Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 5 - Sep. / Oct. of 2019
Vol. 52 nº 5 - Sep. / Oct. of 2019
|
LETTERS TO THE EDITOR
|
|
Monostotic fibrous dysplasia invading the inferior turbinate: computed tomography and magnetic resonance imaging findings |
|
|
Autho(rs): Mustafa Resorlu1; Ozan Karatag2; Fatma Uysal3; Ozge Caglar4 |
|
|
Dear Editor
A 25-year-old woman presented to our hospital with a headache and nasal congestion. Although she reported a one-year history of nasal congestion, she had no chronic diseases. On local examination, the inferior turbinate was enlarged and hard. Systemic cutaneous examination revealed no pathology. Magnetic resonance imaging (MRI), performed to investigate the headache, showed a 3 × 1.5 × 1.0 cm lesion in the right inferior turbinate (Figure 1). On T1- and T2-weighted images, the lesion was hypointense with well-defined margins. Computed tomography (CT) of the paranasal sinus showed that the turbinate was enlarged, and that the mass causing the expansion was homogeneous and hyperdense (Figure 2). No soft tissue invasion or bone destruction was seen on CT or MRI. The patient was treated with surgical excision and was discharged without complications. 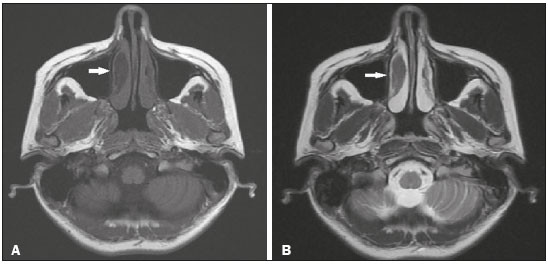 Figure 1. Axial T1- and T2-weighted MRI sequences (A and B, respectively), showing a hypointense lesion (arrow) consistent with FD. 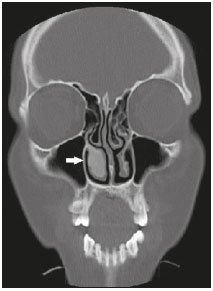 Figure 2. CT of the paranasal sinus showing a ground-glass opacity causing expansion of the right inferior turbinate (arrow). Fibrous dysplasia (FD) is a benign skeletal disorder characterized by fibroblastic proliferation. Although factors such as genetics and trauma have been implicated, the etiology remains uncertain. Involvement of the facial bones is rare, and when present, the maxilla and mandible are commonly affected(1). Inferior turbinate involvement has previously been reported in only a few cases. In cases of FD with craniofacial involvement, the clinical findings include facial asymmetry, nasal obstruction, and pain. Involvement of the inferior turbinate has been reported in only a few cases. Karligkiotis et al.(2) reported the first such case in 2012, describing a 6-month history of persistent nasal obstruction in a 68-year-old woman who was subsequently treated with corticosteroids. The diagnosis is typically made on the basis of the radiological findings. The radiological findings vary depending on bone matrix development within the lesion and the amount of that matrix. It may assume the form of ground-glass opacity or a radiolucent lytic area(3). The differential diagnosis includes Paget's disease and ossifying fibroma. Three different CT imaging patterns have been reported in FD(2,4): ground-glass (the most common and characteristic); sclerotic; and lytic. MRI is used for diagnostic purposes or to show relationships with the adjacent anatomical structures. On T1- and T2-weighted images, the lesion is sharply marginated and hypointense. However, the diagnostic efficacy of MRI decreases when the signal is hyperintense on T2-weighted images in particular(3). Lysis developing in the area of an FD lesion, calcified foci, a periosteal reaction contiguous to the lesion, a cortical defect, and a soft-tissue mass observed at radiology indicate malignant transformation. In monostotic FD, malignant transformation is more common in individuals with craniofacial involvement than in those with involvement of other bones. The most common malignant transformation of FD is to osteosarcoma(4). In the case presented here, homogeneous ground-glass opacity, which is typical of FD, was seen on CT. The preliminary diagnosis of FD, based on the radiological findings, was confirmed by histopathology. In patients with FD, small, asymptomatic lesions not causing any cosmetic deformity can be monitored. Patients in pain can be treated with bisphosphonates, vitamin B, or calcitonin(3). Surgical treatment, if required, involves radical excision and reconstruction(3,5). REFERENCES 1. Feller L, Wood NH, Khammissa RAG, et al. The nature of fibrous dysplasia. Head Face Med. 2009;5:22. 2. Karligkiotis A, Terranova P, Dallan I, et al. Monostotic fibrous dysplasia of the inferior turbinate. Otolaryngol Head Neck Surg. 2012;146:1035–6. 3. Chen YR, Chang CN, Tan YC. Craniofacial fibrous dysplasia: an update. Chang Gung Med J. 2006;29:543–9. 4. Riddle ND, Bui MM. Fibrous dysplasia. Arch Pathol Lab Med. 2013; 137:134–8. 5. Gui H, Zhang S, Shen SG, et al. Real-time image-guided recontouring in the management of craniofacial fibrous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:680–5. 1. Canakkale Onsekiz Mart University, Faculty of Medicine, Canakkale, Turkey; https://orcid.org/0000-0002-2941-8879 2. Canakkale Onsekiz Mart University, Faculty of Medicine, Canakkale, Turkey; https://orcid.org/0000-0002-0606-6364 2. Canakkale Onsekiz Mart University, Faculty of Medicine, Canakkale, Turkey 3. Canakkale Onsekiz Mart University, Faculty of Medicine, Canakkale, Turkey; https://orcid.org/0000-0001-8737-2891 Correspondence: Mustafa Resorlu, MD Canakkale Onsekiz Mart University Terzioğlu Yerleşkesi, Barbaros Mh 17100, Canakkale, Turkey Email: mustafaresorlu77@gmail.com Received 2 October 2017. Accepted after revision 20 December 2017. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554