Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 5 - Sep. / Oct. of 2019
Vol. 52 nº 5 - Sep. / Oct. of 2019
|
LETTERS TO THE EDITOR
|
|
Disseminated intramuscular cysticercosis diagnosed incidentally in a patient with joint pain |
|
|
Autho(rs): Denise Maria Rissato Camilo1; Tiago Kojun Tibana2; Rômulo Florêncio Tristão Santos3; Edson Marchiori4; Thiago Franchi Nunes5 |
|
|
Dear Editor,
A 43-year-old male resident of a rural area presented with a two-month history of pain in his right leg, predominantly in the hip region, the pain having progressively increased in intensity. Physical examination showed mild pain during active and passive movement of the limb. Laboratory tests showed no significant changes, except for a slightly elevated erythrocyte sedimentation rate. A plain X-ray demonstrated multiple radiopaque rhizoid images, distributed throughout various muscle planes (Figures 1A and 1B). Computed tomography revealed numerous calcifications in the muscle groups of both legs (Figures 1C and 1D). The diagnostic hypothesis was muscular cysticercosis. Pathological analysis of a muscle tissue sample confirmed that diagnosis. The patient was started on a 30-day course of albendazole and prednisone, which resulted in improvement of all of the signs and symptoms. 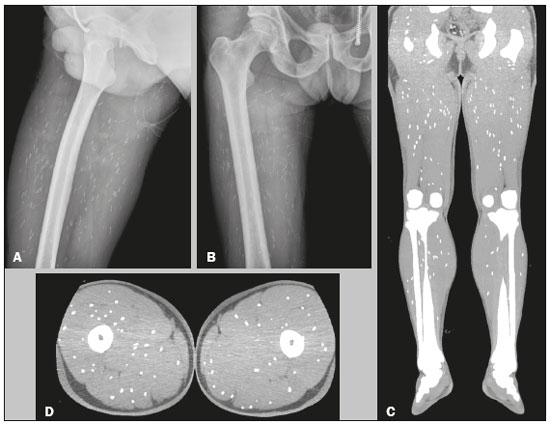 Figure 1. Plain X-rays (A,B) showing radiopaque rhizoid images in the muscle planes. Coronal and axial computed tomography scans (C and D, respectively) showing diffuse intramuscular calcifications. Diseases caused by uncommon infectious agents have recently been described in the radiology literature of Brazil(1–4). Taeniasis and cysticercosis are two distinct entities. Although cestodes of the same genus are responsible for both diseases, the stage of the cestode at infection differs between the two. Taeniasis is caused by the adult forms of Taenia solium or Taenia saginata infesting the small intestine of its definitive host, human beings. However, cysticercosis is caused by the larval form of tapeworms infesting the tissues of its intermediate hosts (pigs and cows). In human cysticercosis, humans are categorized as accidental intermediate hosts(5). The eggs enter the human intestine by fecal–oral contamination, by autoinfection, or by ingestion of contaminated food or water(6). Eggs develop into larvae that spread throughout the intestinal wall and are disseminated through the bloodstream to the brain, muscles, subcutaneous tissues, or other organs(5). Cysticercosis is endemic in many parts of the world, particularly in Latin America, Africa, and Asia. However, a trend toward gradual growth is observed in developed countries, due to the increase in travel and immigration(7,8). The preferred sites of infestation are the central nervous system, in 70–80% of cases; the eye, in 18–20% of cases; the skin, in 10–12% of cases; and the musculature, in 5–6% of cases. Infestation of the musculature does not result in specific clinical symptoms or signs. In most cases, the symptoms are mild. Muscle pains and weakness can occur, as can lower limb paresthesia and hydrarthrosis of the knee. Significantly altered muscle function, with evident changes on physical examination, is rare. The muscular form of cysticercosis has been identified as an incidental finding on radiological examinations that focus on the soft tissues and demonstrate the characteristic calcifications(9). The treatment of intramuscular cysticercosis depends on the presence of symptoms, especially on whether there is pain or a local inflammatory process. Treatment modalities include the use of anthelmintics such as albendazole and praziquantel (in patients with viable cysts), the use of corticosteroids or other agents to suppress or prevent the immune response of the host, and surgical intervention in selected cases(10,11). REFERENCES 1. Frota Júnior JH, Pereira MAH, Lopes PGM, et al. Intestinal strongyloidiasis: radiological findings that support the diagnosis. Radiol Bras. 2017;50:137–8. 2. Mogami R, Vaz JLP, Chagas YFB, et al. Ultrasound of ankles in the diagnosis of complications of chikungunya fever. Radiol Bras. 2017;50: 71–5. 3. Niemeyer B, Muniz BC, Gasparetto EL, et al. Reply: Congenital Zika syndrome and neuroimaging findings. Radiol Bras. 2017;50:405. 4. Barbosa DL, Hochhegger B, Souza Jr AS, et al. High-resolution computed tomography findings in eight patients with hantavirus pulmonary syndrome. Radiol Bras. 2017;50:148–53. 5. Saeed N, Ehsan A, Vasenwala SM. Disseminated cysticercosis incidentally diagnosed in a patient of fracture shaft of femur. BMJ Case Rep. 2017;28:2017. 6. Yamashita S, Mesquita MVGBC, Machado JCM, et al. Cisticercose intramedular: relato de caso e revisão da literatura. Radiol Bras. 2003; 36:255–7. 7. Sharma BS, Banerjee AK, Kak VK. Intramedullary spinal cysticercosis. Case report and review of literature. Clin Neurol Neurosurg. 1987;89:111–6. 8. Liu H, Juan YH, Wang W, et al. Intramuscular cysticercosis: starry sky appearance. QJM. 2014;107:459–61. 9. Armbrust-Figueiredo J, Speciali JG, Lison MP. Forma miopática da cisticercose. Arq Neuro-Psiquiatr (São Paulo). 1970;28:385–90. 10. Nash TE. Human case management and treatment of cysticercosis. Acta Trop. 2003;87:61–9. 11. Tripathy SK, Sen RK, Akkina N, et al. Role of ultrasonography and magnetic resonance imaging in the diagnosis of intramuscular cysticercosis. Skeletal Radiol. 2012;41:1061–6. 1. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0002-9016-8610 2. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0001-5930-1383 3. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0002-8679-7369 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil; https://orcid.org/0000-0001-8797-7380 5. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; https://orcid.org/0000-0003-0006-3725 Correspondence: Dr. Thiago Franchi Nunes Avenida Senador Filinto Müller, 355, Vila Ipiranga Campo Grande, MS, Brasil, 79080-190 E-mail: thiagofranchinunes@gmail.com Received 13 November 2017. Accepted after revision 22 December 2017. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554