Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 4 - July / Aug. of 2013
Vol. 46 nº 4 - July / Aug. of 2013
|
CASE REPORT
|
|
Frontal sinus pneumocele: case report and literature review |
|
|
Autho(rs): Ana Célia Baptista Koifman1; Lívio de Oliveira Ferraz2; Bernardo Teixeira Blanco2; Luiz Eugênio Bustamante Prota Filho2 |
|
|
Keywords: Pneumocele; Frontal sinus; Computed tomography. |
|
|
Abstract: INTRODUCTION
The imaging evaluation of paranasal sinuses has been approached by a range of publications in the Brazilian radiological literature(1–4). Pneumocele is a rare, slow growing condition affecting the paranasal sinuses, most commonly the frontal sinus, and less frequently the maxillary sinus(5). Such disease is characterized by an abnormal, focal or generalized, single or multiple dilatation of the sinusal cavity, with bone wall thinning or erosion(6,7). The etiology still remains unknown, but several causes have been proposed as follows: spontaneous drainage of mucocele; presence of gas-producing microorganisms; post-traumatic involvement; benign and malignant neoplasias; hormonal abnormalities; congenital factors and osteomeatal complex function as an unidirectional valve(5,6,8,9). The patients may be asymptomatic or present with a range of clinical signs, most of times depending on the mass effect resulting from the paranasal cavity enlargement. Computed tomography (CT) is the method of choice in such cases, since it can easily confirm the presence of this condition. CASE REPORT A female, 26-year-old student was admitted to the hospital emergency department, complaining of a brownish, thick and fetid discharge through her right nasal fossa for some hours. The patient reported repetition rhinosinusitis for a long time, sometimes associated with headache, discomfort and swelling in the right eye area. At clinical examination, a small bulging was observed in the right supraorbital region. The patient underwent paranasal sinuses computed tomography in a Brilliance 6-slice apparatus (Philips Medical System; Best, The Netherlands), with 1 mm-thick slices, 120 kV, 180 mA, and multiplanar reformation, which demonstrated hyperaeration of the frontal sinus at right, beyond the usual anatomical limits, in association with thinning and erosion of the frontal sinus posterior wall and extensive defect of the ipsilateral orbital plate of the frontal bone (Figures 1 to 4). The patients did not report any previous facial surgery or trauma.  Figure 1. Cranial CT scan, lateral view. Extensive pneumatization of the frontal sinus. 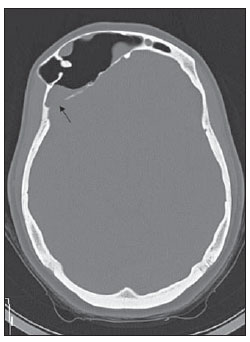 Figure 2. Axial CT, bone window. Abnormal pneumatization of the frontal sinus at right, beyond the normal anatomical limits, in association with thinning and erosion (arrow) of the posterior sinus wall. Note the presence of material within the cavity. 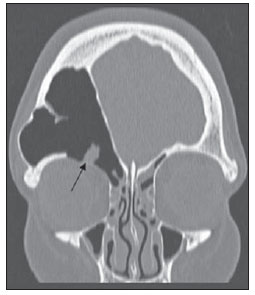 Figure 3. Coronal CT, bone window. Extensive erosion (arrow) of the orbital plate of the frontal bone at right.  Figure 4. Coronal CT, soft-tissue window. Presence of material with soft parts density in the frontal sinus at right. DISCUSSION The term pneumocele is many times utilized as a synonym for hypersinus, aerocele, pneumosinus dilatans and air cyst(10). According to the classification developed by Urken et al.(6), paranasal sinuses dilatation may be classified into three types, namely, sinus hyperpneumatization, pneumosinus dilatans and pneumocele. Hyperpneumatization is characterized by sinus enlargement within the usual anatomical limits. Pneumosinus dilatans consists in sinus enlargement beyond the normal anatomical limits, while the bone walls of the sinus remain normal. Pneumocele corresponds to an abnormal enlargement of the paranasal sinus with bone walls thinning or erosion(6). The clinical presentation is sinus-dependent and varied, including headache, proptosis, nasal obstruction, Eustachian tube obstruction, sinusitis, pain and pressure on the affected paranasal sinus, facial deformity, otalgia, diplopia and decreased visual acuity(5,9,11,12). Pneumocele has been associated with some conditions such as trauma, respiratory hamartomas, spontaneous pneumocephalus, affecting equally men and women(8,9,12). CT is the method of choice and is sufficient for the diagnosis of this condition. Because of the variety of etiologies, the treatment is individualized, but sinus decompression is recommended in many circumstances(5,9,12). In the present case, the patient presented right-sided sinusal and orbital signs for a long time, associated with ipsilateral frontal sinus pneumocele and with extensive communication between the sinus and the orbit. The patient did not report any previous meningitis or cerebral infection, despite the presence of communication between the frontal sinus and the cranial fossa caused by the posterior sinus wall erosion. The brownish secretion discharge reported by the patient suggests a chronic material retention either in association or not with underlying mucocele and/or superimposed fungal infection. The patient has been undergoing immunotherapy on an irregular basis and, until the publication of the present case report, she had not been submitted to any surgical intervention, by her own decision. The rarity of the condition and the paucity of studies in the radiological literature confirm the relevance of the knowledge on this abnormality by radiologists, corroborating the critical role of CT in the diagnosis of the lesion. REFERENCES 1. Agnollitto PM, Nogueira-Barbosa MH. Síndrome de Gardner [Qual o seu diagnóstico?]. Radiol Bras. 2012;45(4):xi–xii. 2. Holanda MMA, Rocha AB, Santos RHP, et al. Encefalocele basal esfenoetmoidal associada a fissura labiopalatina mediana: relato de caso. Radiol Bras. 2011;44:399–400. 3. Gonçalves FG, Jovem CL, Moura LO. Tomografia computadorizada das células etmoidais intra e extramurais: ensaio iconográfico. Radiol Bras. 2011;44:321–6. 4. Miranda CMNR, Maranhão CPM, Arraes FMNR, et al. Variações anatômicas das cavidades paranasais à tomografia computadorizada multislice: o que procurar? Radiol Bras. 2011;44:256–62. 5. Mauri M, Oliveira CO, Krumenauer RCP, et al. Pneumosinus dilatans: uma doença de etiologia variada. Braz J Otorhinolaryngol. 1999;65:529–33. 6. Urken ML, Som PM, Lawson W, et al. Abnormally large frontal sinus. II. Nomenclature, pathology, and symptoms. Laryngoscope. 1987;97:606–11. 7. Kiroglu Y, Karabulut N, Sabir NA, et al. Pneumosinus dilatans and multiplex: report of three rare cases and review of the literature. Dentomaxillofac Radiol. 2007;36:298–303. 8. Gu Z, Cao Z. Frontal sinus pneumocele associated with respiratory epithelial adenomatoid hamartoma and nasal polyps. Otolaryngol Head Neck Surg. 2012;147:177–8. 9. Karadag D, Calisir C, Adapinar B. Post-traumatic pneumocele of the frontal sinus. Korean J Radiol. 2008;9:379–81. 10. Teh BM, Hall C, Chan SW. Pneumosinus dilatans, pneumocele or air cyst? A case report and literature review. J Laryngol Otol. 2012;126:88–93. 11. Abdel-Aal AK, Abayazeed AH, Raghuram K, et al. Pneumocele of the frontal sinus producing orbital roof defect: case report and review of literature. Am J Otolaryngol. 2010;31:202–4. 12. Park CY, Kim KS. Spontaneous pneumocephalus associated with pneumocele of the frontal sinus. Cephalalgia. 2010;30:1400–2. 1. Private Docent, Associate Professor of Radiology, Universidade Federal do Estado do Rio de Janeiro (UNIRIO), Rio de Janeiro, RJ, Brazil 2. Graduate Students of Medicine, Universidade Federal do Estado do Rio de Janeiro (UNIRIO), Rio de Janeiro, RJ, Brazil Mailing Address: Dra. Ana Célia Baptista Koifman Rua João Lira, 143/701, Leblon Rio de Janeiro, RJ, Brazil, 22430-210 E-mail: anaceliak@gmail.com Received September 13, 2012. Accepted after revision March 27, 2013. * Study developed at Universidade Federal do Estado do Rio de Janeiro (UNIRIO), Rio de Janeiro, RJ, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554