Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 3 - May / June of 2010
Vol. 43 nº 3 - May / June of 2010
|
ORIGINAL ARTICLE
|
|
Imaging diagnosis and clinical findings of cerebral venous thrombosis in full-term neonates without brain damage: a ten-year review |
|
|
Autho(rs): Alexandra Maria Vieira Monteiro, Claudio Marcio Amaral de Oliveira Lima, Érica Barreiros Ribeiro, Maria Cristina Lins, Silvia Miranda, Luis Eduardo Miranda |
|
|
Keywords: Cerebral venous thrombosis, Full-term neonates, Magnetic resonance imaging, Magnetic resonance angiography, Ultrasonography and Doppler |
|
|
Abstract:
IPhD, Associate Professor of Radiology at Faculdade de Ciências Médicas da Universidade do Estado do Rio de Janeiro (FCM-UERJ), MD, Radiologist at Casa de Saúde São José (CSSJ-RJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION Cerebral venous thrombosis (CVT) in neonates is a severe and rare condition, with an incidence of less than one case for every 100 thousand newborns per year(1,2). This condition has been increasingly diagnosed mainly because the huge developments in diagnostic imaging methods. The most frequent predisposing factor for the development of CVT is hypoxic-ischemic encephalopathy (HIE), with a considerable morbimortality rate(3-6). Clinically, CVT signs and symptoms are nonspecific and may determine delay or failure in the diagnosis(7). In approximately 85% of cases, the thrombosis affects either the superior sagittal sinus or the transverse sinus(8-10). Among the imaging methods, transfontanellar ultrasonography (TFUS) associated with Doppler fluxometry is the initial evaluation method, particularly because of the wide availability and bed-side capability, with low cost, and non-necessity of sedation or ionizing radiation exposure, but magnetic resonance imaging (MRI) remains as the gold standard for the diagnosis of CVT(5,6,9,11,12). The present study was aimed at describing the imaging findings, comparing the methods used in the neonatal period, as well as describing the clinical findings and the neurological progression in four term neonates diagnosed with CVT, with no brain damage, admitted to a neonatal intensive care unit over a 10-year period.
MATERIALS AND METHODS In the period from May 1999 to May 2009, 2,865 neonates were admitted to the Neonatal Intensive Care Unit (ICU) of Casa de Saúde São José (CSSJ) in Rio de Janeiro, RJ, Brazil. Among these neonates, 2,547 were submitted to TFUS as a routine procedure of the ICU, or for different clinical indications, with 10% of such studies being associated with Doppler fluxometry due to a precise indication. In this group, nine full-term neonates were diagnosed with CVT. Two cases of CVT associated with bacterial meningitis, and three associated with the presence of a cerebral lesion were excluded. All of the four selected cases were submitted to magnetic resonance angiography (MR angiography) for diagnosis confirmation. All the neonates underwent evoked auditory potential study to evaluate their degree of auditory loss associated with CVT. All the neonates were male, with gestational age ranging between 37 and 41 weeks (mean, 39 weeks), weight ranging between 3,010 and 4,085 g (mean weight, 3,548 g), and Apgar score at the first minute between 2 and 8 (mean, 5), and at the fifth minute between 7 and 9 (mean, 8). Also, risk factors for CVT were evaluated according to the following classification: neonatal risks (perinatal hypoxia and sepsis), and maternal risks (diabetes and infection, including infections of any etiology, in any region or organ, during the prenatal period). The clinical evaluation of the neonates was based on the presence, or not, of early (up to 24 hours of life) or late onset seizures, and on the presence of respiratory disorders. All the neonates were evaluated by a single pediatric neurologist from their admission to the ICU up to discharge or follow-up abandonment. A Sonoline Versa-Pro ultrasonography unit (Siemens Medical Systems; Erlangen, Germany), with a convex, multifrequency transducer was utilized. Transfontanellar US with Doppler fluxometry was performed through the anterior fontanelle, with acquisition of images in the coronal and sagittal planes. Resistance index (RI) was evaluated for both the right and left middle cerebral artery, anterior cerebral artery, and basilar artery, and was considered as altered in the setting of increased RI in at least two vessels. The venous flow was mapped with color Doppler. MR angiography was performed in a Harmony, 1 tesla unit (Siemens Medical Systems; Erlangen, Germany). The neonates received sedation with chloral hydrate as necessary, and in none of the cases, paramagnetic contrast agent was intravenously administered. The imaging evaluation was aimed at identifying and localizing the thrombosis, its association with parenchymal lesions, and the presence, or not, of hydrocephalus.
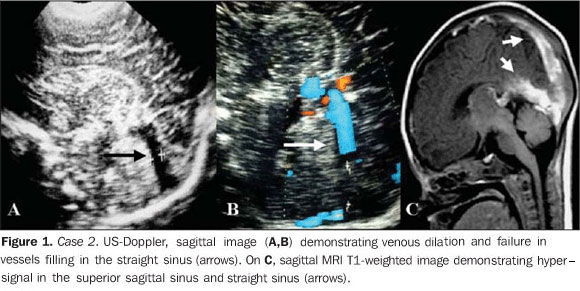
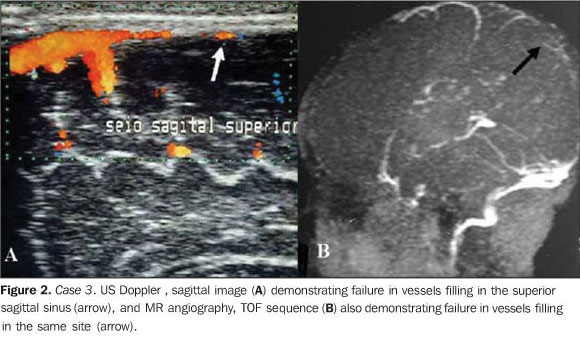
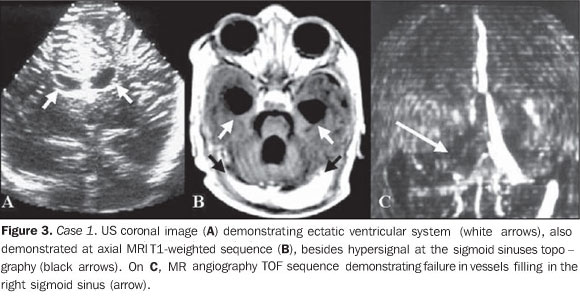
RESULTS Table 1 consolidates the clinical data and imaging findings. The neonatal risk factors observed were associated hypoxia and sepsis in three cases (75%) and hypoxia alone as a single risk factor in one case. As regards maternal risks, the most frequent one was infection in two cases (50%) and diabetes in one (25%). In one case no maternal risk factor was identified. The predominant clinical sign was early seizure onset observed in 100% of cases. Respiratory failure ocurred in the cases 1, 2 and 4, and apnea in one case (25%). The response to evoked auditory potential ranged from normal in two cases (50%), mild/moderate, unilateral auditory loss in one case (25%) and severe, bilateral loss in another case (25%). TFUS was normal in three cases (75%). In the case 2, TFUS identified hypoechoic tubular dilatation diagnosed as venous dilation and absent flow at color Doppler mapping of the straight sinus (Figure 1). Also, the venous Doppler mapping identified flow absence in the superior sagittal sinus, confirmed by MR angiography in the case 3 (Figure 2). In case 1, ectatic ventricular system was observed (Figure 3).
Altered RI in at least two vessels was observed in all the cases, with values ranging between 0.80 and 0.91 (mean, 0.85) for the right middle cerebral artery; between 0.83 and 0.88 (mean, 0.85) for the left middle cerebral artery; between 0.64 and 0.86 (mean, 0.75) for the anterior cerebral artery; and between 0.58 and 0.88 (mean, 0.73) for the basilar artery. The cases with low values for RI were attributed to a mechanism of cerebral self-regulation as a function of arterial redistribution resulting from venous congestion secondary to the thrombosis. Morphological brain MRI was normal in four cases (100%). Cerebral venous thrombosis was diagnosed at T1-weighted sequences complemented by MR angiography. All the sinuses were isolatedly involved. As regards their neurodevelopment, all the neonates progressed within the normality parameters until their discharge or follow-up abandonment.
DISCUSSION The global CVT incidence in children is of 0.67/100,000 children per year, and neonates constitute the most affected group(2,13,14). A retrospective study developed from 1999 to 2006 by Teksam et al.(13) with 71 children divided into three groups (neonates, 0-28 days; infants, 29 days-1 year; children/teenagers, 1-18 years) and diagnosed by computed tomography (CT), CT angiography MRI and MR angiography, reported 48% incidence of CVT in neonates, confirming that this group is more prone to CVT than any other pediatric age range, in spite of the fact that the true incidence rate is still unknown because of the scarcity of reliable epidemiological data(13). It is believed that neonates propensity to CVT is a result from a failure of protective mechanisms caused by cerebral immaturity, besides the presence of physiological prothrombotic factors and peri- and/or postnatal diseases(14,15). According to the literature, CVT is most frequent in male neonates(7,16), in a studied population of 32 neonates(16), similarly to the results of the present study. Risk factors for CVT can be classified into neonatal and maternal. deVeber et al.(2), in a study with 160 children (60 neonates and 91 non-neonates) with ages ranging from NN (gestational age > 36 weeks) to 18 years, have reported the presence of any acute systemic disease in 84% of neonates with CVT and, among them, about 51% and 30% present, respectively, perinatal complications and dehydration as a risk factor for CVT. The most frequent complication was hypoxia in 30 cases, besides premature membrane rupture, maternal infection and gestational diabetes(2). The results of the present study are in agreement with the literature, both in terms of neonatal and maternal risks. In 25% of cases, no maternal risk factor for CVT was observed. It is interesting to note that all the patients were diagnosed with perinatal asphyxia and precociously admitted to the neonatal ICU where, probably, the associated risk factor has been hypoxia and not infection. Therefore, perinatal complications inexorably constitute the most frequent and relevant risk factor for CVT in neonates, probably resulting from the lack of protective mechanisms as a function of immaturity(13). The clinical presentation is highly variable and nonspecific in this age range, and the diversity of associated predisposing factors make the diagnosis difficult and frequently delayed(13). Additionally, the clinical condition is influenced by the child age, extent and site of the thrombosis. Also, according to deVeber et al.(2), 72% of neonates in their study presented some kind of seizure resulting from (HIE) and/or CVT. Besides seizures, most neonates also present some diffuse neurological sign such as agitation or lethargy. This same study shows that 67% of neonates have not presented any focal neurological deficit; on the other hand, hemiparesis, as a clinical sign, has occurred in only 6% of cases, and cranial nerve palsy in 7%. The absence or scarcity of focal signs is explained by the cerebral immaturity. In agreement with the literature, the present study observed the presence of convulsive seizures in all the patients. In the setting of thrombosis, the intraluminal venous pressure increases, reducing the blood flow and the cerebral perfusion pressure, which induces the hematoencephalic barrier disruption and frequently results in vasogenic edema and hydrocephalus(17). In the multicentric study developed by Wasay et al.(1), from 1992 to 2001, with 25 neonates with at least two imaging methods for diagnosis of CVT, hydrocephalus was present in 10% of cases. In the present study, the inclusion criterion was exactly the absence of associated encephalic lesion. In approximately 85% of cases, thrombosis affects the superior sagittal sinus or the transverse sinus(1,17) and in the other 15%, the other sinuses of the dura mater and deep veins of the Galen's system(2,14,18). The involvement of multiple venous sinuses may be present in more than 70% of cases(1,19). The results of the present study presented isolate involvement of venous sinuses. The brainstem auditory evoked response test allows the evaluation of the functional integrity of the auditory tract with several clinical applications, particularly as a method for auditory screening in high-risk neonates, because of its objectivity, rapidity, noninvasiveness, bed-side capabilities and applicability to any age range(20,21). It is estimated that, in Brazil, three to four in every 1,000 children have congenital deafness. This ratio increases to two-four in every 100 neonates when these children come from an ICU. Deafness associated with the occurrence of thrombosis was described by Perlman et al.(22), one of the first authors to demonstrate the cochlear sensitivity to a vascular event. Currently, many studies suggest the existence of a cochlear vessels spasm or increase in blood viscosity associated to vascular events, like in thrombosis, to explain the temporary deafness(21,23). In the present study, in 50% of cases there was an auditory loss ranging from mild to severe. TFUS with Doppler fluxometry presents great advantages, principally the noninvasiveness to measure blood flow velocity in intracranial vessels and to evaluate physiopathological changes in the cerebral hemodynamics, besides the bed-side capability, low cost and non-necessity of sedation and of ionizing radiation exposure(24-27). Several studies on TFUS Doppler fluxometry have demonstrated changes of RI in pathological conditions as, for example, hypoxia with presence of reversed diastolic flow, inclusive, reflecting the increased vascular resistance as a result from edema(17,24). The results of the present study are in agreement with the literature, considering that the increased RI values were observed in all the studied vessels. MR angiography is the most sensitive and specific method for the diagnosis of CVT and, as combined with MRI is considered as gold standard(12,28,29). In agreement with the literature, MR angiography was diagnostic for CVT in 100% of cases in the present study. According to Teksam et al.(13), in a study with 34 neonates with CVT diagnosed by CT, CT angiography, MRI and MR angiography, 62% of neonates with CVT presented an association with parenchymal lesion, with variable location and a predominantly hemorrhagic pattern (76% of cases), but with smaller extent as compared with lesions in older children, and with higher frequency in the frontal and parietal lobes. Additionally, the parenchymal lesion is, in general, correlated with the involved territory of venous drainage (76% of cases). In the present study, association with parenchymal lesion was not observed. The literature reports a survival rate of more than 90% among NN with associated cerebral lesion(14). A Canadian longitudinal study covering an eight-year period reports 8% survival with presence of neurological deficit in 61%, seizures in 21%, and recurrent cerebral thrombosis in 9%(14). Yet, some authors report that the best estimate was observed after 2,1 years, as 77% of neonates diagnosed with CVT were neurologically normal, although the absence of association with parenchymal lesion has not been highlighted(2). As regards the evaluation of the neurological development, all the areas remained within the normality parameters up to the abandonment of the follow-up or contact with the clinician.
CONCLUSION In the neonatal period, combined TFUS and Doppler fluxometry allows the early diagnosis of CVT, which can be confirmed by MRI/ MR angiography, that is the gold standard for the diagnosis of this severe disease. The absence of associated parenchymal lesion may, prospectively, represent the absence of a progressive cerebral damage.
REFERENCES 1. Wasay M, Dai AI, Ansari M, et al. Cerebral venous sinus thrombosis in children: a multicenter cohort from the United States. J Child Neurol. 2008;23:26-31. [ ] 2. deVeber G, Andrew M, Adams C, et al. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001;345:417-23. [ ] 3. De Lorenzi DRS, Tanaka ACd'A, Bozzetti MC, et al. A natimortalidade como indicador de saúde perinatal. Cad Saúde Pública. 2001;17:141-6. [ ] 4. deVeber G, Chan A, Monagle P, et al. Anticoagulation therapy in pediatric patients with sino-venous thrombosis: a cohort study. Arch Neurol. 1998;55:1533-7. [ ] 5. Rivkin MJ. Hypoxic-ischemic brain injury in the term newborn. Neuropathology, clinical aspects, and neuroimaging. Clin Perinatol. 1997;24:607-25. [ ] 6. Silva GS, Almeida CMO, Félix EPV, et al. Trombose venosa cerebral e homocistinúria: relato de caso. Arq Neuropsiquiatr. 2001;59:815-6. [ ] 7. Sébire G, Tabarki B, Saunders DE, et al. Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Brain. 2005;128:477-89. [ ] 8. Khurana DS, Buonanno F, Ebb D, et al. The role of anticoagulation in idiopathic cerebral venous thrombosis. J Child Neurol. 1996;11:248-50. [ ] 9. Marques MCP, Pires LA, Damasceno CA, et al. Trombose da veia de Galeno: relato de caso. Arq Neuropsiquiatr. 2003;61:285-7. [ ] 10. McMurdo SK Jr, Brant-Zawadzki M, Bradley WG Jr, et al. Dural sinus thrombosis: study using intermediate field strength MR imaging. Radiology. 1986;161:83-6. [ ] 11. Lee BCP, Park TS, Kaufman BA. MR angiography in pediatric neurological disorders. Pediatr Radiol. 1995;25:409-19. [ ] 12. Brito AR, Vasconcelos MM, Domingues RC, et al. Pseudotumor cerebral secundário a trombose venosa dural: relato de caso pediátrico. Arq Neuropsiquiatr. 2005;63:697-700. [ ] 13. Teksam M, Moharir M, deVeber G, et al. Frequency and topographic distribution of brain lesions in pediatric cerebral venous thrombosis. AJNR Am J Neuroradiol. 2008;29:1961-5. [ ] 14. Andrew ME, Monagle P, deVeber G, et al. Thromboembolic disease and antithrombotic therapy in newborns. Hematology Am Soc Hematol Educ Program. 2001:358-74. [ ] 15. Klein L, Bhardwaj V, Gebara B. Cerebral venous sinus thrombosis in a neonate with homozygous prothrombin G20210A genotype. J Perinatol. 2004;24:797-9. [ ] 16. Golomb MR, Dick PT, MacGregor DL, et al. Neonatal arterial ischemic stroke and cerebral sinovenous thrombosis are more commonly diagnosed in boys. J Child Neurol. 2004;19:493-7. [ ] 17. Heinz ER, Provenzale JM. Imaging findings in neonatal hypoxia: a practical review. AJR Am J Roentgenol 2009;192:41-7. [ ] 18. Ferreira CS, Pellini M, Boasquevisque E, et al. Alterações parenquimatosas na trombose venosa cerebral: aspectos da ressonância magnética e da angiorressonância. Radiol Bras. 2006;39:315-21. [ ] 19. Huang BY, Castilllo M. Hypoxic-ischemic brain injury: imaging findings from birth to adulthood. Radiographics. 2008;28:417-39. [ ] 20. Lourenço EA, Oliveira MH, Umemura A, et al. Audiometria de resposta evocada de acordo com sexo e idade: achados e aplicabilidade. Rev Bras Otorrinolaringol. 2008;74:545-51. [ ] 21. Maia RA, Cahali S. Surdez súbita. Rev Bras Otorrinolaringol. 2004;70:238-48. [ ] 22. Perlman HB, Kimura R, Fernandez C. Experiments on temporary obstruction of the internal auditory artery. Laryngoscope. 1959;69:591-613. [ ] 23. Barreira-Nielsen C, Futuro Neto HA, Gattaz G. Processo de implantação de programa de saúde auditiva em duas maternidades públicas. Rev Soc Bras Fonoaudiol. 2007;12:99-105. [ ] 24. Garcia MHM, Monteiro AMV, Freire SM. Relação entre o índice de resistência obtido pela ultra-sonografia Doppler transfontanela e o neurodesenvolvimento até o primeiro ano de vida em recém-nascidos a termo com encefalopatia hipóxico-isquêmica leve e moderada. Arq Neuropsiquiatr. 2007;65:1206-10. [ ] 25. Mello RR, Meio MDBB, Morsch DS, et al. Ultra-sonografia cerebral neonatal normal no prematuro - é possível tranqüilizar os pais? J Pediatr (Rio J). 1999;75:45-9. [ ] 26. Taylor GA. Recent advances in neonatal cranial ultrasound and Doppler techniques. Clin Perinatol. 1997;24:677-91. [ ] 27. Ipsiroglu OS, Eichler F, Stoeckler-Ipsiroglu S. Cerebral Doppler sonography of the neonate. A résumé after 20 years and future aspects. Clin Perinatol. 1999;26:905-46. [ ] 28. Gasparetto EL. Trombose venosa cerebral [editorial]. Radiol Bras. 2006;39(5):iii. [ ] 29. Chao CP, Zaleski CG, Patton AC. Neonatal hypoxic-ischemic encephalopathy: multimodality imaging findings. Radiographics. 2006;26:S159-72. [ ] Received March 16, 2010. * Study developed at Casa de Saúde São José (CSSJ-RJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554