Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 54 nº 3 - May / June of 2021
Vol. 54 nº 3 - May / June of 2021
|
ORIGINAL ARTICLES
|
|
Evaluation of variations of the glenoid attachment of the inferior glenohumeral ligament by magnetic resonance arthrography |
|
|
Autho(rs): Marcelo Novelino Simão1,2,a; Maximilian Jokiti Kobayashi3,b; Matheus de Andrade Hernandes1,2,c; Marcello Henrique Nogueira Barbosa2,d |
|
|
Keywords: Shoulder; Ligaments, articular/anatomy & histology; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
Traumatic shoulder instability is a common condition, with an estimated prevalence of approximately 2% in the general population(1,2). Lesions associated with anterior traumatic shoulder dislocation include bone fractures, such as Hill–Sachs and Bankart lesions, and soft tissue injuries, such as cartilaginous Bankart lesion and its variants. Other shoulder lesions, such as those involving the inferior glenohumeral ligament (IGHL), have also been described in the literature(3). Humeral avulsion of the glenohumeral ligament (HAGL) reportedly occurs in up to 9.3% of cases of traumatic shoulder dislocation(4). Variations of IGHL lesions described in the literature include avulsion of a bone fragment off the humeral attachment, known as bony HAGL, avulsion of the humeral and glenoid attachments, known as a floating IGHL, and injury associated with posterior dislocation, known as reverse HAGL(5,6). Other possibilities are isolated avulsion of the IGHL off the glenoid rim without lesion of the anterior glenoid labrum, which can be related to detachment but does not involve a tear of the capsular-ligamentous or periosteal complexes(6,7), known as anterior labroligamentous inferior periosteal sleeve avulsion (ALIPSA), or complete capsular-ligamentous avulsion with periosteal tear(2,3), known as glenoid avulsion of the glenohumeral ligament (GAGL), although there is some controversy over these definitions. While the imaging features of some anatomical variations of the labral aspect or in different capsular, tendinous, and perilabral shoulder attachment patterns, such as the biceps-labral complex, are well-known and have been intensively studied(8,9), variations of the IGHL attachment to the anterior glenoid rim are less common research topics. Most studies in the radiology literature provide only a generic description of the glenoid attachment of the anterior and posterior bands of the IGHL, stating they emerge from the labrum at the middle and lower thirds of the glenoid(6,10–15) or simply from the glenoid rim(16,17), and rarely do we find a more detailed description stating that they originate from the glenoid rim, labrum, and periosteum(2). However, anatomical studies indicate greater variability in the pattern of IGHL glenoid attachment, which can originate from the chondrolabral complex or directly from the glenoid rim(18,19), what Eberly(19) refers to as type I and type II glenoid attachment, respectively. During arthroscopy, it is common to find that the IGHL and the chondrolabral junction cannot be clearly separated at the anteroinferior glenoid rim, a variant known as the labralligamentous complex(20). Several imaging methods can contribute to the diagnosis of lesions associated with traumatic dislocation, including conventional X-ray, conventional magnetic resonance imaging (MRI), magnetic resonance (MR) arthrography, and even ultrasound(6,7,21,22), although MR arthrography is considered the gold standard for the preoperative assessment(23). To our knowledge, there have been no imaging studies aimed at assessing the different patterns of IGHL attachment to the glenoid rim, which could help in the interpretation of this complex anatomy and the associated lesions. Although an isolated lesion of the IGHL glenoid attachment is rare, it is important to recognize it because, when found in arthroscopies of patients with traumatic shoulder instability, it requires fixation, even if the fibrocartilaginous labrum is intact(2,24). Diagnosing such a lesion with MR arthrography is considered challenging, and some authors argue that the most appropriate arthroscopic approach for diagnosing and assessing the extent of the lesion is the anterior portal(24). A better understanding of the anatomy of the IGHL, combined with the recognition of the different patterns of glenoid attachment, improves the diagnostic capacity of MR arthrography. In addition, details about the lesions obtained during the preoperative assessment with MR arthrography can facilitate the choice of the appropriate surgical techniques and lead to better treatment outcomes. In light of this, the objectives of this retrospective study were to assess MR arthrography examinations of the shoulder in order to characterize the anatomy of the IGHL attachment to the glenoid rim. We also evaluated the interobserver and intraobserver agreement for the findings. MATERIALS AND METHODS This was a retrospective study carried out in the radiology and diagnostic imaging department of the university hospital of our institution. The study was approved by the research ethics committee of the institution (Reference no. 36029414.7.0000.5440). Because of the retrospective nature of the study, the requirement for written informed consent was waived. We selected 137 consecutive MR arthrography examinations of the shoulder performed at the university hospital or at a private diagnostic imaging clinic between 2011 and 2013. We applied the following exclusion criteria for MR arthrography examinations of the shoulder: failure to follow the standard protocol (i.e., no acquisition of volumetric sequences); unsatisfactory image quality because of motion or magnetic susceptibility artifacts; poor distension of the joint capsule by the contrast medium; postoperative acquisition; and extensive lesion of the anterior labrum. On the basis of the study criteria, 44 examinations were excluded. Therefore, the final sample comprised 93 MR arthrography examinations of the shoulder. Of the 93 corresponding patients, 70 (75.3%) were male, with a mean age of 28 ± 9.3 years (range, 14–70 years), and 23 (24.7%) were female, with a mean age of 32 ± 13.2 years (range, 13–65 years). There were 70 patients with a history of traumatic instability, the remaining 23 patients having nothing in their clinical history, medical record, or pre-examination interview that could lead to a suspicion of instability. MR arthrography protocols The MR arthrography examinations involved the acquisition of at least one volumetric sequence in the axial plane (Table 1), which was the only sequence used for assessment in this study. All images were acquired in one of the following MRI scanners: – A 1.5-T Philips Achieva (Philips Medical Systems, Cleveland, OH, USA), with a SENSE-Shoulder-4 or SENSE-Flex-M coil and acquisition of at least one of the following sequences: three-dimensional (3D) T1-weighted; 3D T1-weighted; 3D T1-weighted VISTA; or proton density-weighted VISTA ISO – A 1.5-T Signa HDxt (GE Medical Systems, Milwaukee, WI, USA), with a SHLDRPA4 coil and acquisition of a 3D FIESTA sequence – A 3.0-T Discovery MR750 (GE Medical Systems, Milwaukee, WI, USA), with an HD Shoulder coil and acquisition of a 3D FIESTA sequence Data analysis The images were archived and anonymized, after which they were interpreted by two radiologists, a fellow in musculoskeletal radiology (reader 1) and a senior musculoskeletal radiologist at our institution with four years of experience (reader 2). The two readers, who were working independently, were blinded to the clinical history, signs/ symptoms, surgical findings, examination reports, and clinical evolution of the patients. For the assessment of intraobserver agreement, one of the observers (reader 1) re-evaluated the findings six months after the first reading. We conducted a retrospective analysis of the cases in order to characterize the following: the glenoid attachment pattern of the anterior band of the IGHL (AB-IGHL), distinguishing between type I, in which the AB-IGHL has a predominantly chondrolabral origin (Figure 1A), and type II, in which it emerges directly from the glenoid rim (Figure 1b); and the AB-IGHL glenoid attachment as a clock position—12 o’clock when it emerged at the upper portion, 3 o’clock when it emerged at the mid-anterior position, and 6 o’clock when it emerged at the lower position—using the multiplanar reconstruction tool of the OsiriX software package (64-bit version; Pixmeo, Geneva, Switzerland) in a three-dimensional volumetric sequence (Figures 2 and 3). 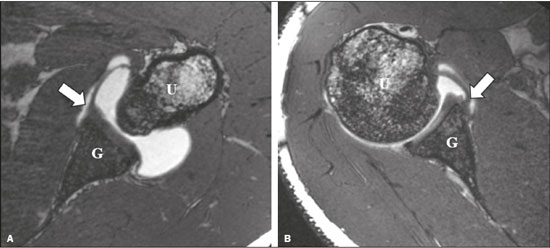 Figure 1. Variations of the AB-IGHL labrum-periosteal glenoid attachment. Axial 3D FIESTA volumetric sequence of the shoulder showing the AB-IGHL (arrow) originating mainly from the labrum—a type I attachment pattern (A); and the AB-IGHL (arrow) originating predominantly from the bone margins of the glenoid—a type II attachment pattern (B). G, glenoid; H, humerus. 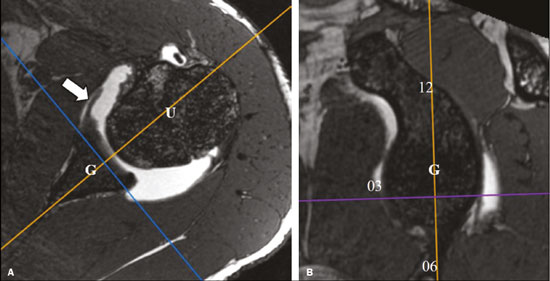 Figure 2. Multiplanar reconstruction tool of OsiriX software on an axial 3D FIESTA volumetric sequence showing the sagittal reconstruction reference lines (A); and the sagittal reconstruction plane to identify the level of AB-IGHL attachment to the glenoid rim (arrow) in relation to the 12 o’clock (12), 3 o’clock (03), and 6 o’clock (06) positions (B). G, glenoid; H, humerus. 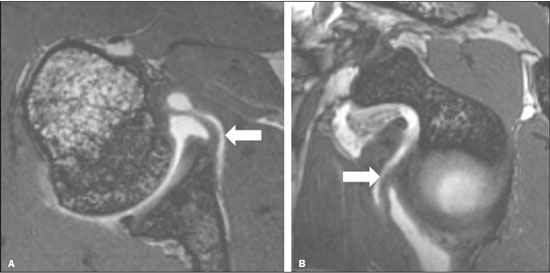 Figure 3. A 30-year-old male patient with no history of traumatic shoulder instability. A: Axial 3D FIESTA sequence showing the IGHL emerging directly from the glenoid rim (arrow)—a type II pattern. B: Sagittal reconstruction showing the IGHL glenoid attachment at the 3 o’clock position (arrow). Statistical analysis The statistical analysis was performed with the Statistical Analysis System(24), version 9.0 (SAS Institute Inc., Cary, NC, USA). We used the chi-square test to determine whether the types of attachment were associated with the of the AB-IGHL attachment level. The interpretation of presence or absence of glenohumeral dislocation/instabil-the agreement analysis results was based on the following ity and labral injury. We used the kappa statistic with a criteria(25,26): no agreement (κ < 0); poor agreement (κ of 95% confidence interval (95% CI) for the evaluation of 0–0.19); fair agreement (κ of 0.20–0.39); moderate agreeinterobserver and intraobserver agreement rates, whereas ment (κ of 0.40–0.59); substantial agreement (κ of 0.60– we used the weighted kappa statistic for the evaluation 0.79); and almost perfect agreement (κ of 0.80–1.00). RESULTS Variation in the AB-IGHL glenoid attachment The AB-IGHL emerged from the chondrolabral rim (type I pattern) in 50 cases (53.8%) and directly from the glenoid rim (type II pattern) in 43 cases (46.2%). The evaluation of the attachment pattern achieved near-perfect interobserver agreement (κ = 0.91; 95% CI: 0.83–0.99) and intraobserver agreement (κ = 0.87; 95% CI: 0.77–0.97). After the cases in which the physician request or the patient interview indicated suspicion or complaint of dislocation, instability, or labral injury had been excluded, the sample comprised 23 patients without a clinical history of instability. Of those 23 patients, 15 (65%) had a type I attachment pattern and 8 (35%) had a type II attachment pattern. We found no significant association between the type of attachment pattern and the presence or absence of glenohumeral dislocation/instability and labral injury (p = 0.20). Level of AB-IGHL attachment to the anterior glenoid rim The AB-IGHL attached to the glenoid rim at the 4 o’clock position in 58 cases (62.4%), at the 3 o’clock position in 14 (15%), and at the 5 o’clock position in 21 (22.6%). In the assessment of the ligament attachment position, there was substantial interobserver agreement (κ = 0.79; 95% CI: 0.65–0.90) and intraobserver agreement (κ = 0.70; 95% CI: 0.56–0.83). DISCUSSION Several recent studies conducted in Brazil have highlighted the importance of using imaging methods for evaluating the musculoskeletal system(27–31). The anatomy of the glenohumeral ligaments is complex and variable, various patterns having been described in the literature, which makes it difficult to gain a proper understanding of it. Although the IGHL is probably the most widely studied of those ligaments, there is as yet no consensus about its level of origin, size, and most common attachment pattern(32). The results of the present study confirm those of previous studies showing anatomical variations in the attachment of the AB-IGHL. More than 46% of the cases in our sample had an IGHL attached to the glenoid rim, medial to the fibrocartilage of the glenoid labrum. For the identification of that anatomical variation, the interobserver and intraobserver agreement were almost perfect. Although there are anatomical studies in the literature focusing on the assessment of the different glenoid attachment patterns(18,19,33), descriptions of those aspects on MRI or MR arthrography examinations are less common. In our study, the use of MR arthrography enabled us to analyze a sample larger than those of previous anatomical studies. We were able to identify the IGHL in all 93 of the examinations analyzed, which confirms that MR arthrography is an excellent method for assessing this ligament and that it can be used in routine practice. In addition, the characterization of the anatomy of the AB-IGHL glenoid attachment by a radiologist with experience in the method proved to be reproducible and reliable. Although reports in the literature state that diagnosing isolated lesions of the IGHL glenoid attachment (known as ALIPSA/GAGL lesions) with MR arthrography is a challenge and that arthroscopy is the method of choice in those cases(24), we believe that a better understanding of the IGHL variations and their depiction on MR arthrography can contribute to changing that idea. Anatomical studies of the variations of the AB-IGHL attachment to the glenoid rim show a predominance of the type I pattern, in which most fibers originate from the chondrolabral rim and some extend to the glenoid rim, with incidence rates of 80–88%, over the type II pattern, in which they originate directly from the bone margin(18,19). In the present study, a predominance of the type I pattern was observed, although the prevalence of the type II pattern, in which the AB-IGHL attaches mainly to the glenoid rim and neck, was also found to be high. A possible reason for that is a selection bias—many patients selected for inclusion in the present study had undergone MR arthrography because of complaints of traumatic shoulder instability, resulting in a specific population that differs from that of asymptomatic people. In an attempt to obtain an unbiased sample, cases in which there was suspicion or a complaint of glenohumeral instability and cases of shoulder dislocation were excluded, after which a new analysis was carried out. In that second analysis, the distribution of the two types was more similar to that reported in previous anatomical studies: type I and type II attachment patterns were observed in 65.2% and 34.8% of the cases, respectively. However, there was no association between the type of glenoid attachment and the presence or absence of glenohumeral instability/dislocation and labral injury. Because we did not make any arthroscopic correlation, we cannot rule out completely the possibility that some of the patients in our sample had an ALIPSA/GAGL lesion, in which there is avulsion of the IGHL attachment from the glenoid without damage to the anteroinferior labrum(2,3,6,7). Because their findings on imaging examinations are similar, ALIPSA/GAGL lesions can mimic a type II attachment pattern. However, ALIPSA/GAGL lesions are considered quite uncommon, accounting for less than 3% of the labral-ligamentous lesions in patients with a history of shoulder instability(7). Although it is difficult to distinguish between these two conditions on MR arthrography, the presence of a fibrocartilaginous labrum well adhered to the glenoid rim clearly distinguishes a Bankart or Perthes lesion from an ALIPSA/GAGL lesion or a type II attachment of the IGHL to the glenoid rim. The results of this study, in which we found an IGHL glenoid attachment position between 3 o’clock and 5 o’clock, are in agreement with those of anatomical studies of frozen cadavers, which found attachment positions starting at 3 o’clock, with decreasing thickness toward the lower part of the glenoid(19), as well as between 2 o’clock and 5 o’clock, the extent of the attachment being greatest at the 4 o’clock position(18). Our study has some limitations. First, because it was a retrospective study, the clinical data used were based on the summarized information available on physician requests, electronic medical records, and pre-examination interviews. In addition, there was no standardization of the volume injected into the joint or of the examination protocol. However, a prospective study involving an invasive procedure could raise ethical questions. In addition, although the observers were blinded to the clinical history of patients, findings such as Hill–Sachs and Bankart lesions often made it obvious which cases had a history of traumatic instability. Another limitation is the fact that there is no method of reference or gold standard to confirm the findings of the MR arthrography examinations, which indicates the need for further studies in that area. Furthermore, there could have been a selection bias, given that most of the patients in our sample had a clinical history of shoulder instability, which could affect the usual anatomical aspect of the IGHL-labrum complex. To minimize that limitation, we performed a second analysis, in which cases with a history or signs of instability were excluded. However, as previously mentioned, that analysis was based only on the data available on the physician request and not on a detailed clinical evaluation of the patients. Despite the abovementioned limitations, there are reasons to believe that the results of our study are useful, because they are in agreement with the attachment patterns and levels found in previous anatomical studies, as well as being consistent and having almost perfect interobserver and intraobserver agreement. As in the assessment of other joints, such as the knee menisci(34), identifying these anatomical variations around the anterior glenoid rim on MR arthrography is important for the correct interpretation of the imaging findings. The treatment of traumatic shoulder instability is often surgical and depends on an accurate preoperative diagnosis and careful planning for each type and degree of injury. Therefore, we can conclude that MR arthrography provides an effective assessment of the anatomy as well as of the different patterns and positions of the AB-IGHL glenoid attachment and that radiologist knowledge about them can contribute to a better understanding of the anatomical variations and of less common lesions of the IGHL-labrum complex associated with anterior shoulder instability, which help achieve correct diagnoses and more appropriate treatment planning. REFERENCES 1. Vasconcelos UMR, Leonardi ABA, Reis AL, et al. Instabilidade ântero-inferior traumática do ombro: procedimento de Bankart em atletas não profissionais. Acta Ortop Bras. 2003;11:150–7. 2. Mannem R, DuBois M, Koeberl M, et al. Glenoid avulsion of the glenohumeral ligament (GAGL): a case report and review of the anatomy. Skeletal Radiol. 2016;45:1443–8. 3. Wolf EM, Siparsky PN. Glenoid avulsion of the glenohumeral ligaments as a cause of recurrent anterior shoulder instability. Arthroscopy. 2010;26:1263–7. 4. Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11:600–7. 5. Field LD, Bokor DJ, Savoie FH 3rd. Humeral and glenoid detachment of the anterior inferior glenohumeral ligament: a cause of anterior shoulder instability. J Shoulder Elbow Surg. 1997;6:6–10. 6. Steinbach LS. MRI of shoulder instability. Eur J Radiol. 2008;68: 57–71. 7. Tian CY, Cui GQ, Zheng ZZ, et al. The added value of ABER position for the detection and classification of anteroinferior labroligamentous lesions in MR arthrography of the shoulder. Eur J Radiol. 2013;82:651–7. 8. Smith DK, Chopp TM, Aufdemorte TB, et al. Sublabral recess of the superior glenoid labrum: study of cadavers with conventional nonenhanced MR imaging, MR arthrography, anatomic dissection, and limited histologic examination. Radiology. 1996;201:251–6. 9. Simão MN, Vinson EN, Spritzer CE. Magnetic resonance imaging evaluation of meniscoid superior labrum: normal variant or superior labral tear. Radiol Bras. 2016;49:220–4. 10. Yeh L, Kwak S, Kim YS, et al. Anterior labroligamentous structures of the glenohumeral joint: correlation of MR arthrography and anatomic dissection in cadavers. AJR Am J Roentgenol. 1998; 171:1229–36. 11. Shankman S, Bencardino J, Beltran J. Glenohumeral instability: evaluation using MR arthrography of the shoulder. Skeletal Radiol. 1999;28:365–82. 12. Chung CB, Corrente L, Resnick D. MR arthrography of the shoulder. Magn Reson Imaging Clin N Am. 2004;12:25–38. 13. Woertler K, Waldt S. MR imaging in sports-related glenohumeral instability. Eur Radiol. 2006;16:2622–36. 14. Boulet C, De Maeseneer M, Pouliart N, et al. Magnetic resonance arthrography of glenohumeral lesions: anatomy and arthroscopically confirmed pathology. Can Assoc Radiol J. 2012;63:79–86. 15. Ramirez Ruiz FA, Baranski Kaniak BC, Haghighi P, et al. High origin of the anterior band of the inferior glenohumeral ligament: MR arthrography with anatomic and histologic correlation in cadavers. Skeletal Radiol. 2012;41:525–30. 16. Connell DA, Potter HG. Magnetic resonance evaluation of the labral capsular ligamentous complex: a pictorial review. Australas Radiol. 1999;43:419–26. 17. Takubo Y, Horii M, Kurokawa M, et al. Magnetic resonance imaging evaluation of the inferior glenohumeral ligament: non-arthrographic imaging in abduction and external rotation. J Shoulder Elbow Surg. 2005;14:511–5. 18. Itoigawa Y, Itoi E, Sakoma Y, et al. Attachment of the anteroinferior glenohumeral ligament-labrum complex to the glenoid: an anatomic study. Arthroscopy. 2012;28:1628–33. 19. Eberly VC, McMahon PJ, Lee TQ. Variation in the glenoid origin of the anteroinferior glenohumeral capsulolabrum. Clin Orthop Relat Res. 2002;(400):26–31. 20. Passanante GJ, Skalski MR, Patel DB, et al. Inferior glenohumeral ligament (IGHL) complex: anatomy, injuries, imaging features, and treatment options. Emerg Radiol. 2017;24:65–71. 21. Simão MN, Nogueira-Barbosa MH, Muglia VF, et al. Anterior shoulder instability: correlation between magnetic resonance arthrography, ultrasound arthrography and intraoperative findings. Ultrasound Med Biol. 2012;38:551–60. 22. Ruiz Santiago F, Martínez Martínez A, Tomás Muñoz P, et al. Imaging of shoulder instability. Quant Imaging Med Surg. 2017;7:422– 33. 23. Bak K, Wiesler ER, Poehling GG, ISAKOS Upper Extremity Committee. Consensus statement on shoulder instability. Arthroscopy. 2010;26:249–55. 24. O’Reilly OC, Andrews KA, Siparsky PN. Understanding the glenoid avulsion of the glenohumeral ligaments as a cause of shoulder instability: surgical and postsurgical management. Arthrosc Tech. 2019;8:e1153–e1158. 25. SAS Institute Inc. SAS/STAT® 9.0 user’s guide. Cary, NC: SAS Institute Inc.; 1999. 26. Landis JR, Kock GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. 27. Helito PVP, Rocha SRR, Ortiz RT, et al. Accuracy of magnetic resonance imaging for diagnosing hallux valgus. Radiol Bras. 2020;53: 81–5. 28. Dalto VF, Assad RL, Lorenzato MM, et al. Comparison between STIR and T2-weighted SPAIR sequences in the evaluation of inflammatory sacroiliitis: diagnostic performance and signal-to-noise ratio. Radiol Bras. 2020;53:223–8. 29. Souza ARM, Castro AA, Fonseca EKUN, et al. Magnetic resonance imaging aspects after surgical repair of knee cartilage: pictorial essay. Radiol Bras. 2020;53:201–7. 30. Enge Júnior D, Castro AA, Fonseca EKUN, et al. Main complications of hip arthroplasty: pictorial essay. Radiol Bras. 2020;53:56–62. 31. Fiorentini LF, Stüker G, Pacini GS, et al. Upper-limb magnetic resonance lymphangiography: a useful new technique. Radiol Bras. 2019;52:378–9. 32. Chahla J, Aman ZS, Godin JA, et al. Systematic review of the anatomic descriptions of the glenohumeral ligaments: a call for further quantitative studies. Arthroscopy. 2019;35:1917–26.e2. 33. Bukart AC, Debsky RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res. 2002;(400):32–9. 34. Simão MN, Nogueira-Barbosa MH. Magnetic resonance imaging in the assessment of meniscal anatomic variants and of the perimeniscal ligamentous anatomy: potential interpretation pitfalls. Radiol Bras. 2011;44:117–22. 1. Central Diagnóstico de Ribeirão Preto (Cedirp), Ribeirão Preto, SP, Brazil 2. Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 3. Digimax Medicina Diagnóstica, Caçador, SC, Brazil a. https://orcid.org/0000-0002-2164-1910 b. https://orcid.org/0000-0001-5888-5081 c. https://orcid.org/0000-0002-2244-5532 d. https://orcid.org/0000-0002-7436-5315 Correspondence: Dr. Marcelo Novelino Simão Rua João Alfredo Tardelli, 100, casa 110, Jardim Saint Gerard Ribeirão Preto, SP, Brasil, 14022- 038 E-mail: marcelo_simao@hotmail.com Received 13 April 2020 Accepted after revision 22 June 2020 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
