Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 2 - Mar. / Apr. of 2014
Vol. 47 nº 2 - Mar. / Apr. of 2014
|
CASE REPORT
|
|
Bullet embolism of pulmonary artery: a case report |
|
|
Autho(rs): Mauricio Gustavo Ieiri Yamanari1; Maria Clara Dias Mansur2; Fernando Uliana Kay3; Paulo Rogerio Barboza Silverio3; Shri Krishna Jayanthi4; Marcelo Buarque de Gusmão Funari5 |
|
|
Keywords: Bullet embolism; Trauma; Computed tomography; Pulmonary arteriography. |
|
|
Abstract: INTRODUCTION
Violence is a relevant public health problem in Brazil, representing the third most common cause of death in the country. Besides social and cultural factors, violence is also related to illicit drugs and alcohol overuse in association with a wide availability of firearms(1). The effects of a bullet in the body depend on a range of factors: velocity, entrance profile, bullet diameter, path of the bullet inside the body and biological characteristics of the affected organ(2). A rare and unpredictable complication of firearm injuries is bullet embolism. With only few cases described in the literature, bullet embolism may become a diagnostic challenge for emergency physicians. Venous bullet embolism occurs even more rarely, with the following complications: heart valve dysfunction, endocarditis, septicemia, venous thrombosis, thrombophlebitis, arrhythmias and hypoxemia secondary to arterial pulmonary embolism(3). CASE REPORT The authors report the case of a male, 30-year-old patient, victim of multiple firearm injuries. At admission, the patient was hemodynamically stable, with no respiratory alteration, and complaining of pain in the pelvic region. Amongst several firearm injuries, physical examination revealed the presence of an entrance wound on the gluteal region, without an exit orifice. Plain radiography of the pelvis, lower limbs and right upper limb did not demonstrate the presence of fractures or firearm projectiles. On the other hand, chest radiography demonstrated the presence of a metal artifact compatible with a projectile located in the left pulmonary hilum. No signs of pneumothorax, hemothorax or rib fractures were observed (Figure 1). 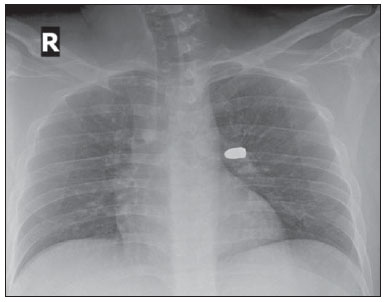 Figure 1. Plain chest radiography demonstrates the presence of a firearm projectile in the left pulmonary hilum. Neither pneumothorax, hemothorax nor fractures are identified. Chest computed tomography (CT) demonstrated that the metal artifact was located in the transition between the left pulmonary artery and the lingular artery. The other chest structures presented with a normal tomographic appearance. Abdominal and pelvic CT images were also acquired and revealed the presence of metal fragments (Figure 2) in the projectile pathway, muscle planes of the left gluteal regions to the ipsilateral inguinal region. Densification of the fat planes was observed around the left iliac vessels (Figure 3) and the inferior vena cava, as well as a small amount of intraperitoneal fluid. 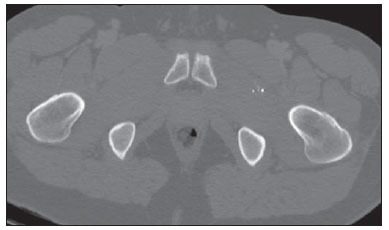 Figure 2. Pelvic computed tomography (bone window) identifies presence of metal fragments adjacent to the left pelvic muscles. 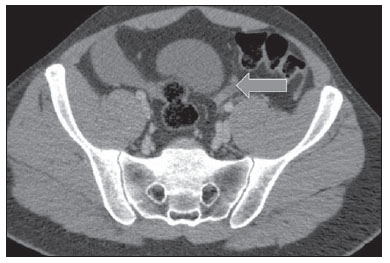 Figure 3. Pelvic computed tomography (soft tissue window) demonstrates the presence of densification adjacent to left iliac vessels and a small amount of free fluid (arrow). Based on the above described findings, bullet embolism of pulmonary artery was diagnosed, with origin in the left external iliac vein. The patient was submitted to exploratory laparotomy that detected 500 ml of blood in the peritoneal cavity, with epiploic and mesosigmoid hematoma. No sign of perforation of hollow viscera or ischemia was observed. Two days after the surgical procedure, pulmonary arteriography confirmed the presence of a bullet in the origin of the lingular artery, reducing the perfusion to the corresponding pulmonary segments (Figure 4). Two unsuccessful attempts to extract the bullet were performed. 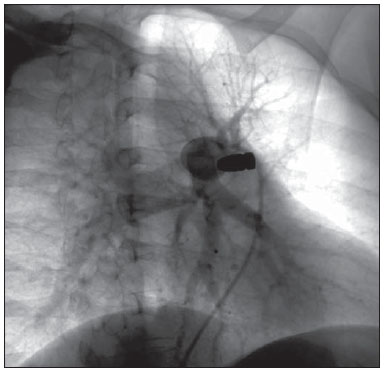 Figure 4. Pulmonary arteriography with selective characterization of left pulmonary artery demonstrates decreased blood flow toward the lingular segment of the left upper pulmonary lobe. DISCUSSION A firearm bullet may reach the body in two ways: with high velocity (military firearms) or with low velocity (civil firearms). In general, the high velocity bullet enters the body in a straight trajectory and leaves the body, while the low velocity bullet may divert through bones or soft tissues and remain lodged, or may yet penetrate vessels or cardiac walls. In most cases, bullet embolism occurs in the arterial system (80% against 20% in the venous system)(4). Arterial embolisms are symptomatic in 80% of cases (claudication/ischemia/peripheral thrombophlebitis)(5). On the other hand, most venous embolisms are asymptomatic. In cases where they are present, the symptoms may include dyspnea, hemoptysis and chest pain(6). A minority of venous embolisms are either retrograde (course of the bullet against the regular direction of the blood flow)(6), or paradoxical, defined as the trajectory of the bullet from the venous system to the arterial system through an arteriovenous fistula, perforation of the atrioventricular septum or ventricular defect through the patent ovale foramen. Bullet embolism should be actively investigated in cases where a bullet enters the body and an exit wound is not characterized. The authors suggest performing whole body radiography or CT, as available in the unit. Angiography remains reserved for supplementary diagnosis or to be used as a therapeutic endovascular extraction procedure. The accurate localization of the bullet is extremely important for the therapeutic planning. Despite controversies, most authors admit an expectant conservative approach in cases of asymptomatic patients with bullet embolism of the venous system, and surgical or endovascular approach in the presence of symptoms or risk for thrombosis or displacement of the bullet(3,7). Bullet embolism of the arterial system is also a surgical indication(8). In the present case, the patient remained asymptomatic during the whole hospital stay, both before and after the attempt to extract the bullet by means of pulmonary arteriography. So, the option was conservative treatment with follow-up on an outpatient basis. REFERENCES 1. Reichenheim ME, de Souza ER, Moraes CL, et al. Violence and injuries in Brazil: the effect, progress made, and challenges ahead. Lancet. 2011;377:1962-75. 2. Lichte P, Oberbeck R, Binnebösel M, et al. A civilian perspective on ballistic trauma and gunshot injuries. Scand J Trauma Resusc Emerg Med. 2010;18:35. 3. Miller KR, Benns MV, Sciarretta JD, et al. The evolving management of venous bullet emboli: a case series and literature review. Injury. 2011;42:441-6. 4. Colquhoun IW, Jamieson MP, Pollock JC. Venous bullet embolism: a complication of airgun pellet injuries. Scott Med J. 1991;36:16-7. 5. Schurr M, McCord S, Croce M. Paradoxical bullet embolism: case report and literature review. J Trauma. 1996;40:1034-6. 6. Schmelzer V, Mendez-Picon G, Gervin AS. Case report: transthoracic retrograde venous bullet embolization. J Trauma. 1989;29:525-7. 7. Hassan AM, Cooley RS, Papadimos TJ, et al. Pulmonar bullet embolism - a safe treatment strategy of a potentially fatal injury: a case report. Patient Saf Surg. 2009;3:12. 8. Adegboyega PA, Sustento-Reodica N, Adesokan A. Arterial bullet embolism resulting in delayed vascular insufficiency: a rationale for mandatory extraction. J Trauma. 1996;41:539-41. 1. Physician Assistant at Instituto da Criança - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (ICr/HC-FMUSP), Radiologist at Imaging Department - Hospital Israelita Albert Einstein, São Paulo, SP, Brazil 2. Fellow of Neuroradiology, Instituto de Radiologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil 3. Physicians Assistants, Instituto de Radiologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), Radiologists at Imaging Department - Hospital Israelita Albert Einstein, São Paulo, SP, Brazil 4. Chief of Emergency Unit, Instituto de Radiologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil 5. Chief of Chest Division, Instituto de Radiologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), Chief of Imaging Department - Hospital Israelita Albert Einstein, São Paulo, SP, Brazil Mailing Address Dr. Mauricio Gustavo Ieiri Yamanari Rua Oscar Freire, 1735, ap. 131, Cerqueira César São Paulo, SP, Brazil, 05409-011 E-mail: mauriciogustavo91@yahoo.com.br Received May 23, 2013. Accepted after revision July 30, 2013. Study developed at Instituto de Radiologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554