Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 2 - Mar. / Apr. of 2014
Vol. 47 nº 2 - Mar. / Apr. of 2014
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Alexandre Dias Mançano1; Rubens Carneiro dos Santos Neto2; Karla Coelho Caixeta e Silva3 |
|
|
A 62-year-old man attended the emergency department, complaining of cough and respiratory distress. The patient denied fever and reported a history of chronic cough that had worsened for the last five years, with crises of respiratory distress which he had never experienced before. According to the patient, he suffered from asthma from his childhood, with bronchitis crises which worsen with physical activity, weather changes or exposure to dust and mold. The patient was formerly a smoker during 26 years and quitted smoking for twenty years. He denied regular clinical follow-up or previous treatments. He usually attends the emergency department and has already been admitted for treatment of some pneumonias. At auscultation, the patient presented with crepitations and stertors in the lung bases and wheezing. Chest radiography was requested and demonstrated sparse reticular opacities more extensively located in the right lower lobe, besides bronchiectasis. In order to deepen the investigation, chest computed tomography was requested (Figures 1 and 2).
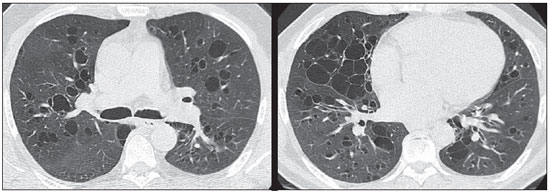 Figure 1. High resolution computed tomography with sections of the middle and lower pulmonary regions. 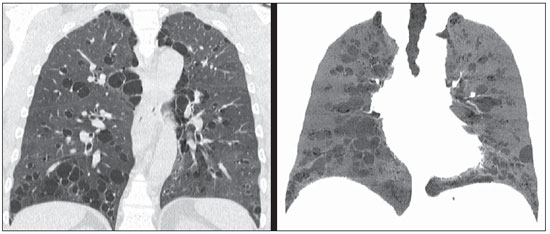 Figure 2. Computed tomography with coronal and MINIP reconstructions. Images description Figures 1 and 2. Chest computed tomography images demonstrate the presence of thin walled cystic bronchiectasis diffusely distributed throughout the lungs. Trachea, main bronchi and lobar bronchi are not affected by the disease. Diagnosis: Williams-Campbell syndrome. COMMENTS Williams-Campbell syndrome is a rare, congenital condition caused by a deficiency of cartilage in the subsegmental bronchi, leading to bronchiectasis and distal airways collapse(1,2). The cartilage rings deficiency in the fourth- to sixth-order bronchi results in distal bronchiectasis, with the trachea and main bronchi remaining intact(3). Such a syndrome is commonly described in children with a history of recurrent pneumonias and obstructive symptoms; and is occasionally diagnosed in adult individuals(2-4). There are descriptions of familial occurrence, suggesting the necessity of investigation of all the family members(1,5). Clinical symptoms include cough, wheezing and recurrent pneumonias(1,5). Respiratory function tests demonstrate an obstructive pattern and, in advanced disease may present a mixed pattern. The cartilage deficiency changes the bronchial physiology, causing dilatation during inspiration and collapse at expiration, determining hyperinsuflation and segmental/lobar collapse(3,5). Such alteration leads to air trapping, impairing the airway drainage and resulting in secretion accumulation(3,4). The recurrent destruction of the bronchial tree and inappropriate mucus drainage result in parenchymal destruction distally to the bronchiectasis. The symptoms severity and disease prognosis depend on the degree and extent of the cartilage involvement(2). The imaging finding at conventional radiography corresponds to symmetrical bronchiectasis. High resolution computed tomography demonstrates distal, cystic bronchiectasis in fourth- to sixth-order bronchi, with variable extent and no involvement of the trachea and main bronchi(2). Normality of the proximal bronchial tree is typical of the syndrome and is the main finding for differentiation with Mounier-Kuhn syndrome (tracheobronchomalacia)(5,6). Additionally, mucoid impaction is observed in some bronchi, predominantly in the lower lobes, besides concomitant findings of infectious disease characterized by a tree-in-bud pattern. Also, a mosaic attenuation pattern may be observed(1). The diagnosis is based on clinical and tomographic findings in addition to the previous and familial history of the patient, besides laboratory tests to rule out other hypotheses. No significant finding is observed at bronchoscopy(1,2). The main differential diagnosis is Mounier-Kuhn syndrome (tracheobronchomalacia), besides alpha-1 antitrypsin, cystic fibrosis, allergic bronchopulmonary aspergillosis and ciliary diskynesia syndrome(1,2,4). There is no specific treatment for Williams-Campbell syndrome, and prophylaxis and management of exacerbations represent the main method of treatment based on respiratory physiotherapy and antibiotic therapy. The literature includes the description of some cases of pulmonary transplant, though without great success. In one of such cases, the post-mortem finding was post-transplant brochomalacia(1,3,7). REFERENCES 1. Konoglou M, Porpodis K, Zarogoulidis P, et al. Williams-Campbell syndrome: a case report. Int J Gen Med. 2012;5:41-4. 2. Di Scioscio V, Zompatori M, Mistura I, et al. The role of spiral multidetector dynamic CT in the study of Williams-Campbell syndrome. Acta Radiol. 2006;47:798-800. 3. George J, Jain R, Tariq SM. CT bronchoscopy in the diagnosis of Williams-Campbell syndrome. Respirology. 2006;11:117-9. 4. Cantin L, Bankier AA, Eisenberg RL. Bronchiectasis. AJR Am J Roentgenol. 2009;193:W158-71. 5. McAdams HP, Erasmus J. Chest case of the day. Williams-Campbell syndrome. AJR Am J Roentgenol. 1995;165:190-1. 6. Marom EM, Goodman PC, McAdams HP. Diffuse abnormalities of the trachea and main bronchi. AJR Am J Roentgenol. 2001;176:713-7. 7. Burguete SR, Levine SM, Restrepo MI, et al. Lung transplantation for Williams-Campbell syndrome with a probable familial association. Respir Care. 2012;57:1505-8. 1. MD, Radiologist, Radiologia Anchieta – Hospital Anchieta, Coordinator for Medical Residency at Hospital Regional de Taguatinga, Taguatinga, DF, Brazil 2. MD, Trainee at Radiologia Anchieta – Hospital Anchieta, Taguatinga, DF, Brazil 3. MD, Resident at Hospital Regional de Taguatinga, Taguatinga, DF, Brazil Mailing Address: Dr. Alexandre Dias Mançano Centro Médico Hospitalar Anchieta AE 8/10, Setor C Norte, 1º subsolo, Centro de Excelência Anchieta, lojas 12 e 13 Taguatinga, DF, Brazil, 72115-700 E-mail: alex.manzano1@gmail.com Study developed at Radiologia Anchieta – Hospital Anchieta, Taguatinga, DF, Brazil |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554