Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
CASE REPORT
|
|
Leiomyosarcoma of the inferior vena cava: a case report |
|
|
Autho(rs): Rafael Lemos Nascif1; Ana Graziela Santana Antón2; Gabriel Lacerda Fernandes1; George Caldas Dantas1; Vinícius de Araújo Gomes3; Marcelo Ricardo Canuto Natal4 |
|
|
Keywords: Leiomyosarcoma; Inferior vena cava; Computed tomography. |
|
|
Abstract: INTRODUCTION
Leiomyosarcoma of the inferior vena cava (IVC) is a malignant tumor that develops from middle layer smooth muscle cells. It is the most common tumor of the venous system, most frequently affecting the IVC and representing 5% to 10% of all soft parts sarcomas(1,2). In the retroperitoneum, leiomyosarcomas and liposarcomas are the most common types of sarcomas(3). Mild, nonspecific abdominal pain is the most prevalent symptom, preceding the diagnosis in months or even years(4). Its incidence peak is in the sixth decade of life, with predominance in women(4,5). The mean size of the tumor at the moment of the diagnosis is 10.8 cm(4). Complete surgical resection with negative margins represents the only chance for long term survival of the patient(1,6). Random clinical trials utilizing chemotherapy and radiotherapy have not demonstrated any benefit to patients' survival(6). CASE REPORT A female, 48-year-old, hypertensive patient who had previously undergone kidney transplant, was admitted complaining of moderate abdominal pain, gastric plenitude, abdominal distention and bulging of the upper part of the abdomen. At physical examination, the patient presented with distended abdomen painful at palpation, with a palpable, round, hard mass located in the epigastrium and without lower limbs edema. Computed tomography (CT) demonstrated the presence of a large, well defined retroperitoneal mass, with heterogeneous contrast uptake and slightly lobulated contours (Figure 1). The lesion extended from the hepatic hilum up to the aortic bifurcation, and was in close contact with the IVC, causing distortion in some segments of the vessel, making it imperceptible, particularly in its infrarenal portion, displacing the pancreatic head without a clear cleavage plane (Figures 1, 2 and 3). Cavography demonstrated dilatation of the infrarenal segment of the IVC, with negative images of irregular contrast uptake representing the irregular filling pattern (Figure 4). 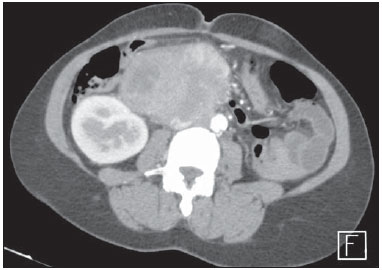 Figure 1. Contrast-enhanced, axial abdominal CT image demonstrating the presence of a heterogeneously enhanced, large slightly lobulated mass in close contact with the IVC, and a small intraluminal component. 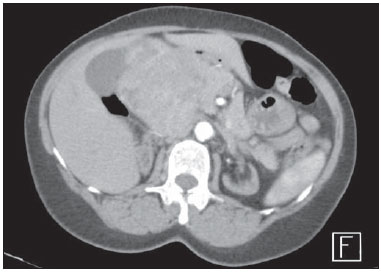 Figure 2. Contrast-enhanced, axial abdominal CT image demonstrating the lesion extending up to the hepatic hilum, displacing the pancreatic head, with imperceptible signal from the IVC. 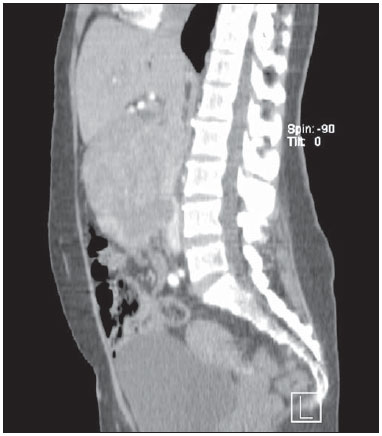 Figure 3. Non-contrast-enhanced, sagittal abdominal CT image more clearly demonstrating the intraluminal component in the IVC as well as the relationship between the lesion and the hepatic hilum. 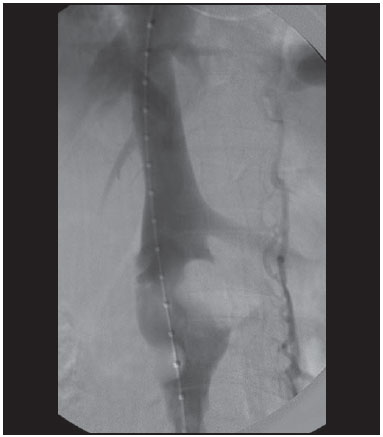 Figure 4. Cavography demonstrating two points of failure in the filling of the vessel, representing the intraluminal component of the lesion with dilatation upstream. Differential diagnoses included lymphoma, primary retroperitoneal leiomyosarcoma, leiomyosarcoma of the IVC, and metastasis. Ultrasonography-guided biopsy was performed and histological and immunohistochemical analyses revealed leiomyosarcoma. The patient was submitted to surgery, with en bloc resection of the tumor mass and of a 9 cm-segment of the infrahepatic IVC invaded by the lesion. The IVC was reconstructed with Dacron prosthesis implantation. DISCUSSION In a reference to the PubMed database, only 85 out of a total of 1210 cases of tumors involving the IVC reported in the literature in the period from 1961 to 2008 were primary leiomyosarcomas of the IVC, and in the absolute majority of cases there was secondary neoplastic involvement of other organs(7). Leiomyosarcoma of the IVC is an uncommon tumor with poor prognosis; but with an aggressive surgical approach in association with the absence of metastasis a long-term survival or even cure can be expected(3,4,6). Tumor size is one of the main prognostic factors and five-year survival is observed in 30% to 53% of patients submitted to resection with free margins(6). It may be difficult to differentiate between a sarcoma of IVC and another soft parts sarcoma of the retroperitoneum involving the IVC(6). The true sarcoma of IVC originates from smooth muscle cells of the vessel and its growth pattern may be either intra- or extraluminal, with possibility of invasion of adjacent structures(6). In cases of tumors with intraluminal growth, the vessel lumen is dilated and filled by the mass(7). The abdominal cavity has room for the growth of a tumor without causing symptoms or recognizable signs at early stages of the disease(5). Liposarcomas and leiomyosarcomas are the most common soft parts sarcomas of the retroperitoneum(3). Leiomyosarcomas represent about 0.5% to 1% of all malignant soft tissue tumors, followed by liposarcomas and malignant fibrous histiocytomas. At CT, the typical pattern of a leiomyosarcoma is that of retroperitoneal, lobulated, noncalcified mass, either with or without areas of low central attenuation resulting from necrosis or cystic degeneration, with no fat content and heterogeneous contrast enhancement(3,7). According to Webb et al., the signal from the IVC imperceptible at the point of maximal contact between the IVC and the retroperitoneal mass has 75% sensitivity and 100% specificity to predict the origin of the mass from the IVC(8) (Figure 2). Most data regarding treatment of leiomyosarcomas of IVC come from case reports and small series. Therefore, the strategies for an ideal treatment remain uncertain(6). Imaging methods play a relevant role in the characterization and preoperative staging of retroperitoneal masses, showing the lesions extent as well as their relationship with adjacent organs and structures(5). Complete surgical resection with negative margins represents the only chance for long term survival of the patient(1,6). Random clinical trials utilizing chemotherapy and radiotherapy have not demonstrated any benefit to patients' survival(6). The present report describes a rare case that should be included in the differential diagnosis of retroperitoneal masses, considering that the surgical planning impacts the patient's survival(1,2,5). REFERENCES 1. Imao T, Amano T, Takemae K. Leiomyosarcoma of the renal vein. Int J Clin Oncol. 2011;16:76-9. 2. Sokolich J, Mejia A, Cheng S, et al. Retroperitoneal leiomyosarcoma of the inferior vena cava mimicking a liver tumor. Am Surg. 2008;74:433-6. 3. Cantwell CP, Stack J. Abdominal aortic invasion by leiomyosarcoma. Abdom Imaging. 2006;31:120-2. 4. Drukker L, Alberton J, Reissman P. Leiomyosarcoma of the inferior vena cava: radical surgery without vascular reconstruction. Vasc Endovascular Surg. 2012;46:688-90. 5. Sessa B, Iannicelli E, Caterino S, et al. Imaging of leiomyosarcoma of the inferior vena cava: comparison of 2 cases and review of the literature. Cancer Imaging. 2010;10:80-4. 6. Dew J, Hansen K, Hammon J, et al. Leiomyosarcoma of the inferior vena cava: surgical management and clinical results. Am Surg. 2005;71:497-501. 7. Narata M, Okuhata Y, Abe K, et al. Primary leiomyosarcoma of the inferior vena cava: case report. Abdom Imaging. 2010;35:481-4. 8. Webb EM, Wang ZJ, Westphalen AC, et al. Can CT features differentiate between inferior vena cava leiomyosarcomas and primary retroperitoneal masses? AJR Am J Roentgenol. 2013;200:205-9. 1. MDs, Residents of Radiology and Imaging Diagnosis, Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil 2. MD, Radiologist, Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil 3. MD, Radiologist, Preceptor of Medical Residency of Radiology and Imaging Diagnosis at Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil 4. MD, Radiologist, Head of Medical Residency of Radiology and Imaging Diagnosis at Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil Mailing Address: Dr. Rafael Lemos Nascif SHN, Quadra 5, Bloco B, ap. 1108, Asa Norte Brasília, DF, Brazil, 70705-000 E-mail: rafaelnascif@gmail.com Received August 30, 2013. Accepted after revision January 6, 2014. Study developed at Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554