Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 1 - Jan. /Feb. of 2014
Vol. 47 nº 1 - Jan. /Feb. of 2014
|
CASE REPORT
|
|
Lithium nephropathy: a case report |
|
|
Autho(rs): Raphael Reis Pereira-Silva1; Débora Esperancini-Tebar2 |
|
|
Keywords: Lithium nephropathy; Renal microcysts; Bipolar disorder. |
|
|
Abstract: INTRODUCTION
Since 1970, when lithium was approved by the U. S. Food and Drug Administration, it started being widely utilized in the treatment of bipolar disorder(1). It is currently the drug of choice for such disorder, and is utilized to prevent recurrence and to minimize the suicide risk. This drug is efficacious in drastically reducing depressive and maniac symptoms in 70-80% of cases(2). Despite its proven benefits, the use of lithium may bring adverse effects associated with the urinary, endocrine and neurological systems(1). Several studies have reported lithium-related renal complications, such as nephrogenic diabetes insipidus, renal tubular acidosis, tubulointerstitial nephritis and nephrotic syndrome(1). It seems there is a direct relationship between the progression of lithium nephropathy and the time of drug use(3), which may be aggravated with the simultaneous use of other potentially nephrotoxic pharmaceuticals. Additionally, advanced age, previous episodes of lithium intoxication and presence of comorbidities such as hypertension, diabetes mellitus, hyperparathyroidism and hyperuricemia usually enhance the risk(4). Lithium therapy is the main cause of drug-induced nephrogenic diabetes insipidus, affecting 10% of patients undergoing therapy for more than 15 years(5). In most cases, clinical findings correlated with laboratory tests results can provide enough information for the diagnosis. A biopsy might be required in some circumstances where the symptoms are atypical. But recently, with the increasing use of imaging techniques, some researchers have demonstrated the relevance of such techniques in the follow-up of these conditions. The main clinical manifestations of lithium nephropathy include polydipsia and polyuria, which raise this diagnostic hypothesis(1). In the presence of an appropriate clinical context, the imaging identification of several microcysts < 2.0 mm symmetrically distributed in normal-sized kidneys suggests a causal link(1). A recent study involving patients undergoing lithium therapy submitted to ultrasonography demonstrated the presence of numerous renal microcysts and a pattern of hyperrefringent foci without posterior acoustic shadowing(1). Such hyperechogenic spots were not closely correlated with computed tomography (CT) and magnetic resonance imaging (MRI) findings, but the possibility of such findings corresponding to initial alterations of the microcysts is considered(1). As such imaging alterations are correlated with the histopathological study of lithium tubulointerstitial nephritis, the presence of microcysts in the distal tubule and interstitial fibrosis is observed(1,6). The presence of renal cysts may correspond to a series of both congenital and acquired abnormalities. Their differentiation can be made by the cysts location and morphology, patient's age, kidneys size and degree of renal function(7). Autosomal dominant polycystic kidney disease is seen at MRI as enlarged kidneys with multiple cysts varying in size and intensity; and, in about 70-75% of cases, associated with hepatic cysts(7). Glomerulocystic kidney disease is rarely seen, affecting particularly children and young adults, with cysts distributed exclusively over the renal cortex and, in some cases, associated with renal failure(7). Medullary cystic disease is characterized by chronic renal failure, decrease in the cortex thickness, and presence of cysts in the medulla and in the cortical-medullary junction(7). Acquired cystic kidney disease occurs by the development of cysts in patients with chronic renal failure or undergoing dialysis. The kidneys are small and the cysts present varied sizes and are distributed over the renal cortex and medulla(7). A careful analysis of imaging findings correlated with clinical data provides information for the diagnosis of lithium nephropathy. CASE REPORT A 59-year-old woman presented with nonspecific abdominal pain for one week, and was submitted to abdominal computed tomography. The images demonstrated normal-sized kidneys, with multiple, small intraparenchymal cystic lesions (Figure 1). MRI was performed for a better assessment of such microcysts ( < 2.0 mm) which presented with hyposignal at T1-weighted, hypersignal on T2-weighted sequences, with no paramagnetic contrast uptake, distributed both over the cortex and medulla of both kidneys (Figure 2). 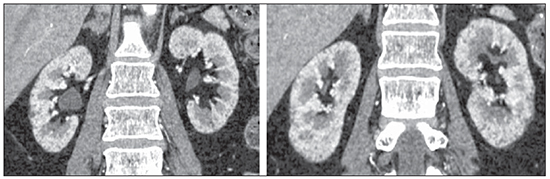 Figure 1. CT image demonstrating multiple small intraparenchymal cystic lesions in normal-sized kidneys. 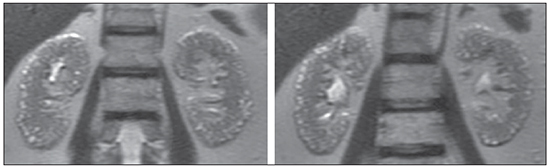 Figure 2. MRI, T2-weighted image demonstrating the presence of multiple microcysts with hypersignal distributed in both kidneys. From a careful analysis of the patient's clinical history, one could find out that she was under regular lithium carbonate therapy for bipolar disorder for more than 15 years. Additionally, the patient reported hypothyroidism, with polyuria and polydipsia which had worsened in the last times. She denied a family history of cystic kidney disease and neither presented with renal failure nor was under substitutive renal therapy. After correlating such information with the imaging findings, lithium nephropathy was considered as the main diagnostic hypothesis. DISCUSSION Despite its side effects, lithium still remains as a widely utilized drug. The action mechanism of this drug and its complications are still to be completely understood, but great advances have been observed in the last years. It is necessary to be attentive to the monitoring of such adverse effects, since an early identification might reduce the impact of such harms(8). However, the interruption of lithium therapy many times pose a dilemma, since it increases the risk for early bipolar disorder recurrence(9). Thus, the decision to replace lithium with other mood stabilizer should be made jointly by the patient and his/her doctor, although the kidney disease prognosis after lithium withdrawal is unknown(1). Scientific studies have demonstrated that the diagnosis of lithium nephropathy is rare, since 85% of patients under treatment did not presented with renal failure(3) and only 0.37% had alterations appreciable by histopathological analysis(1); hence the relevance of a clinical-radiological-histopathological correlation(1). There is a series of diseases which course with renal cysts observed at imaging studies, among them autosomal dominant polycystic kidney disease; medullary cystic disease, acquired cystic kidney disease and glomerulocystic kidney disease. The presence of several microcysts distributed in both kidneys on images of a patient undergoing lithium therapy is strongly suggestive of the diagnosis, which may dispense with biopsy(7). Sonographic images demonstrate some microcysts and hyperrefringent foci which, despite the uncertainty, may represent initial alteration of the microcysts(1). Microcysts are well characterized at computed tomography, but MRI can demonstrate kidney alterations with higher sensitivity to identify microcysts in lithium nephropathy(1,7). The present case report is aimed at calling attention to a nephropathy that tends to become prevalent and is still poorly known by most general radiologists. REFERENCES 1. Di Salvo DN, Park J, Laing FC. Lithium nephropathy: unique sonographic findings. J Ultrasound Med. 2012;31:637–44. 2. Müller-Oerlinghausen B, Berghöfer A, Bauer M. Bipolar disorder. Lancet. 2002;359:241–7. 3. Presne C, Fakhouri F, Noël LH, et al. Lithium-induced nephropathy: rate of progression and prognostic factors. Kidney Int. 2003;64:585–92. 4. Tuazon J, Casalino D, Syed E, et al. Lithium-associated kidney microcysts. ScientificWorldJournal. 2008;8:828–9. 5. Bendz H, Aurell M. Drug-induced diabetes insipidus: incidence, prevention and management. Drug Saf. 1999;21:449–56. 6. Alexander MP, Farag YM, Mittal BV, et al. Lithium toxicity: a doubleedged sword. Kidney Int. 2008;73:233–7. 7. Farres MT, Ronco P, Saadoun D, et al. Chronic lithium nephropathy: MR imaging for diagnosis. Radiology. 2003;229:570–4. 8. Livingstone C, Rampes H. Lithium: a review of its metabolic adverse effects. J Psychopharmacol. 2006;20:347–55. 9. Suppes T, Baldessarini RJ, Faedda GL, et al. Risk of recurrence following discontinuation of lithium treatment in bipolar disorder. Arch Gen Psychiatry. 1991;48:1082–8. 1. MD, Resident Radiologist at Instituto de Radiodiagnóstico Rio Preto – Ultra-X, São José do Rio Preto, SP, Brazil 2. MD, Radiologist Assistant, Department of Imaging, Hospital de Base da Faculdade de Medicina de São José do Rio Preto (Famerp), Radiologist at Instituto de Radiodiagnóstico Rio Preto – Ultra-X, São José do Rio Preto, SP, Brazil Mailing Address: Dr. Raphael Reis Pereira-Silva Rua Conselheiro Correa de Menezes, 91, Horto Florestal Salvador, BA, Brazil, 40295-030 E-mail: raphaelrpereira@hotmail.com Received January 15, 2013. Accepted after revision July 1st, 2013. Study developed at Instituto de Radiodiagnóstico Rio Preto - Ultra-X, São José do Rio Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554