Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 6 - Nov. / Dec. of 2013
Vol. 46 nº 6 - Nov. / Dec. of 2013
|
REVIEW ARTICLES
|
|
Preparation and management of complications in prostate biopsies |
|
|
Autho(rs): Chiang Jeng Tyng1; Macello José Sampaio Maciel2; Bruno Lima Moreira2; João Paulo Kawaoka Matushita Jr.2; Almir Galvão Vieira Bitencourt3; Miriam Rosalina Brites Poli4 |
|
|
Keywords: Prostate; Needle biopsy; Interventional ultrasonography; Complications. |
|
|
Abstract: INTRODUCTION
Recent studies published in Brazil have highlighted the relevance of interventional radiology to collect appropriate material for the diagnosis of several diseases in different organs(1-3). In this context, transrectal ultrasonography (US)-guided prostate biopsy is one of the most common procedures, with high sensitivity for the diagnosis of prostate cancer. The prostate biopsy technique as well as its indications and results have already been widely studied(4,5). Such procedure is relatively simple, rapid and safe, with low morbimortality. Generally, the complications are mild, but some precautions should be taken in the patients' preparation in order to avoid more severe complications. Despite the already published guidelines(6,7), there is a lack of standardization of such procedure in Brazil, so different types of preparation are adopted by the different institutions. The present study aimed to review the literature on complications related to transrectal US-guided prostate biopsy, discuss its management and directions to reduce its incidence. PREPROCEDURAL ORIENTATIONS Every patient undergoing such procedure must be previously instructed and informed about risks and possible complications. The patients' preparation for transrectal US-guided prostate biopsy is still a controversial issue. Antibiotic prophylaxis Preprocedural antibiotic prophylaxis is recommended for all patients. This concept is based on the fact that 16% to 100% of cases of biopsy with no prophylaxis presented either asymptomatic bacteriuria or transient bacteremia, increasing the risk for infectious complications such as urinary tract infection, sepsis and Fournier's syndrome(8). The antibiotic must have a spectrum for bacteria from the flora of the skin, rectum and genitourinary tract. Studies describe Escherichia coli as the main etiologic agent of infections after biopsies, but Streptococcus faecalis and bacterioid organisms are also frequently reported. The utilization of broad spectrum antibiotics is a common practice, but guidelines should be locally developed according to the microbiological profile, taking the regional antibiotic resistance into consideration. In a meta-analysis, Zani et al. have demonstrated that preprocedural antibiotic prophylaxis reduces significantly the risk for bacteriuria, bacteremia, fever, urinary tract infection and hospitalization(9). No significant difference was observed between the administration pathways, whether oral or systemic. Currently, quinolones (ciprofloxacin, for example) are the antibiotics of choice, since oral administration allows a good absorption, reaching good levels in prostatic tissue(10-12). Still there is a lack of consensus about the regimen duration. Several studies have compared a single-dose regimen with a three-dose regimen (one dose 30 to 60 minutes before the procedure and continuation for the two following days). Evidences suggest that a single dose is as effective as the prophylaxis with multiple antibiotic doses(13-15). Considering all the evidences described in the literature, availability, convenience e cost, the authors recommend antibiotic prophylaxis with oral 500 mg ciprofloxacin taken one hour before biopsy. In patients with major risk factors, such as diabetes, immunodepression, recent use of corticoids, severe urinary dysfunction or prostate volume > 75 g, antibiotic therapy may be maintained for three days, in spite of the lack of evidences in the literature justifying such strategy. In patients with history of allergy to quinolones, sulfamethoxazole-trimethoprim, piperacillin-tazobactam, cefalosporines or aminoglycosides may be utilized. Table 1 describes the recommended doses of antibiotic therapy. 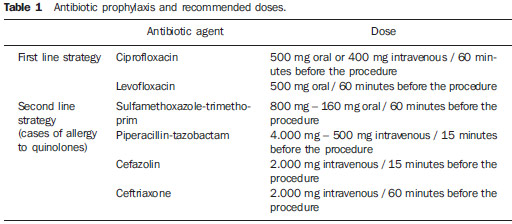 The wide utilization of quinolones has increased the rate of infections by resistant strains of E.coli. The additional utilization of intravenous aminoglycoside reduces the risk of such infection in institutions where this problem has been documented(16,17). Patients under risk for development of endocarditis or infection of prosthetic heart valves, cardiac pacemakers or implanted cardiac defibrillators, benefit from the associated use of intravenous ampicillin and gentamicin before the procedure, followed by oral quinolone for 2-3 days. Bowel preparation Bowel preparation before transrectal biopsy of prostate, either by means of enema, suppository or povidone lavage, is based on the assumption that such preparation would reduce the incidence of infectious complications by bacteria present in the rectal ampulla. Considering the fact that the rectum contains feces only during defecation, the routine utilization of pre-biopsy bowel preparation is questionable. Some authors believe that such preparation might even increase the level of bacteria in the rectum since it liquidizes the feces in the sigmoid colon and also impairs the quality of the sonographic images because of the air inserted during the preparation(18). Evidences demonstrate that there are no significant difference in the rates of infectious complications among patients submitted or not to bowel preparation, since they have undergone antibiotic prophylaxis(18,19). Thus, some authors support that bowel preparation increases the cost of the procedure and the discomfort of the patient with no additional benefit. For this reason, patients submitted to appropriate antibiotic prophylaxis do not require pre-biopsy bowel preparation. Anticoagulant and antiplatelet agents Many of the patients submitted to prostate biopsy present with increased cardiovascular risk and continuously use anticoagulant agents or antiplatelet therapy. The decision about discontinuing or continuing such therapies should be made in conjunction with the assisting physicians, taking the risks for bleeding and cardiovascular events into consideration. Although prospective studies with patients under continuous use of low doses of acetylsalicylic acid (AAS) submitted to transrectal prostate biopsy have not demonstrated any increase in the incidence of severe hemorrhagic complications(20,21), most urologists recommend discontinuation of the therapy. AAS and other nonsteroidal anti-inflammatory drugs should be discontinued three to five days before the biopsy, while clopidogrel should be discontinued seven days before, and ticlopidine, 14 days before the procedure(22,23). As regards the use of anticoagulant therapy with coumarins, the lack of evidences about post-biopsy hemorrhagic complications in such patients suggests that such therapy should be discontinued four to five days before the procedure(24,25). Further studies are necessary to change such practice and establish some recommendations according to the risk for thrombosis and indication for anticoagulation(26). Patients with history of acute venous or arterial thromboembolism in the last month preceding the biopsy should undergo the procedure as an inpatient, and with the anticoagulant therapy replaced by intravenous heparin. In cases of patients with other indications for anticoagulant therapy (for example, metal heart valves, recurrent venous thromboembolism or atrial fibrillation) and lower risk for embolic events, the therapy may be changed to subcutaneous or low-molecular-weight heparin. Anesthesia Although transrectal prostate biopsy is generally well tolerated without the use of anesthesia(27), the pain and anxiety related to the procedure may lead to unfavorable outcomes besides influencing the decision of the patient about undergoing a new biopsy. Randomized studies have demonstrated that the use of topic anesthetics alone does not reduce the pain(28-30). Thus, local anesthesia or sedation should be routinely performed in order to reduce the patient's discomfort during the procedure, particularly in younger patients and during procedures requiring the collection of a greater number of specimens. Sedation with a hypnotic agent (for example, midazolam or propofol) is generally performed by an anesthetist. Such technique promotes great satisfaction and is widely accepted by patients for reducing the discomfort secondary to the transducer positioning and the patient's fear in relation to the procedure, providing a calm environment for its performance(31,32). However, an anesthetic agent should be associated to prevent postoperative pain; fentanyl is the most utilized in such cases. But such association is not free from risks, as cases of respiratory depression may occur due to the interaction between fentanyl and propofol(31). It is important that patients that are candidates to biopsy with sedation undergo a preanesthetic assessment to determine the surgical risk and for a better anesthetic planning. The patient must be appropriately monitored during the procedure which should be preferentially performed in a hospital environment. In cases where sedation is not performed, local anesthesia with periprostatic nerve block is highly recommended. Several techniques have been described; among them the most accepted one is the injection of 5 ml of 2% lidocaine using a 7 in / 22 gauge spinal needle into the periprostatic nerve pathway, at the junction between the seminal vesicles and the base of the prostate, bilaterally (Figure 1). Evidences demonstrate that such a technique allows for a satisfactory management of the pain, without increasing the incidence of complications(32-35). 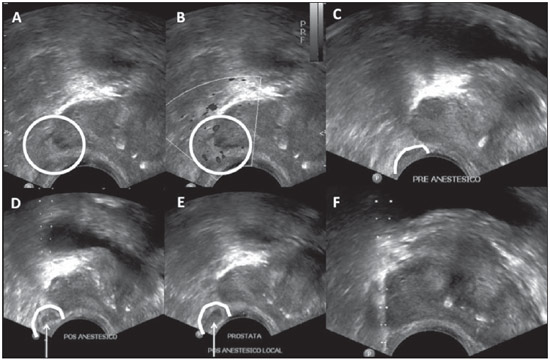 Figure 1. Ultrasonography with a step-by-step description of local anesthesia for prostate biopsy by means of periprostatic nerve block. 2% lidocaine injection with spinal needle at the junction between seminal vesicles and the base of the prostate. A,B: Identification of the angle between the seminal vesicle and the base of the prostate – B-mode (A), Doppler study (B). C: Preanesthesia. D: During anesthetic agent injection. E: Postanesthesia: An anechoic content is observed in the angle between the seminal vesicle and the base of the prostate. F: Biopsy. Systemic arterial hypertension No evidence is found in the literature to indicate an increase in the risk for complications after transrectal prostate biopsy in patients with high arterial pressure levels during the procedure. But, theoretically, there is an increased risk for bleeding in such cases. Additionally, the presence of arterial hypertension increases the risk for cardiovascular events during surgical procedures. Special care should be taken with patients undergoing procedures under sedation, considering that anesthetics may increase the systemic arterial pressure and the cardiac frequency(36,37). In general, such procedure should be avoided in patients with systolic pressure > 170 mmHg or diastolic pressure > 110 mmHg. Patients under chronic use of antihypertensive drugs should maintain their regular medication, even in the day of the procedure. The reduction of blood pressure levels could be achieved with either oral or parenteral administration of antihypertensive drugs. POSTPROCEDURAL ORIENTATIONS The patients should be advised about rest, liquids ingestion, antibiotic prophylaxis and post-biopsy follow-up. At any patient discharge after transrectal US-guided prostate biopsy, one must be sure that he has understood the potential complications from the procedure, requiring medical assistance in case of fever or other signs of infection, urinary obstruction/retention or persistent bleeding. Patients with urethral catheter or diabetes mellitus require a more strict monitoring in relation to signs of sepsis. COMPLICATIONS Transrectal US-guided prostate biopsy is generally a well tolerated procedure with no complication. The rates of discomfort and major complications do not depend on the number and site of punctures made with the biopsy needle and their incidence is not higher in patients submitted to an initial biopsy or rebiopsy after some weeks(38,39). Minor complications A small urinary and/or rectal bleeding is expected after prostate biopsy, but is generally self-limited and does not require any intervention. Hematospermia is the most frequent complaint from patients (6.5% to 74.4% of cases), followed by hematuria (up to 14.5% of cases) and rectal bleeding (2.2% of cases). Such complications may persist for up to two weeks, with a progressive decrease in their intensity(40,41). Major complications The rate of severe complications related to transrectal US-guided prostate biopsy is low. Infection, hemorrhage and urinary obstruction are the most common severe complications from such procedure. Hospitalization is required in up to 1.6% of patients(42). Infections related to the procedure or febrile episodes are reported in up to 6.6% of cases, with urosepsis caused by aerobic bacteria in 0.3% of cases(42). In the literature, septicemia caused by anaerobic organisms is reported with low frequency. Prebiopsy antibiotic prophylaxis reduces the rate of urinary tract infection, but some patients are at risk for severe infectious complications independent of the prophylaxis. The main risk factors that are predictive for sepsis include the presence of urethral catheter and diabetes mellitus(43,44). The treatment of urinary infection related to prostate biopsy with oral antibiotics (such as quinolones and sulfamethoxazoletrimethoprim) is generally sufficient, although hospitalization and intravenous antibiotic therapy may be necessary(42,45). Antimicrobial treatment may be altered on the basis of the clinical response and the results of uroculture and antibiogram. Acute bacterial prostatitis is relatively uncommon and is characterized by perineal pain, fever, chills, irritative micturition symptoms (micturition urgency, polacyuria and dysuria) and even acute urinary retention. Such complication must be promptly assessed and treated otherwise there is a risk for progressing to sepsis, development of prostatic abscess and dissemination to adjacent organs such as epididymis and testis(46). Urinary obstruction/retention (including obstruction by clot or secondary to the local postbiopsy inflammatory alterations themselves) is described in 0% to 4.6% of cases(42). The assessment of post micturition residue must be made in symptomatic patients. Therapy with alpha-adrenergic blockers may be initiated in patients with residual urinary volume < 100 ml, while insertion of a low-caliber urethral catheter or cytostomy may be necessary in patients with greater residual volumes. Severe rectal bleeding requiring intervention is a rare complication, occurring in up to 1% of cases(47). The management of patients with significant hemorrhage at the moment of biopsy is described in the algorithm below. In hemodynamically stable patients with active rectal bleeding, manual (digital) compression of the prostate (or compression with the sonographic transducer) is the primary strategy line. A set of gauzes applied to the rectum may be utilized(48). As direct pressure is applied over the prostate, the vital signs of the patient are monitored and the coagulation parameters are verified and corrected as necessary. The rectal insertion of a Foley catheter with an inflated (50 ml) balloon has shown to reduce hemorrhage(49); but the routine use of such technique to prevent bleeding is not supported, since it causes unnecessary discomfort for a borderline benefit. Nevertheless, such technique may be used for temporary management of the bleeding until a resolutive intervention is performed. In case the bleeding remains active or the patient is hemodynamically unstable, an endoscopic intervention (for epinephrine injection or clipping) or surgery (for example, ligature) should be performed(47,50). Any patient with a major complication related to the procedure should be assessed and followed-up by an experienced urologist. 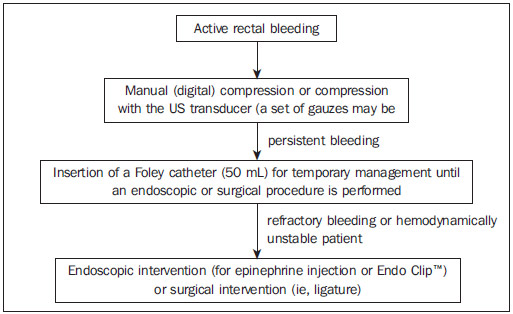 Algorithm for management of active rectal bleeding following prostate biopsy. CONCLUSIONS RRadiologists involved in the performance of transrectal US-guided prostate biopsy should know the complications related to the procedure as well as their management. The guidance on preprocedural preparation is fundamental to reduce the incidence of severe complications. In such a context, antibiotic prophylaxis should be routinely performed. REFERENCES 1. Chojniak R, Pinto PNV, Tyng CJ, et al. Computed tomography-guided transthoracic needle biopsy of pulmonary nodules. Radiol Bras. 2011;44:315-20. 2. Chojniak R, Grigio HR, Bitencourt AGV, et al. Percutaneous computed tomography-guided core needle biopsy of soft tissue tumors: results and correlation with surgical specimen analysis. Radiol Bras. 2012;45:259-62. 3. Ceratti S, Giannini P, Souza RAS, et al. Ultrasound-guided fine-needle aspiration of thyroid nodules: assessment of the ideal number of punctures. Radiol Bras. 2012;45:145-8. 4. Scherr DS, Eastham J, Ohori M, et al. Prostate biopsy techniques and indications: when, where, and how? Semin Urol Oncol. 2002;20:18-31. 5. Smeenge M, de la Rosette JJ, Wijkstra H. Current status of transrectal ultrasound techniques in prostate cancer. Curr Opin Urol. 2012;22:297-302. 6. Dall'Oglio MF, Crippa A, Faria EF, et al. Diretrizes de câncer de próstata. Rio de Janeiro: Sociedade Brasileira de Urologia; 2011. 7. Rocha LCA, Silva EA, Costa RP, et al. Biópsia de próstata - projeto diretrizes. Sociedade Brasileira de Urologia. Rio de Janeiro: Associação Médica Brasileira e Conselho Federal de Medicina; 2006. 8. Puig J, Darnell A, Bermúdez P, et al. Transrectal ultrasound-guided prostate biopsy: is antibiotic prophylaxis necessary? Eur Radiol. 2006;16:939-43. 9. Zani EL, Clark OA, Rodrigues Netto N Jr. Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane Database Syst Rev. 2011;(5):CD006576. 10. Aron M, Rajeev TP, Gupta NP. Antibiotic prophylaxis for transrectal needle biopsy of the prostate: a randomized controlled study. BJU Int. 2000;85:682-5. 11. Muñoz Vélez D, Vicens Vicens A, Ozonas Moragues M. Antibiotic prophylaxis in transrectal prostate biopsy. Actas Urol Esp. 2009;33:853-9. 12. Bootsma AM, Laguna Pes MP, Geerlings SE, et al. Antibiotic prophylaxis in urologic procedures: a systematic review. Eur Urol. 2008;54:1270-86. 13. Lindstedt S, Lindström U, Ljunggren E, et al. Single-dose antibiotic prophylaxis in core prostate biopsy: impact of timing and identification of risk factors. Eur Urol. 2006;50:832-7. 14. Shigemura K, Tanaka K, Yasuda M, et al. Efficacy of 1-day prophylaxis medication with fluoroquinolone for prostate biopsy. World J Urol. 2005;23:356-60. 15. Shandera KC, Thibault GP, Deshon GE Jr. Efficacy of one dose fluoroquinolone before prostate biopsy. Urology. 1998;52:641-3. 16. Hori S, Sengupta A, Joannides A, et al. Changing antibiotic prophylaxis for transrectal ultrasound-guided prostate biopsies: are we putting our patients at risk? BJU Int. 2010;106:1298-302. 17. Steensels D, Slabbaert K, De Wever L, et al. Fluoroquinolone-resistant E. coli in intestinal flora of patients undergoing transrectal ultrasound-guided prostate biopsy - should we reassess our practices for antibiotic prophylaxis? Clin Microbiol Infect. 2012;18:575-81. 18. Zaytoun OM, Anil T, Moussa AS, et al. Morbidity of prostate biopsy after simplified versus complex preparation protocols: assessment of risk factors. Urology. 2011;77:910-4. 19. Carey JM, Korman HJ. Transrectal ultrasound guided biopsy of the prostate. Do enemas decrease clinically significant complications? J Urol. 2001;166:82-5. 20. Giannarini G, Mogorovich A, Valent F, et al. Continuing or discontinuing low-dose aspirin before transrectal prostate biopsy: results of a prospective randomized trial. Urology. 2007;70:501-5. 21. Maan Z, Cutting CW, Patel U, et al. Morbidity of transrectal ultrasonography-guided prostate biopsies in patients after the continued use of low-dose aspirin. BJU Int. 2003;91:798-800. 22. Mukerji G, Munasinghe I, Raza A. A survey of the peri-operative management of urological patients on clopidogrel. Ann R Coll Surg Engl. 2009;91:313-20. 23. El-Hakim A, Moussa S. CUA guidelines on prostate biopsy methodology. Can Urol Assoc J. 2010;4:89-94. 24. Ihezue CU, Smart J, Dewbury KC, et al. Biopsy of the prostate guided by transrectal ultrasound: relation between warfarin use and incidence of bleeding complications. Clin Radiol. 2005;60:459-63. 25. Ghani KR, Rockall AG, Nargund VH, et al. Prostate biopsy: to stop anticoagulation or not? BJU Int. 2006;97:224-5. 26. Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336:1506-11. 27. Irani J, Fournier F, Bon D, et al. Patient tolerance of transrectal ultrasound-guided biopsy of the prostate. Br J Urol. 1997;79:608-10. 28. Yurdakul T, Taspinar B, Kilic O, et al. Topical and long-acting local anesthetic for prostate biopsy: a prospective randomized placebo-controlled study. Urol Int. 2009;83:151-4. 29. Szlauer R, Gotschl R, Gnad A, et al. Comparison of lidocaine suppositories and periprostatic nerve block during transrectal prostate biopsy. Urol Int. 2008;80:253-6. 30. Song SH, Kim JK, Song K, et al. Effectiveness of local anaesthesia techniques in patients undergoing transrectal ultrasound-guided prostate biopsy: a prospective randomized study. Int J Urol. 2006;13:707-10. 31. Barbosa RAG, Silva CD, Torniziello MYT, et al. Estudo comparativo entre três técnicas de anestesia geral para biópsia de próstata dirigida por ultrassonografia transretal. Rev Bras Anestesiol. 2010;60:457-65. 32. Song JH, Doo SW, Yang WJ, et al. Value and safety of midazolam anesthesia during transrectal ultrasound-guided prostate biopsy. Korean J Urol. 2011;52:216-20. 33. Bingqian L, Peihuan L, Yudong W, et al. Intraprostatic local anesthesia with periprostatic nerve block for transrectal ultrasound guided prostate biopsy. J Urol. 2009;182:479-83. 34. Ashley RA, Inman BA, Routh JC, et al. Preventing pain during office biopsy of the prostate: a single center, prospective, double-blind, 3-arm, parallel group, randomized clinical trial. Cancer. 2007;110:1708-14. 35. Kuppusamy S, Faizal N, Quek KF, et al. The efficacy of periprostatic local anaesthetic infiltration in transrectal ultrasound biopsy of prostate: a prospective randomised control study. World J Urol. 2010;28:673-6. 36. Wolfsthal SD. Is blood pressure control necessary before surgery? Med Clin North Am. 1993;77:349-63. 37. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery - executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation. 2002;105:1257-67. 38. Rodríguez LV, Terris MK. Risks and complications of transrectal ultrasound guided prostate needle biopsy: a prospective study and review of the literature. J Urol. 1998;160:2115-20. 39. Djavan B, Waldert M, Zlotta A, et al. Safety and morbidity of first and repeat transrectal ultrasound guided prostate needle biopsies: results of a prospective European prostate cancer detection study. J Urol. 2001;166:856-60. 40. Ecke TH, Gunia S, Bartel P, et al. Complications and risk factors of transrectal ultrasound guided needle biopsies of the prostate evaluated by questionnaire. Urol Oncol. 2008;26:474-8. 41. Loeb S, Carter HB, Berndt SI, et al. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186:1830-4. 42. Chiang IN, Chang SJ, Pu YS, et al. Major complications and associated risk factors of transrectal ultrasound guided prostate needle biopsy: a retrospective study of 1875 cases in Taiwan. J Formos Med Assoc. 2007;106:929-34. 43. Simsir A, Kismali E, Mammadov R, et al. Is it possible to predict sepsis, the most serious complication in prostate biopsy? Urol Int. 2010;84:395-9. 44. Lange D, Zappavigna C, Hamidizadeh R, et al. Bacterial sepsis after prostate biopsy - a new perspective. Urology. 2009;74:1200-5. 45. Lindert KA, Kabalin JN, Terris MK. Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000;164:76-80. 46. Sharp VJ, Takacs EB, Powell CR. Prostatitis: diagnosis and treatment. Am Fam Physician. 2010;82:397-406. 47. Brullet E, Guevara MC, Campo R, et al. Massive rectal bleeding following transrectal ultrasound-guided prostate biopsy. Endoscopy. 2000;32:792-5. 48. Maatman TJ, Bigham D, Stirling B. Simplified management of post-prostate biopsy rectal bleeding. Urology. 2002;60:508. 49. ilciler M, Erdemir F, Demir E, et al. The effect of rectal Foley catheterization on rectal bleeding rates after transrectal ultrasound-guided prostate biopsy. J Vasc Interv Radiol. 2008;19:1344-6. 50. Braun KP, May M, Helke C, et al. Endoscopic therapy of a massive rectal bleeding after prostate biopsy. Int Urol Nephrol. 2007;39:1125-9. 1. Master, Titular in Charge of the Sector of Intervention, Imaging Department, A.C. Camargo Cancer Center, São Paulo, SP, Brazil 2. MDs, Residents, Imaging Department, A.C. Camargo Cancer Center, São Paulo, SP, Brazil 3. PhD, Chairperson of the Imaging Department, A.C. Camargo Cancer Center, São Paulo, SP, Brazil 4. MD, Titular in Charge of the Sector of Ultrasonography, Imaging Department, A.C. Camargo Cancer Center, São Paulo, SP, Brazil Mailing Address: Dr. Chiang Jeng Tyng A. C. Camargo Cancer Center Rua Professor Antônio Prudente, 211, Liberdade São Paulo, SP, Brazil, 01509-010 E-mail: chiangjengtyng@gmail.com Received April 13, 2013. Accepted after revision June 7, 2013. Study developed at A.C. Camargo Cancer Center, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554