Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 6 - Nov. / Dec. of 2019
Vol. 52 nº 6 - Nov. / Dec. of 2019
|
ORIGINAL ARTICLE
|
|
Rates of success and failure of biopsies of hollow abdominal organs: descriptive analysis |
|
|
Autho(rs): Diana Oliveira1,a; Cristina Felicani2,b; Carla Serra2,c |
|
|
Keywords: Biopsy, needle/methods; Abdominal neoplasms/pathology; Ultrasonography, interventional/methods; Contrast media/ administration & dosage. |
|
|
Abstract: Ultrasound-guided percutaneous biopsy was a great innovation in the field of medicine. It made biopsies faster, saving the patient from radiation exposure and from invasive procedures with greater risks(1). Currently, ultrasound is the most useful imaging technique for guiding percutaneous and endoscopic biopsies(2), being extensively used in daily clinical practice because it retrieves sufficient high-quality tissue to facilitate the pathologic diagnosis of focal and diffuse diseases(3). In most cases of abdominal or pelvic lesions, is possible to use ultrasound guidance. It is often safer, quicker, and less expensive, as well as having a higher diagnostic yield, in comparison with other image guidance modalities, including computed tomography (CT). In general, if the mass or target lesion can be seen with ultrasound, a biopsy will be performed under ultrasound rather than CT(1). Contrast-enhanced ultrasound (CEUS) is the latest paradigm in this area. It improves the detection and characterization of multiple lesions(4,5), as well as increasing the accuracy of percutaneous biopsies(6,7) and reducing the rate of complications(6,8–11). Through the use of CEUS, it is possible to perform real-time evaluation of the perfusion of focal lesions in the arterial, portal, and delayed contrast phases, in order to characterize focal lesions with high diagnostic accuracy(5–7,12). In comparison with conventional ultrasound-guided biopsy, CEUS-guided biopsy has been shown to increase diagnostic accuracy by 5% (from 93.3% to 98.3%) and to decrease the false-negative rate in those large undetermined abdominal lesions(6).
The aim of this article is to evaluate the rates of success and failure of ultrasound-guided percutaneous biopsy of abdominal lesions in hollow organs. We also analyze the histopathological results and the influence of the use of CEUS. MATERIALS AND METHODS This was a retrospective, descriptive, single-center study involving patients who underwent ultrasound-guided percutaneous core needle biopsy of lesions in the abdominal cavity, excluding lesions in solid organs (liver, spleen, kidney, or reproductive system), in the diagnostic and interventional ultrasound department of a tertiary care hospital between January 2017 and June 2018. Patients were identified through a review of medical records. The study was approved by the local research ethics committee before the collection of data. We employed a standardized data collection form, including clinical and demographic characteristics of the patients, clinical suspicion, and pathological findings. Patients for whom the procedure documentation was incomplete were excluded. Statistical analysis Categorical variables are expressed as absolute and relative frequencies, whereas continuous variables are expressed as means and standard deviations. All statistical analyses were performed with the SPSS Statistics software package, version 23.0 (IBM Corp., Armonk, NY, USA). RESULTS A total of 838 ultrasound-guided biopsies were performed between January of 2017 and June of 2018. Of those, 49 (6%) were abdominal biopsies of hollow organs, performed in 48 patients (1 patient underwent two procedures), of whom 26 (54%) were women and 22 (46%) were men. The mean age was 64 ± 15.4 years (range, 18–88 years). All 49 procedures were analyzed. Of the 48 patients included, 18 (38%) had a history of cancer, the most common type being hematologic neoplasms, which accounted for 7 cases (39%), followed by gynecological neoplasms, in 6 cases (33%), and colorectal cancer, in 3 (17%). Four patients (8%) had previously been diagnosed with more than one type of cancer. Of the 49 biopsies evaluated, 24 (49%) were performed in cases of lymphadenopathy, 20 (41%) were performed in cases of unspecified abdominal masses, and 2 (4%) were performed for peritoneal sampling. The three remaining biopsies (6%) were obtained from the mesentery, a thickened area of the perirenal fascia, and a thickened area of the intestinal wall, respectively. The mean lesion size was 3.5 ± 2.4 cm (range, 0.8–14.0 cm). As can be seen in Table 1, the lesion diameter was between 2 cm and 5 cm in 32 (65%) of the cases, whereas it was less than 2 cm in only 10 (21%). 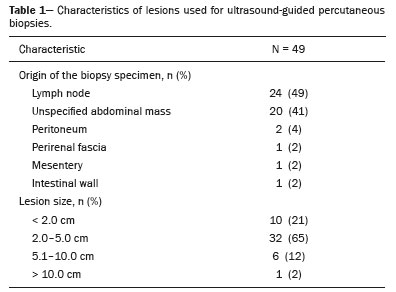 In 18 cases (37%), there was no diagnostic hypothesis and CEUS was therefore performed prior to the biopsy. The contrast behavior was suggestive of malignancy in 11 samples (61%) and was inconclusive in 7 (39%). Among the latter lesions, the histopathology showed that five (71%) were malignant and two (29%) were benign. Malignancy was suspected in 44 cases (90%). Among those 44 cases, the suspicion was of a new neoplasm in 28 (64%), of relapse in 11 (25%), and of a metastatic lesion in 5 (11%). The biopsy specimen was sufficient for diagnosis in 44 (90%) of the 49 procedures analyzed and was insufficient in 5 (Table 2). In those five cases, surgical biopsy was recommended. The histopathology revealed malignant lesions in 33 (67%) of the biopsies and benign lesions in 11 (23%). Of the 33 malignant lesions, 7 (21%) were primary, 15 (46%) were metastatic, and 11 (33%) were representative of recurrence, as depicted in Table 2. The diagnosis was consistent with the clinical suspicion in 33 cases (75%). 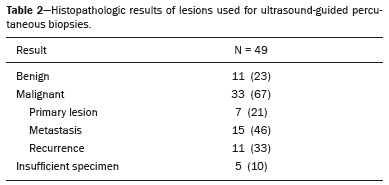 Of the 18 lesions that were evaluated with CEUS (Table 3), all were suspected of malignancy on ultrasound, histological confirmation of malignancy being obtained in 16 (89%). Of the remaining 31 lesions, 26 (84%) were suspected of being malignant, and histological confirmation was obtained in 22 (85%) of those. Patients were followed for a period of two weeks, during which time no complications were reported. 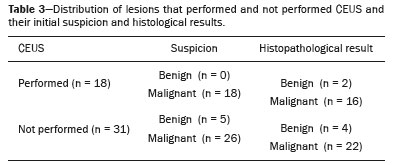 DISCUSSION Abdominal masses include various benign and malignant pathological lesions. Such lesions can be solid or cystic and which can differ depending on patient age and gender, as well as on their location and organ or tissue of origin(13). The results of the present study demonstrate that ultrasound-guided percutaneous biopsy of lesions in hollow abdominal organs is an effective procedure with an accuracy of nearly 90%. The great majority of the samples were obtained from patients with lymphadenopathy or unspecified abdominal masses, although some were obtained from the intestinal wall and peritoneum. Suspicion of a new neoplasm was the main reason for performing biopsy among the patients evaluated in our study. The use of CEUS plays an important role in the evaluation of suspicious lesions because it helps physicians determine whether a biopsy is necessary, identify the most viable area within the lesion, and choose the best lesion to biopsy(6). The diagnostic performance of CEUS has been shown to be better than that of conventional ultrasound(4,6,7,12). However, in our study, there were no records of lesions excluded for biopsy after CEUS had been performed, which could account for the fact that there was no significant difference between the CEUS and non-CEUS groups in terms of diagnostic performance (89% versus 85%). In the sample as a whole, the diagnosis was consistent with the clinical suspicion in the vast majority of cases. In our experience, ultrasound-guided percutaneous biopsy is a safe procedure, and there were no reported complications in the present study. Ultrasound has a number of advantages(1): real-time imaging guidance; speed of use; the ability to compress the abdomen, thus increasing the proximity to the target; lower cost in comparison with CT and magnetic resonance imaging; rapid confirmation of complications; higher success rates; portability; and the fact that it does not expose the patient and medical staff to radiation. In comparison with contrast-enhanced CT and contrast-enhanced magnetic resonance imaging, CEUS has the advantage of exerting no harmful effects on the kidneys or thyroid(4,14). This study has some limitations. The retrospective design introduces the possibility of certain biases. For example, we were able to evaluate only those patients for whom the necessary information was available in the medical report. CONCLUSION Ultrasound-guided percutaneous biopsy is a safe, efficient, minimally invasive, accurate method of diagnosing undetermined lesions in hollow abdominal organs. The present study demonstrated that the most common indication for ultrasound-guided percutaneous biopsy was the suspicion of a new neoplasm, in which performing CEUS might be helpful. It was possible to obtain a good specimen for histopathological evaluation in over 90% of the cases, and the result of the biopsy was in agreement with the clinical suspicion in 75%. REFERENCES 1. Winter TC, Lee FT Jr, Hinshaw JL. Ultrasound-guided biopsies in the abdomen and pelvis. Ultrasound Q. 2008;24:45–68. 2. Khati NJ, Gorodenker J, Hill MC. Ultrasound-guided biopsies of the abdomen. Ultrasound Q. 2011;27:255–68. 3. Kim JW, Shin SS. Ultrasound-guided percutaneous core needle biopsy of abdominal viscera: tips to ensure safe and effective biopsy. Korean J Radiol. 2017;18:309–22. 4. Chung YE, Kim KW. Contrast-enhanced ultrasonography: advance and current status in abdominal imaging. Ultrasonography. 2015;34:3–18. 5. Larsen LPS. Role of contrast enhanced ultrasonography in the assessment of hepatic metastases: a review. World J Hepatol. 2010; 27;2:8–15. 6. Mao F, Dong Y, Ji Z, et al. Contrast-enhanced ultrasound guided biopsy of undetermined abdominal lesions: a multidisciplinary decision- making approach. Biomed Res Int. 2017;2017:8791259. 7. Sparchez Z, Radu P, Zaharia T, et al. Usefulness of contrast enhanced ultrasound guidance in percutaneous biopsies of liver tumors. J Gastrointestin Liver Dis. 2011;20:191–6. 8. Lorentzen T, Nolsøe CP, Ewertsen C, et al. EFSUMB guidelines on interventional ultrasound (INVUS), part I. General aspects (long version). Ultraschall Med. 2015;36:E1-14. 9. Sidhu PS, Brabrand K, Cantisani V, et al. EFSUMB guidelines on interventional ultrasound (INVUS), part II. Diagnostic ultrasoundguided interventional procedures (long version). Ultraschall Med. 2015;36:E15–35. 10. Dietrich CF, Lorentzen T, Appelbaum L, et al. EFSUMB guidelines on interventional ultrasound (INVUS), part III – abdominal treatment procedures (long version). Ultraschall Med. 2016;37:E1–E32. 11. Dietrich CF, Lorentzen T, Appelbaum L, et al. EFSUMB guidelines on interventional ultrasound (INVUS), part III – abdominal treatment procedures (short version). Ultraschall Med. 2016;37:27–45. 12. Dong Y, Mao F, Wang WP, et al. Value of contrast-enhanced ultrasound in guidance of percutaneous biopsy in peripheral pulmonary lesions. Biomed Res Int. 2015;2015:531507. 13. Akkoca M, Tokgöz S, Yılmaz KB, et al. Diagnosis and treatment approaches for intraabdominal masses in adults. Journal of Ankara University Faculty of Medicine. 2017;70:201–5. 14. Sidhu PS, Choi BI, Nielsen MB. The EFSUMB guidelines on the non-hepatic clinical applications of contrast enhanced ultrasound (CEUS): a new dawn for the escalating use of this ubiquitous technique. Ultraschall Med. 2012;33:5–7. 1. Coimbra University Hospital, Coimbra, Portugal 2. Interventional Ultrasound Unit, St. Orsola-Malpighi Hospital, Bologna, Italy a. https://orcid.org/0000-0002-1466-3855 b. https://orcid.org/0000-0002-3842-4701 c. https://orcid.org/0000-0001-5555-0745 Correspondence: Diana Oliveira, MD Avenida Bissaya Barreto – Praceta Prof. Mota Pinto Coimbra 3000-075, Portugal Email: difilipa_oliveira@ hotmail.com Received 25 March 2019 Accepted after revision 10 June 2019 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554