Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Misael Gadelha Terceiro; Igor Murad Faria; Rafael Alfenas de Paula; Edson Marchiori |
|
|
A 72-year-old, female patient presented with abdominal pain in the right flank for two days. Physical examination revealed pain at palpation and painful decompression, particularly in the right lower quadrant of the abdomen. The patient was afebrile and did not report diarrhea or vomiting episodes. Blood count revealed leukocytosis (11,900 cel/mm3), and the patient was submitted to abdominal computed tomography (Figure 1).
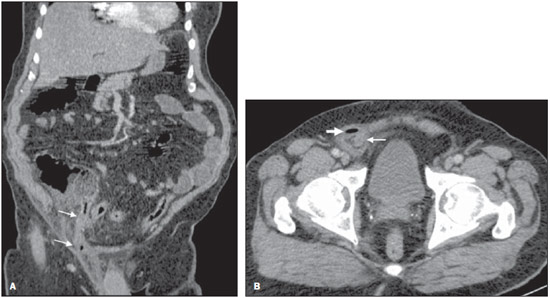 Figure 1. A: Abdominal computed tomography, coronal reconstruction. B: Axial section at the level of the pelvis. Image description Figure 1. A: Coronal reconstruction demonstrated the extension of the appendix into an inguinal hernia at right (arrows), with infiltration of adjacent fat planes. B: Axial section identified a distended appendix with thickened walls (thin arrow) within an inguinal hernia at right, with the presence of adjacent focus of free gas (gross arrow). Diagnosis: Amyand's hernia with perforated appendicitis. COMMENTS A series of recent publications in the Brazilian radiological literature have evaluated the role played by radiology in the study of the digestive tube and acute abdominal conditions(1–8). In the present case, a perforated appendix within the right inguinal canal was found during surgery. The patient underwent appendectomy with hernia repair and was discharged in four days. The term Amyand's hernia is used as a vermiform appendix is found within an inguinal hernia. The incidence of appendix within a hernial sac ranges between 0.28 and 1%(9), and in 0.13% it is inflamed(10). Amyand's hernia is more prevalent in male individuals and presents bimodal distribution as regards age range, affecting principally neonates and patients above the age of 70(11). In most cases, the appendix is within an indirect inguinal hernia located at right, reflecting the usual position of the vermiform appendix. Amyand's hernia is rarely found in the left inguinal region. The most common clinical presentation is similar to the clinical condition of incarcerated hernia and for this reason the diagnosis is made during surgery(11–15). In most of times, the patient presents with a painful mass in the inguinal region, possibly in association with vomiting. Fever and leukocytosis which are commonly found in cases of appendicitis are rarely observed(16,17). The use of computed tomography facilitates the identification of inguinal hernias, and sagittal and coronal reconstructions are particularly useful for the visualization of a blind-ending tubular structure arising from the cecum and entering the inguinal canal, representing the vermiform appendix within the hernial sac(16). In addition to the evaluation of signs of appendix perforation such as peritonitis and extension of the inflammatory process into the abdominal cavity, it is essential to evaluate signs of appendicitis such as appendix wall thickening and infiltration of adjacent fat planes(18,19). Additionally, the presence of other associated processes such as abdominal tumors and masses must be assessed. In the presence of such findings, Losanoff et al.(20,21) have classified Amyand's hernias into four types. According to such a classification, each type of Amyand's hernia requires a specific surgical approach. In the presence of Amyand's hernia with a normal appendix (type I hernia), the surgical treatment is elective, aiming at reducing the hernia, either with or without appendectomy. The presence of appendicitis with inflammatory signs located in the hernial sac (type II hernia), generally are treated by means of hernia repair and appendectomy, possibly by inguinal approach. Appendicitis with signs of perforation, as well as the presence of peritonitis and intra-abdominal extension of the inflammatory process (type III hernia) is approached by means of laparotomy. The association with other abdominal conditions, such as tumor or abdominal masses (type IV hernia), requires an appropriate individualized approach. Thus, the recognition of such situations is essential for an appropriate management of cases. Finally, Amyand's hernias are rarely found and commonly underdiagnosed. Computed tomography and reconstructions represent a highly useful tool for a correct diagnosis. The radiologist must recognize these situations, identifying the factors which change the classification and approach to these hernias. REFERENCES 1. Kierszenbaum ML, von Atzingen AC, Tiferes DA, et al. CT colonography: the value of this method in the view of specialists. Radiol Bras. 2014;47:135–40. 2. Maciel AC, Maciel LC. Computed tomography colonography: a well-known but poorly utilized screening method. Radiol Bras. 2014;47(3):v–vi. 3. Cunha EFC, Rocha MS, Pereira FP, et al. Walled-off pancreatic necrosis and other current concepts in the radiological assessment of acute pancreatitis. Radiol Bras. 2014;47:165–75. 4. Alvares BR, Stopiglia MCS, Mezzacappa MA. Presence of air in the hepatic portal system in association with umbilical venous catheter malposition. Radiol Bras. 2014;47:49–50. 5. Silva WLF, Indiani JMC, Martin MF, et al. Pyogenic liver abscess caused by a foreign body which perforated the small gastric curvature. [Which is your diagnosis?]. Radiol Bras. 2013;46(1):xv–xvi. 6. Rocha MS. Liver abscesses secondary to acute cholangitis. [Letter to the Editor]. Radiol Bras 2013;46(2):xi. 7. Hollanda ES, Torres US, Gual F, et al. Spontaneous perforation of gallbladder with intrahepatic biloma formation: sonographic signs and correlation with computed tomography. Radiol Bras. 2013;46:320–2. 8. Teixeira ACV, Torres US, Westin CEG, et al. Multidetector-row computed tomography in the preoperative diagnosis of intestinal complications caused by clinically unsuspected ingested dietary foreign bodies: a case series emphasizing the use of volume rendering techniques. Radiol Bras. 2013;46:346–50. 9. Keskin S, Simsek C, Keskin Z. The Amyand's hernia: a rare clinical entity diagnosed by computed tomography. Case Rep Radiol. 2013;2013:638270. 10. D'Alia C, Lo Schiavo MG, Tonante A, et al. Amyand's hernia: case report and review of the literature. Hernia. 2003;7:89–91. 11. Michalinos A, Moris D, Vernadakis S. Amyand's hernia: a review. Am J Surg. 2014;207:989–95. 12. Thomas WE, Vowles KD, Williamson RC. Appendicitis in external herniae. Ann R Coll Surg Engl. 1982;64:121–2. 13. Sharma H, Gupta A, Shekhawat NS, et al. Amyand's hernia: a report of 18 consecutive patients over a 15-year period. Hernia. 2007;11:31–5. 14. Carey LC. Acute appendicitis occurring in hernias: a report of 10 cases. Surgery. 1967;61:236–8. 15. Inan I, Myers PO, Hagen ME, et al. Amyand's hernia: 10 years' experience. Surgeon. 2009;7:198–202. 16. Constantine S. Computed tomography appearances of Amyand hernia. J Comput Assist Tomogr. 2009;33:359–62. 17. Luchs JS, Halpern D, Katz DS. Amyand's hernia: prospective CT diagnosis. J Comput Assist Tomogr. 2000;24:884–6. 18. Montandon Júnior ME, Montandon C, Fiori GR, et al. Acute appendicitis: computed tomography findings – an iconographic essay. Radiol Bras. 2007;40:193–9. 19. Freire Filho EO, Jesus PEM, D'Ippolito G, et al. When and why use unenhanced computed tomography in patients with acute abdomen. Radiol Bras. 2006;39:51–62. 20. Losanoff JE, Basson MD. Amyand hernia: what lies beneath – a proposed classification scheme to determine management. Am Surg. 2007;73:1288–90. 21. Losanoff JE, Basson MD. Amyand hernia: a classification to improve management. Hernia. 2008;12:325–6. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil Mailing Address: Dr. Edson Marchiori Rua Thomaz Cameron, 438, Valparaíso Petrópolis, RJ, Brazil, 25685-120 E-mail: edmarchiori@gmail.com Study developed at Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554