Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 5 - Sep. / Oct. of 2014
Vol. 47 nº 5 - Sep. / Oct. of 2014
|
CASE REPORT
|
|
Atypical retroperitoneal endometriosis and use of tamoxifen |
|
|
Autho(rs): Daniel Zambuzzi Naufel1; Thiago José Penachim2; Leandro Luiz Lopes de Freitas3; Patricia Prando Cardia2; Adilson Prando4 |
|
|
Keywords: Endometriosis; Ureter; Tamoxifen; Magnetic resonance imaging; Biopsy. |
|
|
Abstract: INTRODUCTION
Tamoxifen, a drug that is widely used in the chemotherapeutic management of breast cancer because of its antiestrogenic action in the breast tissue, has also an agonist effect on the endometrium. In long-term therapies, this drug leads to endometrial proliferative disorders, including a wide spectrum of endometrial abnormalities such as endometrial hyperplasia, hyperplastic polyps and endometrial cancer, besides being associated with endometriosis in postmenopausal patients(1). In the last years, many studies have been published about imaging diagnosis of endometriosis, highlighting particularly the role of transvaginal ultrasonography (US) and magnetic resonance imaging (MRI) as methods of choice. Such methods allow for an appropriate assessment of involved sites, as well as the surgical planning, as necessary. In cases of dubious diagnosis, percutaneous biopsy represents a useful and less invasive alternative to confirm the diagnosis. In the present case report, the authors highlight the value of pelvic MRI findings that have led to the diagnostic suspicion of periureteral lesion in a postmenopausal patient undergoing tamoxifen therapy for breast cancer, who presented with left lumbar pain secondary to hydronephrosis. The differential diagnosis of metastasis from breast cancer could be ruled out and the diagnosis of endometriosis could be histopathologically confirmed by means of multislice computed tomography (MCT)-guided percutaneous biopsy. CASE REPORT A 55-year-old female patient with previous history of breast cancer, undergoing tamoxifen therapy for two years, without any other comorbidity or history of surgery, presented with nonspecific left lumbar pain. She was submitted to US that demonstrated left hydronephrosis, with no noticeable obstructive factor. Complementary MRI showed the presence of a solid retroperitoneal tissue with retractile aspect involving the left ureter at the level of the intersection with the iliac vessels, causing ureteral stenosis and hydronephrosis (Figure 1). 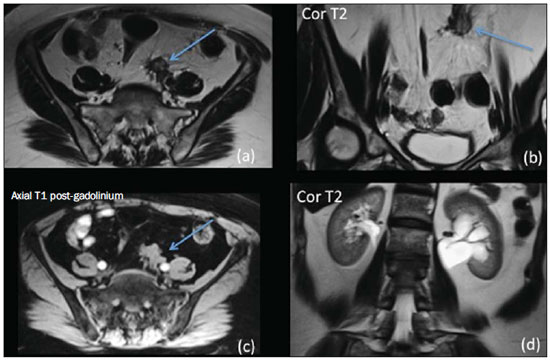 Figure 1. MRI: axial T2-weighted (a), coronal (b) and T1-weighted image with fat-suppression (c) revealing retroperitoneal solid, retractile tissue (arrows) with predominant low signal intensity on T1- and T2-weighted sequences, located in periureteral site at the level of the intersection with iliac vessels, determining ureteral obstruction and hydronephrosis (d). Ureteroscopy demonstrated an intraluminal polypoid lesion whose biopsy results were compatible with chronic inflammatory process. Considering the patient's history of breast cancer, the possibility of metastatic involvement of the left ureter was considered, and MCT-guided percutaneous biopsy(2) (Figure 2), with an 18-gauge needle was performed. 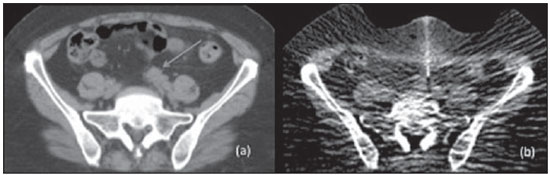 Figure 2. a: Percutaneous biopsy of a left retroperitoneal periureteral retractile lesion (arrow). b: Anterior abdominal approach with extrinsic compression of the abdominal wall for bowel loops separation. The histopathological result was compatible with endometriotic tissue (Figure 3), so oncologic therapy was ruled out, and clinical treatment for deep pelvic endometriosis was initiated, considering a surgical approach with ureteral reimplant. As the patient was about to complete the therapy with tamoxifen, the use of this drug was discontinued in an attempt to allow regression and spontaneous volumetric reduction of the endometriotic tissue, which in fact has occurred. Two months later the patient became asymptomatic, with no significant compromise of the renal filtration and excretion at 99mTc-DTPA renography. Up to now an invasive approach has not been necessary . If the patient remained symptomatic or in case of renal function compromise, a surgical resection of the fibrotic tissue and of the affected ureteral segment would be needed, with ureteroureteral anastomosis or ureterovesical bypass with a psoic bladder. 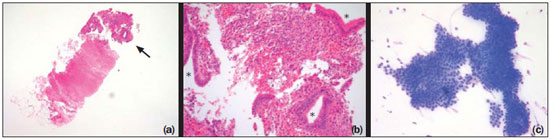 Figure 3. a: Filiform fragment of fibroadipose tissue showing tubular glands intermingled with spindle cell stroma in one of the extremities (hematoxylin-eosin staining, 100× magnification). b: Squamous and cylindrical glandular epithelium with no atypical finding (asterisk) intermingled with spindle cell stroma with foci of hemorrhage, both with appearance resembling endometrium (hematoxylin-eosin staining, 400× magnification). c: Cytological preparation performed during the biopsy specimen collection (in order to evaluate the appropriateness of the specimen) showing a large cluster of epithelial cells with no atypias (panoptic staining, 400× magnification). DISCUSSION Endometriosis, defined as presence of endometrial tissue in extrauterine locations, possibly causing dysmenorrhea, dyspareunia, pelvic pain and infertility(3), is an extremely rare entity in postmenopausal women. Frequent sites of endometriotic involvement include ovaries, uterine ligaments, serous surfaces, Douglas cul-de-sac, uterine tubes, rectosigmoid, and the vesicouterine space(3,4). However, endometriotic implants may affect the urinary tract in up to 20% of cases, affecting, in decrescent order, bladder, distal ureter, kidneys and urethra. Ureteral endometriosis rarely occurs, representing only 0.08% to 1% of cases, particularly in premenopausal women(5,6). Several unusual manifestations of endometriosis have been observed because of the increasing utilization of diagnostic imaging methods such as US and principally MRI. The multiplanar imaging capability and the high sensitivity of MRI to detect hematic components, in association with the capability in identifying sites of endometriotic involvement hidden by gross adhesions, have made MRI the method of choice for the diagnosis of endometriosis(4,7,8), with sensitivity, specificity and accuracy of respectively 90-92%, 91-98% and 91-96%(9). In the present case, besides the rarity of endometriotic involvement in unusual sites and age range, what calls one's attention is the fact that the patient was under tamoxifen therapy. There is not sufficient reports in the literature to support the evidence that the use of tamoxifen can lead to the development of a previously non-existent focus of endometriosis or whether it just exacerbates pre-existing endometriotic foci; but the occurrence of an estrogen-dependent disease in postmenopausal patients submitted to tamoxifen therapy suggests a close causal relationship between the use of this drug and development of endometriosis(1). In the present case, the patient was a postmenopausal woman without previous history or symptoms suggestive of endometriosis. Thus, it is not possible to rule out the possibility of development of a previously non-existent focus of endometriosis, or even a clinical exacerbation of an, until then, asymptomatic disease secondary to the use of tamoxifen. Given the relevance of imaging diagnosis of this disease, it is necessary that the radiologist recognizes and is attentive to MRI findings suggestive of this diagnosis, with emphasis on the constant necessity of evaluation and correct clinical-radiological and pathological correlation aiming at the application of appropriate therapeutic measures. Finally, the present case report highlights the rare occurrence of endometriosis in an unusual site, in a postmenopausal woman undergoing tamoxifen therapy, whose diagnosis might be suspected by MRI findings. REFERENCES 1. Ismail SM, Maulik TG. Tamoxifen-associated post-menopausal endometriosis. Histopathology. 1997;30:187-91. 2. Gupta S, Nguyen HL, Morello FA Jr, et al. Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: anatomic and technical considerations. Radiographics. 2004;24:175-89. 3. Choudhary S, Fasih N, Papadatos D, et al. Unusual imaging appearances of endometriosis. AJR Am J Roentgenol. 2009;192:1632-44. 4. Coutinho A Jr, Bittencourt LK, Pires CE, et al. MR imaging in deep pelvic endometriosis: a pictorial essay. Radiographics. 2011;31:549-67. 5. Woodward PJ, Sohaey R, Mezzetti TP Jr. Endometriosis: radiologicpathologic correlation. Radiographics. 2001;21:193-216. 6. Lima CMAO, Coutinho EPD, Ribeiro EB, et al. Ressonância magnética na endometriose do trato urinário baixo: ensaio iconográfico. Radiol Bras. 2009;42:193-7. 7. Siegelman ES, Oliver ER. MR imaging of endometriosis: ten imaging pearls. Radiographics. 2012;32:1675-91. 8. Chamié LP, Blasbalg R, Pereira RM, et al. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics. 2011;31:E77-100. 9. Glastonbury CM. The shading sign. Radiology. 2002;224:199-201. 1. MD, Trainee in Radiology and Imaging Diagnosis, Centro Radiológico Campinas - Hospital Vera Cruz, Campinas, SP, Brazil 2. MDs, Radiologists, Centro Radiológico Campinas - Hospital Vera Cruz, Campinas, SP, Brazil 3. PhD, MD, Pathologist at Laboratório Multipat, Campinas, SP, Brazil 4. MD, Radiologist, Head of the Department of Radiology and Imaging Diagnosis, Hospital Vera Cruz, Campinas, SP, Brazil Mailing Address: Dr. Daniel Zambuzzi Naufel Centro Radiológico Campinas - Hospital Vera Cruz Avenida Andrade Neves, 707, Botafogo Campinas, SP, Brazil, 13013-161 E-mail: dznaufel00@hotmail.com Received April 11, 2013. Accepted after revision November 18, 2013. Study developed at Centro Radiológico Campinas - Hospital Vera Cruz, Campinas, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554