Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 5 - Sep. / Oct. of 2014
Vol. 47 nº 5 - Sep. / Oct. of 2014
|
CASE REPORT
|
|
Clinical and radiological repercussions of plexiform neurofibroma in the pelvic region |
|
|
Autho(rs): Érica Bertolace Slaibi1; João Gabriel Lima Daher2; Gustavo Guida Godinho da Fonseca3; Carlos Magno Daher4; Mauro Geller5; Márcia Gonçalves Ribeiro6 |
|
|
Keywords: Neurofibromatosis type 1; Plexiform neurofibroma; Pelvis. |
|
|
Abstract: INTRODUCTION
Neurofibromatosis type 1 (NF1) is the most common phakomatosis. It is an autosomal dominant inherited disease, with full penetrance and variable expressiveness, high rate of mutations, wide clinical spectrum and intrafamilial variability. Diagnostic criteria include: presence of café-au-lait spots, neurofibromas, ephelides, optic gliomas, typical bone alterations, Lisch nodules and positive family history, besides other clinical manifestations. In 2004, 1.5 million NF1 cases were reported in the world, 80 thousand in Brazil(1). Plexiform neurofibroma (PNF) is a vascularized benign tumor that involves fascicles and nerve branches, with a low tendency to present distant metastasis. Malignization is observed in 2-5% of cases. Plexiform neurofibroma occurs in 16-40% of cases of neurofibromatosis, affecting any organ, with predominance in the trunk, head, neck and extremities(1), and causes significant morbimortality due to its propensity to grow, affecting adjacent tissues. As the disease is present in the lower abdomen, depending on the size and evolution grade, it affects bowel, bladder and sexual functions(1). The authors report the case of a patient with PNF in the pelvic region, emphasizing the relevance of an early diagnosis and follow-up. CASE REPORT A 36-year-old male patient with diagnosis of NF1 since the age of 20, complaining of dysuria, polyuria, nocturia and lumbar pain for one year. Physical examination results were compatible with NF1 (cafe-au-lait spots; ephelides; skin and subcutaneous neurofibromas; Lisch nodules; thoracic scoliosis) and prostate enlargement was found at rectal digital examination. Laboratory tests results, including specific prostate antigen levels were normal. Contrast-enhanced magnetic resonance imaging (MRI) of the pelvis and column (dorsal and lumbosacral) was performed for investigation. Dorsal and lumbosacral MRI demonstrated the presence of isointense nodular lesions at T1-weighted sequence, and hyperintense nodular lesions at T2-weighted and STIR sequences. Major lesions measured 2.1 cm, and some of them were in communication with the neural foramens (Figure 1). A similar finding was observed in the muscle structures, neurovascular bundles and on the skin plane of the dorsal lumbar region. Pelvic MRI demonstrated the presence of an expansile, lobulated mass that was isointense at T1- and hypointense at T2-weighted sequence, with low contrast uptake, measuring 10.6 × 7.0 × 6.2 cm, located superiorly to the prostate and posteriorly to the bladder, and with no cleavage plane with the prostate and bladder (Figure 2). Transrectal prostate ultrasonography (US) identified a heterogeneous mass projecting towards the lumen of the bladder, as well as heterogeneous nodules, with increased gland volume. US-guided core biopsy of the prostate confirmed the presence of a tumor mass of neural nature, compatible with PNF. Two months later, new MRI demonstrated the persistence of the lesions located beside the nerve roots in the dorsal and lumbosacral regions (Figure 3), along the sciatic nerve and intermingled with the gluteus muscle. Also, the expansile mass remained with heterogeneous signal intensity, predominantly reduced at T2-weighted sequence, with foci of higher signal intensity and irregular contrast uptake. The mass measured 11.5 × 6.7 × 6.0 cm and was in close relationship with the prostate base and the posterior wall of the bladder. Additionally, bladder with reduced capacity, ballottment of seminal vesicles and thick and irregular left deferent duct were identified. 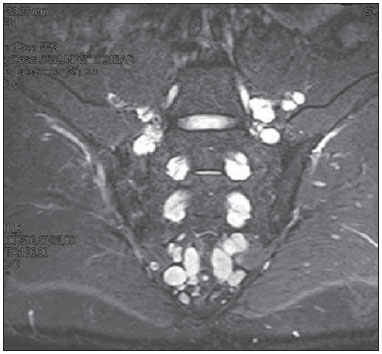 Figure 1. Lumbosacral column MRI showing isointense ovoid and elongated images on T1-weighted, and hyperintense images on T2-weighted and STIR sequences. The lesions vary in size and are located at the level of the neural foramens, with extraforaminal extension. 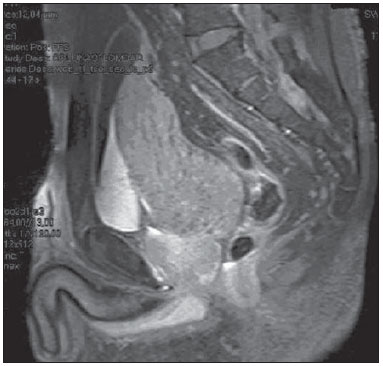 Figure 2. Pelvic magnetic resonance imaging identifying a large expansile mass, with isointense signal on T1-weighted sequence and hypointense signal on T2-weighted sequence. Poor contrast uptake is observed in the prostate region and on the posterior bladder wall. The bladder is elongated, distended and anterosuperiorly displaced. 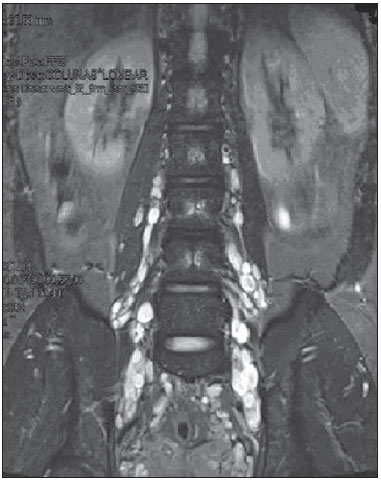 Figure 3. Magnetic resonance imaging demonstrating multiple nodular, stringshaped lesions distributed along the nerve roots of the sacral plexus, in the perivascular retroperitoneum, adjacent to the obturator muscles and in the periprostatic neurovascular bundle. Clinical and radiological follow-up every six months for three years and six months has not recorded any complaint of pain, neurological findings or growth of the pelvic mass. Until the present moment, surgical intervention is contraindicated. The patient was instructed to communicate any clinical alteration, particularly in relation to pain and urinary manifestations. DISCUSSION Location of PNF in the pelvis is uncommon(3). This type of neurofibroma originates from nerves in the pelvis, bladder and from prostatic nerve plexus. Such condition affects children and young adults, and may be isolated, superficial or infiltrating(3,4). Generally, the bladder is affected, with occurrence of obstructive symptoms, urinary incontinence, flank pain, hematuria or polyuria(4). The approach to be adopted is still to be established and the objective is the management of symptoms(1,5). In cases of pelvic location, there is a risk of 12-29% for malignant degeneration, and periodical clinical and radiological follow-up is indicated(1,5). Clinical signs raising suspicion for malignization include onset of persistent pain, neurological deficit and growth of tumor mass. MRI is currently the best imaging method, allowing the identification of neurofibromas and other lesions associated with the disease and distinguishing PNF from malignant peripheral nerve sheath tumor, since it can better characterize the nature and extent of neurofibromas(6-9). The relevance of contrast-enhanced MRI and fat saturation techniques is highlighted to differentiate between malignant and benign lesions. Additionally, at contrast-enhanced MRI, asymmetrical growth and heterogeneous pattern of a lesion (either due to necrotic areas, hemorrhage, or heterogeneous contrast uptake) indicate malignancy(6,7). At MRI, PNFs show intermediate to slightly hyperintense signal in relation to muscle on T1-weighted sequences; and on T2-weighted sequences, the lesions are hyperintense and may present hypointense septations(9). The presence of findings suggestive of PNF at imaging studies (particularly contrast-enhanced MRI) in patients with NF1 makes biopsy unnecessary to confirm the diagnosis(9). Until the present moment, no significant sign of increase in size of the PNF was observed in the present case. Surgical resection is a complex procedure, particularly in cases of atypical location, considering the proximity of critical anatomical structures. Thus, surgery should be indicated in cases of clinical and radiological suspicion of malignancy, considering the inherent risks of the procedure and the high frequency of tumor recurrence(5). The present case report demonstrates the clinical complexity of NF1. Despite the rarity of pelvic involvement, it is important to have in mind that NF1 may be associated with multiple symptoms. PNFs should be included in the differential diagnosis of extensive and bilateral pelvic masses because they may simulate several frequent retroperitoneal diseases (lymph node enlargement, abscesses, other neurogenic tumors, metastases or soft tissue sarcomas). The authors reiterate the necessity of semestral clinical and radiological follow-up to keep vigilance against malignization. Acknowledgement To Centro Nacional de Neurofibromatose (CNNF). REFERENCES 1. Geller M, Bonalumi AF. Neurofibromatose: clínica, genética e terapêutica. 1ª ed. Rio de Janeiro: Guanabara Koogan; 2004. 2. Rubenstein AE, Korf BR. Neurofibromatosis. A handbook for patients, families, and health care professionals. 1st ed. New York: Thieme; 1990. 3. Castillo PMC, Gregorio SA, Alcaide JRC, et al. Neurofibroma de la vejiga: caso clínico y revisión de la literatura. Arch Esp Urol. 2006;59:899-901. 4. Cheng L, Scheithauer BW, Leibovich BC, et al. Neurofibroma of the urinary bladder. Cancer. 1999;86:505-13. 5. Nunes TF, Costa RP, Navarro FC. Von Recklinghausen's disease with urogenital manifestation. Int Braz J Urol. 2005;31:153-4. 6. Ros PR, Eshaghi N. Plexiform neurofibroma of the pelvis: CT and MRI findings. Magn Reson Imaging. 1991;9:463-5. 7. Mautner VF, Friedrich RE, von Deimling A, et al. Malignant peripheral nerve sheath tumours in neurofibromatosis type 1: MRI supports the diagnosis of malignant plexiform neurofibroma. Neuroradiology. 2003;45:618-25. 8. Jana M, Gamanagatti S, Kumar R, et al. Pelvic neurofibroma arising from prostate in a case of neurofibromatosis-1. Indian J Urol. 2011;27:415-7. 9. Cançado DD, Leijoto CC, Carvalho CES, et al. Neurofibromatose plexiforme retroperitoneal e pélvica: aspectos na tomografia computadorizada e ressonância magnética - relato de caso e revisão da literatura. Radiol Bras. 2005;38:239-42. 1. Trainee in Dermatology at Instituto de Dermatologia Prof. Rubem David Azulay - Santa Casa da Misericórdia do Rio de Janeiro (IDPRDA/SCMRJ), MD, Collaborator of Centro Nacional de Neurofibromatose (CNNF), Rio de Janeiro, RJ, Brazil 2. Specialist in Medical Genetics, Physician at Centro Nacional de Neurofibromatose (CNNF), Rio de Janeiro, RJ, Brazil 3. Specialist in Medical Genetics, Physician at Instituto de Puericultura e Pediatria Martagão Gesteira - Universidade Federal do Rio de Janeiro (IPPMG-UFRJ), Rio de Janeiro, RJ, Brazil 4. MD, Radiologist, Casa de Saúde João XXIII, Itaocara, RJ, Brazil 5. Full Professor of Clinical Immunology, Instituto de Pós-Graduação Médica Carlos Chagas (IPGMCC), Teacher and Coordinator, Unit of Phakomatosis, Service of Genetics, Instituto de Puericultura e Pediatria Martagão Gesteira - Universidade Federal do Rio de Janeiro (IPPMG/UFRJ), Rio de Janeiro, RJ, Brazil 6. PhD of Biological Sciences (Genetics), Associate Professor, Department of Pediatrics, School of Medicine, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Mailing Address: Dra. Érica Bertolace Slaibi Rua Voluntários da Pátria, 401, Centro Visconde do Rio Branco, MG, Brazil, 36520-000 E-mail: ericaslaibi@bol.com.br Received December 19, 2012. Accepted after revision November 19, 2013. Study developed at Centro Nacional de Neurofibromatose (CNNF), Instituto de Dermatologia Prof. Rubem David Azulay - Santa Casa da Misericórdia do Rio de Janeiro (IDPRDA/SCMRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554