Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 1 - Jan. /Feb. of 2015
Vol. 48 nº 1 - Jan. /Feb. of 2015
|
LETTER TO THE EDITOR
|
|
Peripheral primitive neuroectodermal tumor of chest wall in young adult |
|
|
Autho(rs): Gilmar Moreira Silva Junior1; Gláucia Maria Ribeiro Zanetti2; Jorge Luiz Barillo3; Edson Marchiori2 |
|
|
Dear Editor,
A 27-year old man attended the health unit complaining of thoracolumbar pain radiating to the anterior region of his right hemithorax. Computed tomography (CT) identified the presence of a spindle-shaped mass on the anterolateral wall of the right hemithorax, with an osteolytic lesion in the costal arch. No sign of distant metastasis was found. Percutaneous biopsy, histopathological and immunohistochemical analyses were performed, with diagnosis of primary neuroectodermal tumor (PNET). Within one month, a remarkable growth of the lesion was observed, with local dissemination to the pleura and onset of distant metastasis, particularly in the axial skeleton, affecting several bone elements. Neoadjuvant chemotherapy was initiated and 50% reduction in tumor volume was demonstrated at magnetic resonance imaging (MRI). Wide surgical resection was performed with placement of a Marlex mesh for the chest wall reconstruction. Adjuvant chemotherapy was reinitiated after the surgery. Eight months after the disease onset, the clinical condition presented unfavorable progression with onset of innumerable metastatic pleural lesions and progressive lower limbs paresthesia and paresis. Also, the onset of new bone metastases invading thoracolumbar and sacral vertebral bodies was observed, with paraplegia resulting from rachidian canal invasion. The patient was admitted with cachexia, dyspnea while talking and difficult-to-control chest pain, and progressed to death. Chest imaging evaluation has been the subject of a series of recent publications in the Brazilian radiological literature(1-7). Peripheral PNETs are extremely malignant tumors and bones and soft tissues are their primary sites. Most frequently, such tumors affect the chest wall, paravertebral region, pelvis and limbs, and also are described in a range of organs such as kidneys, urinary bladder and heart(8). PNET of the chest wall may affect the ribs, sternum, scapula, clavicle and soft tissues of the chest wall and pleura(9). Frequently, these tumors affect children and adolescents, with incidence peak between 15 and 25 years. About 80% of patients are under the age of 20 at the moment of the diagnosis(10). The common presentation of chest wall PNETs is chest pain followed by increase in local volume and/or mass sensitive to palpation, and dyspnea. Pleural effusion is observed in cases where such tumors affect the pleura. Distant metastases occur in lungs, bones, bone marrow, liver and brain(11). The PNET prognosis is related with adjacent structures invasion. About 30% of patients present with metastasis at the moment of the diagnosis(12). CT findings include ill-defined heterogeneous mass, sometimes with a necrotic center. Generally, calcifications are not observed(10). At MRI, a PNET may present as a hyperintense homogeneous lesion as compared with muscle tissues on T1- and T2-weighted sequences(12). There is no pathognomonic finding capable of differentiating PNET from other chest-wall neoplasms. The treatment includes complete and wide surgical resection, preoperative neoadjuvant and postoperative adjuvant chemotherapy, either with or without radiotherapy. Finally, PNET should be included in the differential diagnosis of chest wall tumors, particularly in children and adolescents, although isolated cases have been described in patients of all ages. 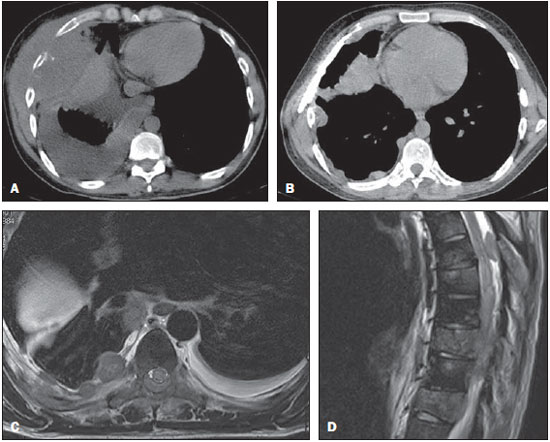 Figure 1. Axial CT section (A) demonstrating the presence of a spindle-shaped mass on the anterolateral wall of the right hemithorax, with an osteolytic lesion in costal arch, invading muscle and fat planes, with homolateral pleural effusion. CT images acquired eight months after the disease onset (B) showing innumerable pleural, nodular lesions compatible with metastases. Also, observe the Marlex mesh placed on the right chest wall. Chest MRI, axial T2-weighted image (C), without fat suppression, demonstrating pleural thickening and nodular lesions with involvement of the posterior thoracic wall at right. Dorsal spine MRI, sagittal T2-weighted turbo spin-echo image (D) without fat suppression identifying several sparse hyperintense ovoid lesions throughout vertebral bodies in the posterior epidural space at the D6 level. The findings are compatible with metastatic lesions. REFERENCES 1. Amorim VB, Rodrigues RS, Barreto MM, et al. Computed tomography findings in patients with H1N1 influenza A infection. Radiol Bras. 2013;46:299-306. 2. Zanetti G, Nobre LF, Mançano AD, et al. Nodular reversed halo sign caused by pulmonary tuberculosis, confirmed by sputum culture. Radiol Bras. 2013;46(6):ix-x. 3. Amoedo MK, Souza LVS, Souza AS, et al. Pulmonary interstitial emphysema: a case report and review of the literature. Radiol Bras. 2013;46:317-9. 4. Koenigkam Santos M, Barreto ARF, Chagas Neto FA, et al. Neuroendocrine tumors of the lung: major radiologic findings in a series of 22 histopathologically confirmed cases. Radiol Bras. 2012;45:191-7. 5. Zanetti G, Nobre LF, Mançano AD, et al. Paracoccidioidomicose pulmonar. Radiol Bras. 2014;47(1):xi-xiii. 6. Fernandes MC, Zanetti G, Hochhegger B, et al. Pneumonia por Rhodococcus equi em paciente com SIDA. Radiol Bras. 2014;47(3):xi-xiii. 7. Koenigkam-Santos M, Paula WD, Gompelmann D, et al. Endobronchial valves in severe emphysematous patients: CT evaluation of lung fissures completeness, treatment radiological response and quantitative emphysema analysis. Radiol Bras. 2013;46:15-22. 8. Hochhegger B, Felicetti JC, Marchiori E. An uncommon intrafissural mass: pleural primitive neuroectodermal tumor. Arch Bronconeumol. 2014 Mar 27. doi: 10.1016/j.arbres.2014.01.003. (Epub ahead of print]. 9. Pandit S, Mukherjee S, Bhattacharya S, et al. A rare mediastinal tumour in a young male mimicking massive pleural effusion. Lung India. 2012;29:66-9. 10. Biswas B, Agarwal AS, Shukla NK, et al. Evaluation of outcome and prognostic factors in thoracic primitive neuroectodermal tumor: a study of 84 cases. Ann Thorac Surg. 2013;96:2006-14. 11. Parikh M, Samujh R, Kanojia RP, et al. Peripheral primitive neuroectodermal tumor of chest wall in childhood: clinico-pathological significance, management and literature review. Chang Gung Med J. 2011;34:213-7. 12. Shi L, Guo Z, Wu X. Primary pulmonary primitive neuroectodermal tumor metastasis to the pancreas: a rare case with seven-year follow-up. Diagn Pathol. 2013;8:51. 1. Lumic - Radiology, Petrópolis, RJ, Brasil 2. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil 3. Universidade Federal Fluminense (UFF), Niterói, RJ, Brasil Mailing Address: Dr. Edson Marchiori Rua Thomaz Cameron, 438, Valparaíso Petrópolis, RJ, Brazil, 25685-120 E-mail: edmarchiori@gmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554