Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 1 - Jan. /Feb. of 2015
Vol. 48 nº 1 - Jan. /Feb. of 2015
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Alexandre Dias Mançano1; Cássia Carvalho de Siqueira2; Gustavo Gomides Macedo2 |
|
|
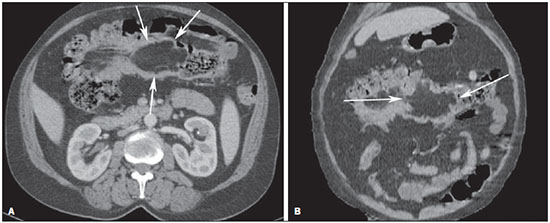
A female, 59 year-old patient complaining of colic-like abdominal pain and mild enterorrhagia for some months. No abnormal finding was observed at physical examination and laboratory tests. Colonoscopy demonstrated the presence of an expansile occlusive luminal lesion in the ascending
colon. The patient was referred for radiological staging and submitted to contrast-enhanced abdominal computed tomography (Figure 1). Image description Figure 1. Axial CT section (A) and coronal reformation (B) showing a predominantly lipomatous tumor with fat density in the transverse colon (arrows), with bosselated contour, measuring about 9 cm in its greater cross-sectional diameter, and signs of ileocolic intussusception. Diagnosis: Giant colonic lipoma. COMMENTS The Brazilian radiological literature has recently highlighted the relevance of imaging methods in the improvement of the diagnosis of digestive system conditions(1-12). Colonic lipoma is a rare benign tumor in spite of being the most common non-epithelial (mesenchymal) neoplasia in the gastrointestinal tract. Generally, it is located in the submucosa and, in rare cases, in the subserous membrane(13) and may have a lobulated aspect. This tumor is more commonly found in women (66,7%)(14) between the fifth and sixth decades of life, and is asymptomatic in most cases. However, a tumor > 2-3 cm may generate normally nonspecific and long-lasting symptoms such as abdominal pain, blood in stools and change in bowel habits(13). Larger tumors may present symptoms of bowel obstruction with colonic intussusception(14). Spontaneous elimination of lipomas has also been reported(15). Studies demonstrate that approximately 46% of bowel lipomas are incidentally found in surgical specimens removed for other conditions(13,16), and the ascending colon is the most common site of involvement(13). Imaging studies can be useful in the preoperative diagnosis, but generally the definitive diagnosis is made with basis on the analysis of the surgical specimen(13) (Figure 2). However, the finding of macroscopic fat at computed tomography or magnetic resonance imaging narrows the differential diagnosis in these cases(17). 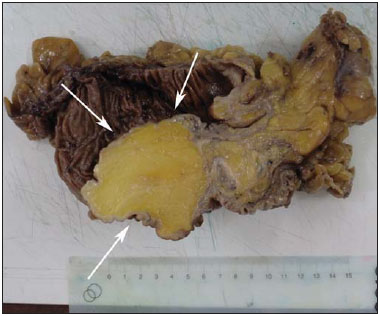 Figure 2. Surgical specimen showing a lipomatous tumor in the transverse colon (arrows). Barium enema demonstrates luminal filling failure, but such finding is nonspecific and may be observed in other types of colonic neoplasias(14). Unenhanced nodules or parietal mass with fat density (-40 to -120 Hounsfield units), as described in the present case, represent a useful tomographic finding in the diagnosis. In cases of association with intussusception, the diagnosis may be more difficult because of the presence of necrotic foci or infarct(18) and, in many cases, the differential diagnosis with other lesions such as adenocarcinomas, lymphomas and metastases(13,19,20) cannot be reliably be established. The treatment varies with the location, symptoms and size of the lipoma. Lesions < 2 cm may be endoscopically resected with the aid of ultrasonography in order to reduce the risk of perforation. The great majority of authors recommend surgical treatment for lesions > 2 cm, and the surgical options include lesion resection, partial colectomy and hemicolectomy(21). Main differential diagnoses include adenoma, adenocarcinoma, lymphoma, neuroendocrine tumors, fibroma, leiomyoma and hamartoma(13,14,18,22,23). Although rare, colonic lipomas should be considered in the differential diagnosis of large bowel tumors. An accurate diagnosis is hardly made preoperatively and many times the lesion may be confused with adenomatous polyps or carcinoma. The surgical approach is the treatment of choice for colonic lipoma, varying with the lesion size and location, and with the presence or not of complications(18). REFERENCES 1. Kierszenbaum ML, von Atzingen AC, Tiferes DA, et al. Colonografia por tomografia computadorizada na visão do médico encaminhador: qual o seu valor segundo a visão de especialistas? Radiol Bras. 2014;47:135-40. 2. Francisco FAF, Araújo ALE, Oliveira Neto JA, et al. Contraste hepatobiliar: diagnóstico diferencial das lesões hepáticas focais, armadilhas e outras indicações. Radiol Bras. 2014;47:301-9. 3. Torres LR, Timbó LS, Ribeiro CMF, et al. Hemangioendotelioma hepático multifocal e metastático: relato de caso e revisão da literatura. Radiol Bras. 2014;47:194-6. 4. Terceiro MG, Faria IM, Alfenas R, et al. Hérnia de Amyand com apendicite perfurada. Radiol Bras. 2014;47(6):xi-xiii. 5. Cunha EFC, Rocha MS, Pereira FP, et al. Necrose pancreática delimitada e outros conceitos atuais na avaliação radiológica da pancreatite aguda. Radiol Bras. 2014;47:165-75. 6. Kadow JS, Fingerhut CJP, Fernandes VB, et al. Peritonite encapsulante: tomografia computadorizada e correlação cirúrgica. Radiol Bras. 2014;47:262-4. 7. Santana Júnior PJ, Aurione ACV, Dangoni R, et al. Tumor neuroendócrino gástrico tipo III. Radiol Bras. 2014;47(4):xi-xii. 8. Pedrassa, BC, Rocha EL, Kierszenbaum ML, et al. Tumores hepáticos incomuns: ensaio iconográfico - Parte 1. Radiol Bras. 2014;47:310-6. 9. Pedrassa, BC, Rocha EL, Kierszenbaum ML, et al. Tumores hepáticos incomuns: ensaio iconográfico - Parte 2. Radiol Bras. 2014;47:374-9. 10. Martins FP, Vilela EG, Ferrari MLA, et al Contribuição da medida do volume de fluxo da artéria mesentérica superior pelo Doppler na caracterização da atividade inflamatória em pacientes com doença de Crohn. Radiol Bras. 2013;46:279-83. 11. Teixeira ACV, Torres US, Westin CEG, et al. Tomografia computadorizada com multidetectores no diagnóstico pré-operatório das complicações intestinais causadas pela ingestão de corpos estranhos da dieta sem suspeita clínica: série de casos enfatizando o uso de técnicas de renderização volumétrica. Radiol Bras. 2013;46:346-50. 12. Costa DMC, Salvadori PS, Monjardim RF, et al. Quando a fase sem contraste intravenoso é desnecessária nos exames de tomografia computadorizada do abdome? Análise retrospectiva de 244 casos. Radiol Bras. 2013;46:197-202. 13. Ghidirim G, Mishin I, Gutsu E, et al. Giant submucosal lipoma of the cecum: report of a case and review of literature. Rom J Gastroenterol. 2005;14:393-6. 14. Jiang L, Jiang LS, Li FY, et al. Giant submucosal lipoma located in the descending colon: a case report and review of the literature. World J Gastroenterol. 2007;13:5664-7. 15. Ryan J, Martin JE, Pollock DJ. Fatty tumours of the large intestine: a clinicopathological review of 13 cases. Br J Surg. 1989;76:793-6. 16. Taylor BA, Wolff BG. Colonic lipomas. Report of two unusual cases and review of the Mayo Clinic experience, 1976-1985. Dis Colon Rectum. 1987;30:888-93. 17. Pereira JM, Sirlin CB, Pinto PS, et al. CT and MR imaging of extra-hepatic fatty masses of the abdomen and pelvis: techniques, diagnosis, differential diagnosis, and pitfalls. Radiographics. 2005;25:69-85. 18. Atmatzidis S, Chatzimavroudis G, Patsas A, et al. Pedunculated cecal lipoma causing colo-colonic intussusception: a rare case report. Case Rep Surg. 2012;2012:279213. 19.Michowitz M, Lazebnik N, Noy S, et al. Lipoma of the colon. A report of 22 cases. Am Surg. 1985;51:449-54. 20. Rogy MA, Mirza D, Berlakovich G, et al. Submucous large-bowel lipomas - presentation and management. An 18-year study. Eur J Surg. 1991;157:51-5. 21. Paškauskas S, Latkauskas T, Valeikaitģ G, et al. Colonic intussusception caused by colonic lipoma: a case report. Medicina (Kaunas). 2010;46:477-81. 22. Gürses B, Kabakci N, Akyuz U, et al. Imaging features of a cecal lipoma as a lead point for colo-colonic intussusception. Emerg Radiol. 2008;15:133-6. 23. Notaro JR, Masser PA. Annular colon lipoma: a case report and review of the literature. Surgery. 1991;110:570-2. 1. MD, Radiologist at Radiologia Anchieta – Hospital Anchieta, Coordinator for Medical Residency at Hospital Regional de Taguatinga, Taguatinga, DF, Brazil 2. MDs., Residents at Hospital Regional de Taguatinga, Taguatinga, DF, Brazil Mailing Address: Dr. Alexandre Dias Mançano Centro Médico Hospitalar Anchieta AE 8/10 Setor C Norte, 1º subsolo, Centro de Excelência Anchieta, lojas 12 e 13 Taguatinga, DF, Brazil, 72115-700 E-mail: alex.manzano1@gmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554