Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 5 - Sep. / Oct. of 2019
Vol. 52 nº 5 - Sep. / Oct. of 2019
|
LETTERS TO THE EDITOR
|
|
Hepatic changes after treatment with oxaliplatin |
|
|
Autho(rs): Leila Pereira Tenório1; Michelle Ferraz Oliveira Miranda2; Marcony Queiroz Andrade3; Marcelo Antônio Nobrega Araujo4 |
|
|
Dear Editor,
A 54-year-old female with colon cancer was treated surgically and with a chemotherapy regimen (fluorouracil, leucovorin, and oxaliplatin). Pre-treatment imaging examinations had shown that her liver had a normal aspect, with no evidence of focal lesions. Follow-up (post-treatment) examinations showed mild splenomegaly and slightly lobulated liver contours. Some liver nodules also appeared, most of them characterized by an isointense signal in T1- and T2-weighted sequences with enhancement in the arterial phase and persistent uptake in the hepatobiliary phase after intravenous injection of a hepatobiliary-specific contrast agent, suggesting focal nodular hyperplasia (FNH)-like lesions (Figure 1). 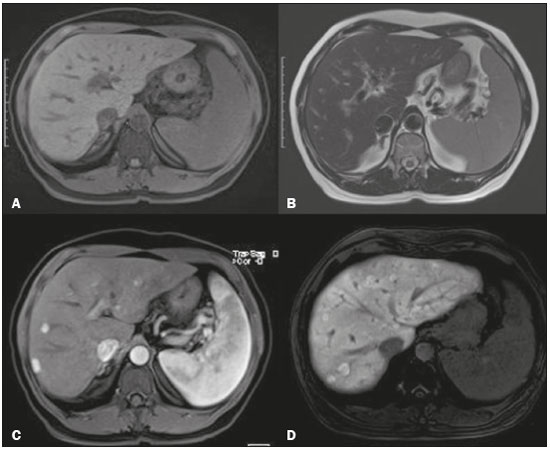 Figure 1. Magnetic resonance imaging. Unenhanced, fat-suppressed T1-weighted sequence (A), unenhanced T2-weighted sequence (B), and contrast-enhanced T1-weighted sequences in the arterial and hepatobiliary phases (C and D, respectively), showing mild splenomegaly and hepatic nodules with isointense signals on T1- and T2-weighted sequences, arterial enhancement, and persistent enhancement in the hepatobiliary phase, suggesting FNH-like lesions. Other areas containing nodules and showing contrast uptake in the hepatobiliary phase can be seen, also suggesting benignity. Colorectal carcinoma is the third leading cancer worldwide, and hepatic metastasis occurs in 40–50% of cases. Various chemotherapy regimens are used in order to treat this type of neoplasia, several of them including oxaliplatin(1). Various classes of chemotherapeutic agents have been associated with hepatic lesions such as steatosis, steatohepatitis, sinusoidal obstruction syndrome, acute hepatitis, and liver necrosis(2). Oxaliplatin-based treatments are most often associated with sinusoidal obstruction syndrome and regenerative nodular hyperplasia(2,3). Sinusoidal obstruction syndrome, previously known as hepatic veno-occlusive disease, is caused by deposits of fibrous material into the small branches of the hepatic veins, causing obstruction and sinusoidal dilatation, resulting in congestion, perisinusoidal fibrosis, and hepatocellular lesion. The condition can lead to hepatosplenomegaly and portal hypertension. Regenerative nodular hyperplasia typically manifests as relatively small lesions, diagnosed in pathological studies, although its pathogenesis has yet to be well established. It is believed to be related to intrahepatic vascular disorders that promote areas of hypoperfusion (atrophic areas) adjacent to areas of hyperperfusion (regenerative areas) and are regarded by some authors as a final stage of vascular lesion induced by chemotherapeutic agents(3,4). Macroscopic nodules with radiological and pathological characteristics identical to those of FNH-like lesions have been related to various hepatic conditions(5) such as cirrhosis(6), vascular changes such as Budd–Chiari syndrome(6), and, more recently, the use of oxaliplatin-based chemotherapy regimens(7,8), as in the case reported here. Focal hepatic lesions that appear in imaging examinations during the follow-up of cancer patients oblige us to make a careful analysis because of the possibility of a secondary neoplasm. Metastases of colon carcinomas are usually poorly vascularized and show low uptake in the hepatobiliary phase. Knowing the histological type of the primary neoplasm, as well as the radiological pattern of metastasis of chemotherapy-induced lesions, is essential for the correct diagnosis and appropriate clinical guidance in cases of hepatic changes after treatment with oxaliplatin. Understanding the hepatic changes related to chemotherapy, especially the possibility that FNH-like hypervascular lesions will occur after treatment with oxaliplatin, can facilitate the diagnosis of chemotherapy-induced lesions and prevent unnecessary invasive procedures in patient follow-up. REFERENCES 1. Fonseca GM, Herman P, Faraj SF, et al. Pathological factors and prognosis of resected liver metastases of colorectal carcinoma: implications and proposal for a pathological reporting protocol. Histopathology. 2018; 72:377–90. 2. Sharma A, Houshyar R, Bhosale P, et al. Chemotherapy induced liver abnormalities: an imaging perspective. Clin Mol Hepatol. 2014;20:317–26. 3. Rubbia-Brandt L, Audard V, Sartoretti P, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460–6. 4. Ames JT, Federle MP, Chopra K. Distinguishing clinical and imaging features of nodular regenerative hyperplasia and large regenerative nodules of the liver. Clin Radiol. 2009;64:1190–5. 5. Kim MJ, Rhee HJ, Jeong HT. Hyperintense lesions on gadoxetate disodium-enhanced hepatobiliary phase imaging. AJR Am J Roentgenol. 2012;199:W575–86. 6. Choi JY, Lee HC, Yim JH, et al. Focal nodular hyperplasia or focal nodular hyperplasia-like lesions of the liver: a special emphasis on diagnosis. J Gastroenterol Hepatol. 2011;26:1004–9. 7. Donadon M, Di Tommaso L, Roncalli M, et al. Multiple focal nodular hyperplasias induced by oxaliplatin-based chemotherapy. World J Hepatol. 2013;5:340–4. 8. Shlomai A, Tobar A, Benjaminov O. Multiple liver lesions after oxaliplatin-based chemotherapy for colorectal cancer. Gastroenterology. 2015; 149:e1–3. 1. Hospital Geral Roberto Santos, Salvador, BA, Brasil; https://orcid.org/0000-0003-2006-0265 2. Hospital Geral Roberto Santos, Salvador, BA, Brasil; https://orcid.org/0000-0002-7073-4697 3. Hospital Aliança, Salvador, BA, Brasil; https://orcid.org/0000-0002-2136-5688 4. Hospital Geral Roberto Santos, Salvador, BA, Brasil; https://orcid.org/0000-0002-4929-5845 Correspondência: Dra. Leila Pereira Tenório Hospital Geral Roberto Santos – Radiologia Rua Direta do Saboeiro, s/nº, Cabula Salvador, BA, Brazil, 41180-780 E-mail: leilatenorio@hotmail.com Received 27 September 2017. Accepted after revision 12 December 2017. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554