Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 50 nº 2 - Mar. / Apr. of 2017
Vol. 50 nº 2 - Mar. / Apr. of 2017
|
LETTER TO THE EDITOR
|
|
Subcapsular splenic hematoma and spontaneous hemoperitoneum in a cocaine user |
|
|
Autho(rs): Bruno Niemeyer de Freitas Ribeiro1; Rafael Santos Correia1; Tiago Medina Salata2; Fernanda Salata Antunes2; Edson Marchiori3 |
|
|
Dear Editor,
A 23-year-old male patient presented with a 36-h history of intense, sudden, progressive abdominal pain, predominantly in the left hypochondrium, irradiating to the ipsilateral infrascapular region. He reported no previous trauma, fever, headache, fatigue, myalgia, arthralgia, skin alterations, or comorbidities. During the clinical interview, he reported moderate smoking and the routine use of an illicit drug (cocaine), including hours prior to the onset of pain. On physical examination, he was well-oriented, hemodynamically stable, and afebrile. The serology was negative for hepatitis B, hepatitis C, and dengue, and the results were normal for antineutrophil cytoplasmic antibody, antinuclear factor, the venereal disease research laboratory test, urea, creatinine, erythrocyte sedimentation rate, C-reactive protein, and coagulation profile. Hemoglobin electrophoresis showed no alterations. Computed tomography (CT) showed a dense collection, compatible with hematic material, in close proximity to the spleen, as well as showing hemoperitoneum (Figure 1). Arteriography showed no abnormalities. Exploratory laparotomy revealed subcapsular splenic hematoma and confirmed the hemoperitoneum, with no evidence of a lesion within the cavity. 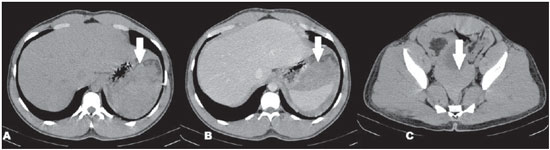 Figure 1. CT scan showing subcapsular hematoma and hemoperitoneum. A: CT, axial slice, without contrast, demonstrating dense collections (arrow) adjacent to the spleen. B: Contrast-enhanced axial CT, showing the dense collections adjacent to the spleen (arrow), without contrast enhancement, indicative of subcapsular hematoma. C: CT, axial slice, without contrast, demonstrating spontaneously dense free liquid in the pelvis (arrow), indicative of hemoperitoneum. Given that there was no perisplenic trauma or adhesions suggestive of previous trauma and that the macroscopic aspect of the spleen was normal on the CT scan and in the exploratory laparotomy, together with the facts that diseases affecting the splenic parenchyma were ruled out and that the patient had used cocaine immediately prior to the episode, we established the working diagnosis of nontraumatic splenic hemorrhage secondary to cocaine use. During clinical follow-up, the patient progressed well, without complications. Recent studies in the radiology literature of Brazil have emphasized the importance of CT and magnetic resonance imaging scans to improving the diagnosis in nontraumatic abdominal disorders(1–5). Splenic hemorrhages are rarely encountered without prior trauma and can have fatal consequences, which makes their early diagnosis essential. The main nontraumatic conditions include neoplasms, as well as inflammatory/infectious, iatrogenic, and mechanical processes(6). The clinical signs of nontraumatic splenic hemorrhage are similar to those found in cases resulting from trauma, including pain in the upper left quadrant, with or without irradiation to the left shoulder, caused by diaphragmatic irritation, evolving to hemodynamic instability in the most severe cases. Such manifestations are nonspecific and cannot be characterized solely by physical examination. Therefore, in hemodynamically stable patients, CT evaluation is fundamental to the characterization of the affected organs(6,7). Currently, Brazil is the second largest consumer of cocaine and its derivatives, the leader being the United States(8). The mechanism thought to trigger bleeding during or after cocaine use is stimulation of alpha-adrenergic receptors, which produce vasoconstriction with a consequent increase in abdominal blood pressure and a reduction of up to 20% of the splenic volume, promoting high-pressure blood flow in a retracted parenchyma and with a low concentration of connective tissue, making the spleen more prone to bleeding, which can be triggered even by coughing(6,9). In nontraumatic splenic hemorrhage, the differential diagnoses include dengue, infectious mononucleosis, polyarteritis nodosa, segmental arterial mediolysis, neoplasms, coagulopathy. and hemoglobinopathy(6,7,9–11). In conclusion, although nontraumatic splenic hemorrhage is uncommon, the possibility of cocaine use as a triggering event should be considered, especially in young, previously healthy patients with no comorbidities to explain such an event. REFERENCES 1. Rocha EL, Pedrassa BC, Bormann RL, et al. Abdominal tuberculosis: a radiological review with emphasis on computed tomography and magnetic resonance imaging findings. Radiol Bras. 2015;48:181–91. 2. Barros RHO, Penachim TJ, Martins DL, et al. Multidetector computed tomography in the preoperative staging of gastric adenocarcinoma. Radiol Bras. 2015;48:74–80. 3. Bormann RL, Rocha EL, Kierzenbaum ML, et al. The role of gadoxetic acid as a paramagnetic contrast medium in the characterization and detection of focal liver lesions: a review. Radiol Bras. 2015;48:43–51. 4. Fernandes DA, Kido RYZ, Barros RHO, et al. Immunoglobulin G4-related disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiol Bras. 2016;49:122–5. 5. Fajardo L, Ramin GA, Penachim TJ, et al. Abdominal manifestations of extranodal lymphoma: pictorial essay. Radiol Bras. 2016;49:397–402. 6. Azar F, Brownson E, Dechert T. Cocaine-associated hemoperitoneum following atraumatic splenic rupture: a case report and literature review. World J Emerg Surg. 2013;8:33. 7. Lin WY, Lin GM, Chang FY. An unusual presentation of scrub typhus with atraumatic hemoperitoneum. Am J Gastroenterol. 2009;104:1067. 8. Laranjeira R, Madruga CS, Pinsky I, et al. II Levantamento Nacional de Álcool e Drogas (LENAD) – 2012. São Paulo: Instituto Nacional de Ciência e Tecnologia para Políticas Públicas de Álcool e Outras Drogas (INPAD), Unifesp; 2014. 9. Carlin F, Walker AB, Pappachan JM. Spontaneous splenic rupture in an intravenous drug abuser. Am J Med. 2014;127:e7–8. 10. Mukhopadhyay M, Chatterjee N, Maity P, et al. Spontaneous splenic rupture: a rare presentation of dengue fever. Indian J Crit Care Med. 2014;18:110–2. 11. Michael M, Widmer U, Wildermuth S, et al. Segmental arterial mediolysis: CTA findings at presentation and follow-up. AJR Am J Roentgenol. 2006;187:1463–9. 12. Redondo MC, Ríos A, Cohen R, et al. Hemorrhagic dengue with spontaneous splenic rupture: case report and review. Clin Infect Dis. 1997; 25:1262–3. 1. Instituto Estadual do Cérebro Paulo Niemeyer, Rio de Janeiro, RJ, Brazil 2. Hospital Casa de Portugal / Clínica 3D Diagnóstico por Imagem, Rio de Janeiro, RJ, Brazil 3. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Mailing address: Instituto Estadual do Cérebro Paulo Niemeyer – Departamento de Radiologia Rua do Rezende, 156, Centro Rio de Janeiro, RJ, Brazil, 20231-092 E-mail: bruno.niemeyer@hotmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554