valério NI, et al. High frequencies of plexiform neurofibromas, mental retardation, learning difficulties, and scoliosis in Brazilian patients with neurofibromatosis type 1. Braz J Med Biol Res. 2005;38: 1441-7. [ ] 4. [No authors listed]. Neurofibromatosis. Conference Statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45:575-8. [ ] [ ] 6. Ruggieri M, Huson SM. The neurofibromatoses. An overview. Ital J Neurol Sci. 1999;20:89-108. [ ] 7. Muniz MP, Ferraz Filho JRL, Souza AS, et al. Neurofibromatose tipo 1: aspectos clínicos e radiológicos. Rev Imagem. 2006;28:87-96. [ ] 8. Li Y, O'Connell P, Breidenbach HH, et al. Genomic organization of the neurofibromatosis 1 gene (NF1). Genomics. 1995;25:9-18. [ ] 9. Littler M, Morton NE. Segregation analysis of peripheral neurofibromatosis (NF1). J Med Genet. 1990;27:307-10. [ ] 10. Alwan S, Tredwell SJ, Friedman JM. Is osseous dysplasia a primary feature of neurofibromatosis 1 (NF1)? Clin Genet. 2005;67:378-90. [ ] 11. Muniz MP, Almeida JRM, Araújo Neto SA, et al. Prevalência de achados radiográficos da neurofibromatose tipo 1: estudo de 82 casos. Radiol Bras. 2002;35:65-70. [ ] 12. Fortman BJ, Kuszyk BS, Urban BA, et al. Neurofibromatosis type 1: a diagnostic mimicker at CT. Radiographics. 2001;21:601-12. [ ] 13. Andrade GC, Braga OP, Hisatugo MK, et al. Giant intrathoracic meningoceles associated with cutaneous neurofibromatosis type I: case report. Arq Neuropsiquiatr. 2003;61:677-81. [ ] 14. Rossi SE, Erasmus JJ, McAdams HP, et al. Thoracic manifestations of neurofibromatosis-I. AJR Am J Roentgenol. 1999;173:1631-8. [ ] 15. Hassell DS, Bancroft LW, Kransdorf MJ, et al. Imaging appearance of diffuse neurofibroma. AJR Am J Roentgenol. 2008;190:582-8. [ ] 16. Lim R, Jaramillo D, Poussaint TY, et al. Superficial neurofibroma: a lesion with unique MRI characteristics in patients with neurofibromatosis type 1. AJR Am J Roentgenol. 2005;184:962-8. [ ] 17. Shu HH, Mirowitz SA, Wippold FJ 2nd. Neurofibromatosis: MR imaging findings involving the head and spine. AJR Am J Roentgenol. 1993;160:159-64. [ ] 18. Bredella MA, Torriani M, Hornicek F, et al. Value of PET in the assessment of patients with neurofibromatosis type 1. AJR Am J Roentgenol. 2007;189:928-35. [ ] 19. Khong PL, Goh WHS, Wong VCN, et al. MR imaging of spinal tumors in children with neurofibromatosis 1. AJR Am J Roentgenol. 2003;180:413-7. [ ] 20. Mena E, Bookstein JJ, Holt JF, et al. Neurofibromatosis and renovascular hypertension in children. Am J Roentgenol Radium Ther Nucl Med. 1973;118:39-45. [ ] 21. Vandenbroucke J, van Ooy A, Geukers C, et al. Dystrophic kyphoscoliosis in neurofibromatosis type I: a report of two cases and review of the literature. Eur Spine J. 1997;6:272-7. [ ] 22. Zeller RD, Dubousset J. Progressive rotational dislocation in kyphoscoliotic deformities: presentation and treatment. Spine (Phila Pa 1976). 2000;25:1092-7. [ ] 23. Felson B. Radiología torácica. 2ª ed. corrigida. Barcelona: Editorial Científico Médica, 1994. [ ] 24. Tsirikos AI, Ramachandran M, Lee J, et al. Assessment of vertebral scalloping in neurofibromatosis type 1 with plain radiography and MRI. Clin Radiol. 2004;59:1009-17. [ ] 25. Hunt JC, Pugh DG. Skeletal lesions in neurofibromatosis. Radiology. 1961;76:1-20. [ ] 26. Gripp KW, Scott CI Jr, Hughes HE, et al. Lateral meningocele syndrome: three new patients and review of the literature. Am J Med Genet. 1997; 70:229-39. [ ] Received November 25, 2009. * Study developed in the Diagnostic Imaging Department - College of Medicine and Hospital de Base in São José do Rio Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554