Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 5 - Sep. / Oct. of 2013
Vol. 46 nº 5 - Sep. / Oct. of 2013
|
ORIGINAL ARTICLE
|
|
Role of Doppler ultrasonography evaluation of superior mesenteric artery flow volume in the assessment of Crohn's disease activity |
|
|
Autho(rs): Fabiana Paiva Martins1; Eduardo Garcia Vilela2; Maria de Lourdes Abreu Ferrari2; Henrique Osvaldo da Gama Torres2; Juliana Brovini Leite3; Aloísio Sales da Cunha4 |
|
|
Keywords: Doppler ultrasonography; Superior mesenteric artery flow; Crohn's disease; Inflammatory activity. |
|
|
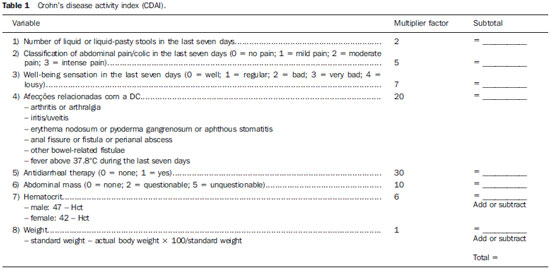
Abstract: INTRODUCTION
Crohn's disease (CD) is a chronic recurrent inflammatory disorder which affects the gastrointestinal tract. Its treatment, although effective in relieving symptoms and in improving the quality of life, is not curative. The evaluation of the inflammatory activity is of paramount importance, as the delay in instituting the treatment may lead to complications. The ideal marker of inflammatory activity at CD is still to be determined. The available clinical indices rely on subjective symptoms such as abdominal pain and well-being sensation, and present poor correlation with endoscopic and histopathological signs of disease activity. Biochemical tests may be more objective, but are not more specific than clinical indices. Endoscopic methods are invasive, costly and time consuming, so their utilization as a routine for all patients is not feasible, particularly in cases where serial examinations are necessary(1,2). Computed tomography enterography has demonstrated to be efficient in the evaluation of inflammatory activity, but, as this method relies on ionizing radiation, its indication is limited in the context of frequent recurrences(3,4). Magnetic resonance enterography provides results comparable to those of computed tomography enterography(1), however it is still scarcely available in our country. Microvascular changes characterized by vascular injuries or infarct are observed in small bowel resection specimens from patients with CD, and vary according to the inflammatory reaction intensity, resulting in neovascularization(5,6), which could also be observed in angiographic studies(7,8), probably reflecting an increase in blood flow to the affected bowel segments. With the publication of studies demonstrating the viability of Doppler ultrasonography (US) for the evaluation of the superior mesenteric artery (SMA) flow(9-11), there has been an increasing interest in the splanchnic hemodynamics evaluation in CD by means of Doppler US, considering its noninvasiveness, safety, low-cost and capability for quantitative analysis. MATERIALS AND METHODS Patients A group of 42 patients previously diagnosed with CD with small bowel involvement, defined according to clinical, endoscopic, radiological, surgical and histopathological(12) criteria, were prospectively evaluated. All the patients originated from the Bowel Clinic of Instituto Alfa de Gastroenterologia - Hospital das Clínicas da Universidade Federal de Minas Gerais (UFMG), recruited between October 2006 and November 2009. The study was approved by the Committee for Ethics in Research of UFMG (ETIC 87/08). All patients signed a term of free and informed consent before their inclusion in the study. The patients were divided into two groups on the basis of the score from the Crohn's disease activity index - CDAI (Table 1) as a reference standard(13): group 1 - comprising patients with CDAI < 150, characterizing disease in remission; group 2 - comprising patients with CDAI > 150, characterizing active disease. Pregnant patients and those with severe coexisting disorders of cardiopulmonary or renal origin were excluded from the study. The patients were clinically evaluated according to the routine of the outpatient clinic and underwent Doppler US before any change of the medical approach. The scans were blindly performed, with the observer being unaware of the patients' clinical history/classification. Once the patients had undergone the scan, their records were reviewed for clinical and laboratory data collection. The patients were classified according to their ages at the time of the diagnosis, site and form of disease according to the Vienna classification(14) (Table 2). 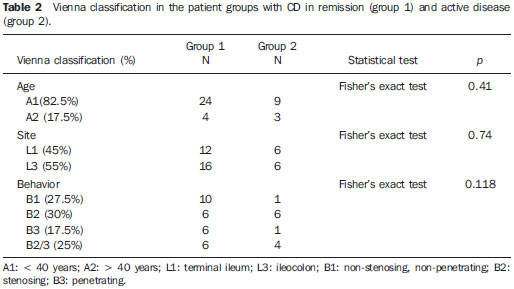 Doppler US of SMA The scans were performed by an experienced radiologist specialized in Doppler US, utilizing a duplex Doppler US ATL 5000 Sono-CT model apparatus (Philips Medical Systems; Best, The Netherlands), equipped with a 2-5 MHz multi-frequency convex transducer. The patients were examined in the morning, after fasting for eight hours. The SMA was sagittal scanned, with high definition zooming and 5 kHz pulse repetition. The Doppler sampling volume was positioned 2-3 cm distally from the vessel origin, before the emergence of its branches and adjusted to comprise the vascular lumen, but without touching its walls. A spectrum of at least five cardiac cycles was obtained during breath hold, and the mean flow velocity was automatically determined by the equipment. The insonation angle was determined on the real time B-mode image and always maintained below 60º. The measurement of the SMA diameter was utilized by the equipment for determining the vessel area and automatically calculating the SMA flow volume (Figure 1). With the objective of reducing random errors, each measurement was repeated for three times, and the mean value was considered as the final result(15). 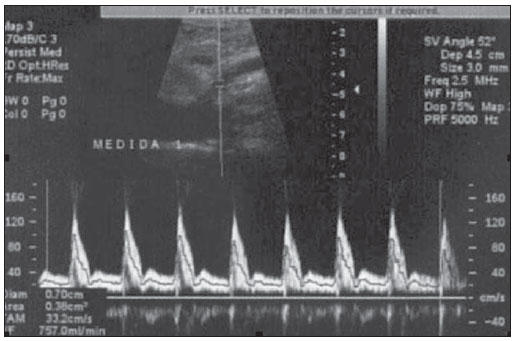 Figure 1. Spectrum of superior mesenteric artery flow at Doppler US in patient with active Crohn's disease. After Doppler US, the patients were submitted to total abdominal US studies, with special attention to the evaluation of thickening of small bowel walls (> 4 mm) and to the presence of fistulas and abscesses.(16,17) Statistical analysis The comparison between the two groups was carried out with the by utilizing the chi-squared test and the Fisher's exact test for dichotomous variables and the Student's t-test for continuous variables. The considered significance level was 5% (p < 0.05). The evaluation of the test performance for characterization of inflammatory activity in CD was carried out by obtaining the receiver operating characteristic curve (ROC) and selection of a cutoff point, with determination of sensitivity, specificity, positive and negative predictive values in relation to the reference standard. RESULTS Two patients were excluded from the analysis for not presenting with satisfactory technical conditions to be submitted to Doppler US of SMA, because of excessive abdominal distension. Thus, group 1 comprised 28 patients (70%) with CD in remission, and group 2 comprised 12 patients (30%) with active disease evaluated according to the CDAI score. Abdominal US demonstrated alterations characterized by ileum wall thickening, presence of entero-enteral fistula and cavitary collection in 16 patients (40%), which were the changes most frequently observed in group 2 (p = 0.037). On average, the SMA flow volume was significantly greater in group 2 (626 ml/min ± 236) as compared with group 1 (376 ml/min ± 190), with p = 0.001 (Figure 2). 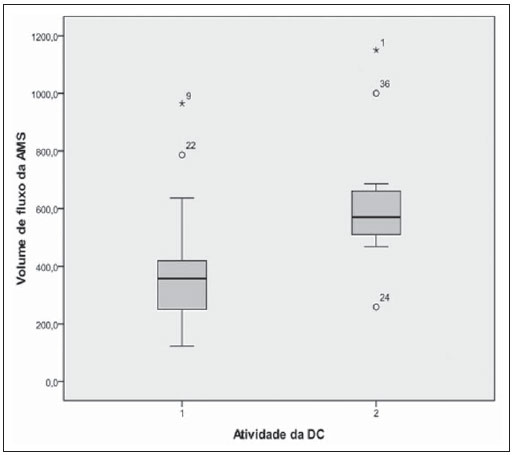 Figure 2. Boxplot of the comparison of the SMA flow volume in patients with CD in remission (group 1) and in activity (group 2). The area under the ROC curve for the SMA flow volume was 0.833 (p = 0.001). The value of 500 ml/min was adopted as the cutoff point, since such value is considered in literature as the upper limit of normality for healthy individuals18-20) and is also utilized for evaluation of the test performance. In the present study, the measurement of the SMA flow volume at Doppler US presented a sensitivity of 83% and specificity of 82% for the diagnosis of inflammatory activity. There was also statistically significant association between altered result of SMA flow volume measurement and the presence of inflammatory activity in CD (p = 0.0001). DISCUSSION The presence of hemodynamic changes in patients with CD has already been previously demonstrated by angiography(7,8) and studies with radionuclides(21), characterized by a hyperdynamic state, probably caused by vascular congestion, stasis and neovascularization. From the physiopathological point-of-view, it would be reasonable to assume that such changes imply an increase in the SMA flow volume at Doppler US, a hypothesis already admitted in other studies. Although some authors assert that results in the literature are conflicting as regards the association between changes observed at Doppler US of SMA and presence of inflammatory activity in CD(22,23), the present study authors believe that such discrepancies are mostly due to crucial differences in the utilized method, notably in the parameters adopted for Doppler US of SMA. Undoubtedly, among the already evaluated parameters, the SMA flow volume stands out as that with best correlation with inflammatory activity(24,25). As previously observed by other authors(24-26), the present study demonstrates that patients with active CD presented significantly greater SMA flow volume than patients with disease in remission. Additionally, as the value of 500 ml/min is considered as the cutoff point, the authors of the present study observed sensitivity of 83% and specificity of 82% in the diagnosis of inflammatory activity, values which are similar to those reported by other studies. Some authors(25,27) question the usefulness of the SMA flow volume measurement for characterizing inflammatory activity in CD, even after finding significant association between increased flow and clinical and laboratory signs of activity, due to the existence of an overlapping range of flow volume values between the patients with active CD and patients with the disease in remission, close to the cutoff point of 500 ml/min. Such range was observed by van Oostayen et al.(28,29) and defined as a "gray zone" of values between 450 and 600 ml/min, where the test would be less useful. In the present study, the authors observed seven patients with the flow volume within such "gray zone" of values. One might assume that patients presenting with less intense inflammatory activity or those who normally have a greater flow volume would be in such zone; it is important to remind that CDAI, although being widely utilized, presents many limitations in the evaluation of inflammatory activity(13). In the present study, there were two patients with false-negative results. One of them had a CDAI score of 180 and flow volume of 469 ml/min (therefore within the "gray zone") and had been previously submitted to partial ileocolic enterectomy, which can explain the absence of increased SMA flow volume. The other patient had a CDAI score of 206 and the flow volume of 259 ml/min; despite the absence of an explanation for such a discrepancy, the patient presented normal C-reactive protein levels, a fact which allows the authors to assume that perhaps the increased CDAI might result from subjective symptoms and not related to inflammatory activity, an influence which is recognized in the literature(13). The main limitation of the present study was the sample size, which led to wide confidence intervals in the measurement of the test performance. Additionally, further studies with prospective evaluation of patients before and after treatment may be useful to elucidate some of the assumptions raised in the discussion. CONCLUSION The mean values for SMA flow volume where higher in patients with active CD, and a statistically significant association was observed between the altered results of the test and the inflammatory activity evaluated by the CDAI score. Because of its noninvasiveness, safety and low-cost, Doppler US of SMA can be useful in the evaluation of the inflammatory activity in patients with CD. Acknowledgements The authors wish to thank Instituto Hermes Pardini, for having provided the facilities for performing SMA Doppler US studies at no cost to patients and investigators. REFERENCES 1. Vilela EG, Torres HOG, Martins FP, et al. Evaluation of inflammatory activity in Crohn's disease and ulcerative colitis. World J Gastroenterol. 2012;18:872-81. 2. Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007;133:1670-89. 3. Booya F, Fletcher JG, Huprich JE, et al. Active Crohn disease: CT findings and interobserver agreement for enteric phase CT enterography. Radiology. 2006;241:787-95. 4. Jaffe TA, Gaca AM, Delaney S, et al. Radiation doses from small-bowel follow-through and abdominopelvic MDTC in Crohn's disease. AJR Am J Roentgenol. 2007;189:1015-22. 5. Brahme F, Lindstöm C. A comparative radiographic and pathological study of intestinal vasoarchitecture in Crohn's disease and in ulcerative colitis. Gut. 1970;11:928-40. 6. Wakefield AJ, Sawyerr AM, Dhillon AP, et al. Pathogenesis of Crohn's disease: multifocal gastrointestinal infarction. Lancet. 1989;2:1057-62. 7. Boijsen E, Reuter SR. Mesenteric angiography in the evaluation of inflammatory and neoplastic disease of the intestine. Radiology. 1966;87:1028-36. 8. Lunderquist A, Knutsson H. Angiography in Crohn's disease of the small bowel and colon. Am J Roentgenol Radium Ther Nucl Med. 1967;101:338-44. 9. Jäger K, Bollinger A, Valli C, et al. Measurement of mesenteric blood flow by duplex scanning. J Vasc Surg. 1986;3:462-9. 10. Moneta GL, Taylor DC, Helton WS, et al. Duplex ultrasound measurement of postprandial intestinal blood flow: effect of meal composition. Gastroenterology. 1988;95:1294-301. 11. Sato S, Ohnishi K, Sugita S, et al. Splenic artery and superior mesenteric artery blood flow: non-surgical Doppler US measurement in healthy subjects and patients with chronic liver disease. Radiology. 1987;164:347-52. 12. Gollop JH, Phillips SF, Melton LJ 3rd, et al. Epidemiologic aspects of Crohn's disease: a population based study in Olmsted county, Minnesota, 1943-1982. Gut. 1988;29:49-56. 13. Best WR, Becktel JM, Singleton JW, et al. Development of Crohn's disease activity index. Gastroenterology. 1976;70:439-44. 14. Gasche C, Scholmerich J, Brinskov J, et al. A simple classification of Crohn's disease: report of the Working Party for the World Congress of Gastroenterology, Vienna 1998. Inflam Bowel Dis. 2000;6:8-15. 15. Perko MJ, Just S. Duplex ultrasound of superior mesenteric artery: interobserver variability. J Ultrasound Med. 1993;12:259-63. 16. Maconi G, Radice E, Greco S, et al. Bowel ultrasound in Crohn's disease. Best Pract Res Clin Gastroenterol. 2006;20:93-112. 17. Tarján Z, Tóth G, Györke T, et al. Ultrasound in Crohn's disease of the small bowel. Eur J Radiol. 2000;35:176-82. 18. Cooper AM, Braatvedt GD, Qamar MI, et al. Fasting and postprandial splanchnic blood flow is reduced by a somatostatin analogue (octreotide) in man. Clin Sci. 1991;81:168-75. 19. Qamar MI, Read AE, Skidmore R, et al. Transcutaneous Doppler ultrasound measurement of superior mesenteric artery blood flow in man. Gut. 1986;27:100-5. 20. Nakamura T, Moriyasu F, Ban N, et al. Quantitative measurement of abdominal arterial blood flow using image-directed Doppler ultrasonography: superior mesenteric, splenic and common hepatic arterial blood flow in normal adults. J Clin Ultrasound. 1989;17:261-8. 21. Giaffer MH, Tindale WB, Senior S, et al. Quantification of disease activity in Crohn's disease by computer analysis of Tc-99m hexamethyl propylene amine oxime (HMPAO) labeled leucocyte images. Gut. 1993;34:68-74. 22. Maconi G, Parente F, Bollani S, et al. Factors affecting splanchnic haemodynamics in Crohn's disease: a prospective controlled study using Doppler ultrasound. Gut. 1998;43:645-50. 23. Maconi G, Parente F, Bollani S, et al. Abdominal ultrasound in the assessment of extent and activity of Crohn's disease: clinical significance and implication of bowel wall thickening. Am J Gastroenterol, 1996;91:1604-9. 24. van Oostayen JA, Wasser MN, van Hogezand RA, et al. Activity of Crohn disease assessed by measurement of superior mesenteric artery flow with Doppler US. Radiology. 1994;193:551-4. 25. Byrne MF, Farrell MA, Abass S, et al. Assessment of Crohn's disease activity by Doppler sonography of the superior mesenteric artery, clinical evaluation and the Crohn's disease activity index: a prospective study. Clin Radiol. 2001;56:973-8. 26. Erden A, Cuhmur T, Ölçer T. Superior mesenteric artery Doppler waveform changes in response to inflammation of the ileocecal region. Abdom Imaging. 1997;22:483-6. 27. Sjekavica I, Barbaric-Babic V, Krznaric Z, et al. Assessment of Crohn's disease activity by Doppler ultrasound of superior mesenteric artery and mural arteries in thickened bowel wall: cross-sectional study. Croat Med J. 2007;48:822-30. 28. van Oostayen JA, Wasser MNJM, van Hogezand RA, et al. Doppler sonography evaluation of superior mesenteric artery flow to assess Crohn's disease activity: correlation with clinical evaluation, Crohn's disease activity index, and alpha-1-antitrypsin clearance in feces. AJR Am J Roentgenol. 1997;168:429-43. 29. van Oostayen JA, Wasser MN, Griffioen G, et al. Activity of Crohn's disease assessed by measurement of superior mesenteric artery flow with Doppler ultrasound. Neth J Med. 1998;53:S3-8. 1. Master, Assistant Professor, Department of Anatomy and Imaging, School of Medicine of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil 2. PhDs, Associate Professors, Department of Medical Practice, School of Medicine of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil 3. Master, Biochemist, Hospital e Maternidade Terezinha de Jesus, Juiz de Gora, MG, Brazil 4. Private Docent, Titular Professor of Medical Practice at School of Medicine, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil Mailing Address: Dra. Fabiana Paiva Martins Avenida Professor Alfredo Balena, 189/803, Centro Belo Horizonte, MG, Brazil, 30130-100 E-mail: fabpaivamartins@gmail.com Received August 28, 2012. Accepted after revision July 1st, 2013. Study developed at the School of Medicine, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554