Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 4 - July / Aug. of 2013
Vol. 46 nº 4 - July / Aug. of 2013
|
ORIGINAL ARTICLE
|
|
Prevalence of simple liver cysts and hemangiomas in cirrhotic and non-cirrhotic patients submitted to magnetic resonance imaging |
|
|
Autho(rs): Breno Victor Tomaz Galvão1; Lucas Rios Torres2; Patrícia Prando Cardia2; Thiago Franchi Nunes2; Priscila Silveira Salvadori1; Giuseppe D'Ippolito3 |
|
|
Keywords: Hemangioma; Cysts; Magnetic resonance imaging; Prevalence; Liver. |
|
|
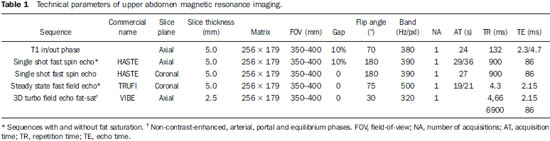
Abstract: INTRODUCTION
The number of magnetic resonance imaging (MRI) studies has increased over the past few years, both because of the wider availability of the method and because of the increase in the number of applications in different clinical settings. Such phenomenon contributes to the increased detection of incidental focal liver lesions (FLLs), also called incidentalomas. The term "incidentaloma" is reserved to the type of lesion not related to the clinical suspicion or to the signs and symptoms presented by the patient(1). Because of its frequency, special attention has been paid to such type of lesion in the literature, leading medical societies to develop consensus and treatment and follow-up protocols(2). As regards liver incidentalomas, cysts and hemangiomas are most frequently found. Although in most cases the diagnosis of such lesions, as well as the determination of their benign nature by means of the available imaging methods are performed with no major difficulties, their prevalence at imaging studies in the general population is still to be accurately estimated. The references utilized in most studies on the theme rely on autopsy studies or surgical series including quite divergent data, ranging from 0.4% to 20% for hemangiomas and from 1% to 14% for simple cysts, with such data sometimes having been acquired several decades ago(3–5). Furthermore, the increase in the number of cirrhotic patients, either for viral or toxic causes, has led to the increase in the number of screening investigations(6). For these patients, the differentiation between benign and malignant lesions is crucial to determine the therapeutic approach. For that reason, a system for the characterization of hepatic lesions, called LI-RADS®, was recently developed(7). Some recent studies have attempted to establish the frequency of pancreatic cysts incidentally found at MRI(8), but there is a necessity of similar studies approaching the detection of FLLs. A theme that has been widely discussed in the literature, generating some controversy is related to the frequency of hemangiomas in cirrhotic livers, which would be lower than that in the general population(9–11). MRI is considered to be a highly sensitive and specific method for the diagnosis of hepatic cysts and hemangiomas(9). The possibility of acquiring images in different planes, the high contrast between soft tissue structures and the analysis of the vascular behavior of lesions and surrounding organs potentialize its utilization as a diagnostic tool optimized with the adoption of new techniques and sequences(12–15), thus improving the capability of the method to detect and characterize focal lesions. For these reasons, the prevalence of FLLs identified at MRI could be higher than the previously observed prevalence. Based on such considerations, the present study was proposed in order to provide updated data on the frequency of cysts and hemangiomas incidentally found at MRI both on cirrhotic and non-cirrhotic patients. MATERIALAS AND METHODS Population A retrospective, cross-sectional and observational study was undertaken by means of survey on the digital Picture Archiving and Communication System – PACS (Synapse®; FujiFilm, USA) of all patients who had undergone upper abdomen MRI in the period between February 1st' and July 10, 2011, comprising a total of 363 patients. Exclusion criteria were the following: patients under the age of 18, indication for investigation of hepatic nodules in non-oncologic cases, images considered technically unsatisfactory, and images acquired under directed protocols which did not comprise the whole liver parenchyma (adrenal and MRI urography, for example). The final study sample included 303 patients (187 women and 116 men), with mean age of 53.3 years (± 16.5 years), 57 of them with cirrhosis. The patients were considered cirrhotic in the presence of a combination of clinical/laboratory findings (for example: esophageal varices, splenomegaly, thrombocytopenia, increased bilirubin and liver enzymes levels), with imaging findings (37 patients), or with percutaneous biopsy findings (20 patients). The patients' clinical data were collected from the digital records system of the institution, comprising information on visits, previous imaging studies, laboratory tests results and surgical data, if available. The clinical indications for the reviewed studies varied, with the most common being evaluation of obstructive bile duct diseases and cancer staging. The application of a term of free and informed consent was waived, according instructions and approval by the Committee for Ethics in Research of the institution (CEP 1067/11). Imaging technique All patients were submitted to upper abdomen MRI according the institution's standard protocol, in an Magnetom Sonata Maestro Class® equipment operating with a 1.5 tesla high magnetic field (Siemens; Erlangen, Germany), with synergy coil and with breath hold technique. T1-weighted in-phase and out-phase, gradient-echo sequences were acquired as follows: single shot fast spin echo (HASTE®); steady state fast field echo (TRUFI®); and 3D turbo field echo fat-sat (VIBE®), before and after contrast medium injection (0.5 mmol/ml gadoteric acid – Dotarem®, Guerbet), on arterial, portal and equilibrium phases (respectively 30, 60 and 180 seconds after the intravenous contrast medium injection) at an infusion rate of 2.0 ml/s and dose of 0.2 ml/kg. The technical parameters of the sequences are represented on Table 1. Images interpretation The acquired images were available for visualization on a digital workstation (Synapse®; FujiFilm, USA), where they were consensually evaluated by two radiologists, among the five radiologists who comprised the observers team, with experience in radiology ranging from 2 to 20 years. In the cases where more than one study from a single patient was available over the studied period, only the most recent one was considered. The observers actively sought for liver hemangiomas and simple hepatic cysts with characteristic features, as widely described in the literature(8–10). Thus, hemangiomas were those nodules with hyper-signal on T2-weighted images with long echo time (TE > 130 ms) and with globuliform, discontinuous, progressive and centripetal enhancement (progressive type) or with fast, early and persistent enhancement (flash-filling type)(9,10), and simple cysts, those homogeneous nodules hypointense on T1-weighted and hyperintense on T2-weighted, with a thin capsule, without septa, vegetations or enhancement areas after intravenous paramagnetic contrast medium injection(8). Focal lesions of undetermined nature or of other natures were not taken into consideration. The measurement of the largest axial diameter of the lesion was made on the sequence with highest conspicuity. The number and location of lesions were defined, as well as the enhancement pattern for the hemangiomas (progressive or flash-filling) (Figures 1 and 2)(10). In cases of more than five lesions in a single patient, only the largest five lesions were considered. Patients with innumerable small cysts (< 1.5 cm) widely disseminated throughout the parenchyma and with appearance suggestive of biliary hamartomas, were not included in the study sample. 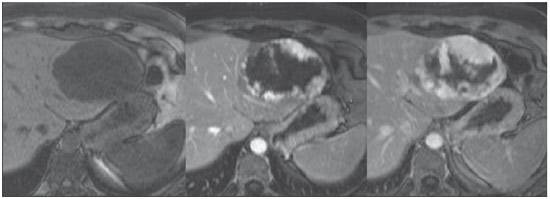 Figure 1. Hepatic hemangioma with progressive enhancement pattern. 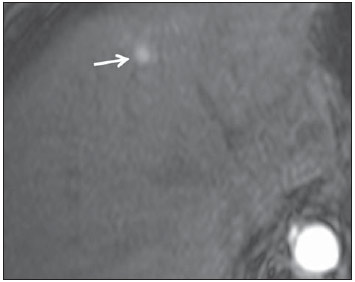 Figure 2. Hepatic hemangioma with flash-filling enhancement pattern. The liver lesions were characterized according to their imaging features as simple cysts, typical hemangiomas and solid nodules, including in the latter group any lesion which did not meet the criteria for the two first groups. The cysts which were considered atypical(16) were not included in any of the groups. Additionally, those patients with cirrhotic liver features were also categorized following the criteria widely adopted in literature(6,17). Statistical analysis The associations between qualitative variables (gender, type of hemangioma enhancement and presence or absence of liver cirrhosis) were made by means of the chi-squared test (χ2). For the quantitative variables (patients' age and lesion dimensions) parametric tests were utilized whenever normal distribution was observed, and non-parametric tests whenever normal distribution was not observed. The comparison of quantitative variables between the several groups was made by means of the t test in the case of two groups, or by variance analysis in the case of more than two groups. In the case of significant variance analysis, a multiple comparisons test was subsequently applied (Turkey's test). The adopted significance level was 5% and the statistical tests were carried out by means of the SPSS 11.0 software. RESULTS Hepatic cysts Among all individuals, 44 had 95 hepatic cysts, making up a prevalence of 14.5% in the studied population (in 10 cirrhotic and 34 non-cirrhotic patients). Out the total of 44 patients with cysts, 23 presented single cysts, while 21 patients presented multiple cysts. The most commonly affected hepatic segments were the IVa (23%) and VI (17%) segments. The mean cyst size was 1.0 cm (ranging from 0.2 cm to 8.8 cm). Out the total of 95 cysts, 66 were < 1.0 cm. As the prevalence of simple hepatic cysts in the cirrhotic population was determined (10/57; 17.5%) and compared with the prevalence in the non-cirrhotic population (34/246; 13.8%) no statistically significant difference was observed (p = 0.472). The dimensions and distribution of the cysts in these two populations did not present any statistically significant difference either. No difference was observed in the prevalence of hepatic cysts with respect to gender and age. Hemangiomas In the present study, 47 hemangiomas were detected in 26 patients (prevalence of 8.6%), 7 of them cirrhotic, while 19 were non-cirrhotic. Out of the total of 26 patients with hemangiomas, 17 had single hemangiomas, while 9 had multiple hemangiomas. The most commonly affected hepatic segments were the VI segment (21%) and II segment (19%), and the mean diameter of the hemangiomas was 2.13 cm (ranging from 0.4 cm to 13.5 cm), with no statistically significant difference between the group of cirrhotic patients (2.51 cm) and the non-cirrhotic group (2.05 cm). The most common enhancement pattern was the progressive type, with a frequency of 89.4%, and the flash-filling pattern was observed in only 10.6% of the hemangiomas in the sample. In only two patients out of the total of 26 patients with hemangiomas, the coexistence of two enhancement patterns was observed (one patient had two hemangiomas, one of each type, and the other had five hemangiomas, with only one with the flash-filling enhancement pattern. No statistically significant difference was observed in the prevalence of hepatic hemangiomas among cirrhotic (5/57; 8.8%) and non-cirrhotic patients (21/246; 8.5%), with p = 0.954. The same was observed for the dimensions, distribution and enhancement pattern of such lesions. Patients' age and gender did not influence the prevalence of hepatic hemangiomas in the study sample, i.e., the presence or absence of hemangiomas was not associated with patients' gender (χ2 = 0.695; p = 0.659; nonsignificant), occurring in 8% of the women and in 9.5% of the men. Mean sizes of the hemangiomas in women and in men were, respectively, 2.29 cm and 1.75 cm. DISCUSSION Cysts and hemangiomas are the most common benign focal hepatic lesions(18). Simple hepatic cysts may be either congenital or acquired and are related to developmental anomalies and/or conformation of the biliary tree(19). Abdominal traumas determining bile extravasation outside of the biliary tree have been regarded as a plausible cause of hepatic cysts(20). At MRI, the cysts are seen as well-defined lesions with hypersignal on T2-weighted sequences and hyposignal on T1-weighted sequences. Depending upon the presence of hemorrhage, there may be variation in signal intensity. No enhancement is observed after paramagnetic contrast medium injection(16). Reports in the literature indicate that the prevalence and number of cysts increase with age because of obstruction and biliary stasis in small biliary ducts(21). An Australian study evaluating obstetric ultrasonography images over a period of more than 10 years has found only three hepatic cysts in fetuses(22). There is a reported predominance in female individuals, with a ratio ranging between 1.5:1 and 5.5:1(23). The data in the present study, however, do not demonstrate any relationship between age or gender and the occurrence of cysts. The first reports on prevalence of simple hepatic cysts were observed in autopsy studies. In a series of 20,000 autopsies, a prevalence of 0.14% (28 cysts)(24) was found. Other similar studies have reported values of 0.17% and 0.53%(25,26). More recent data derived from imaging studies reveal slightly higher values. In 1989, an European study about the prevalence at ultrasonography recorded a prevalence of 2.5% (43 cases in a total of 1,695 patients)(27). Another study, in 1993, found 755 patients with hepatic cysts in a total of 26,000 sonographic images, corresponding to a prevalence of 2.9%(28). On the other hand, such prevalence may reach 5%-14%, as demonstrated in at least one publication(29). A tomographic series developed in 2003 points out a simple hepatic cyst prevalence of 18% in 617 patients(30). More recent studies focused on the therapeutic approach for such lesions report values ranging from 0.1% to 7%, frequently making reference to decades-old data(31,32). There is no report in the literature about the prevalence of hepatic cysts found at MRI. The results in the present study (14.5%) demonstrate a higher prevalence than the average found in previous studies, but similar to the prevalence in the studies which relied on computed tomography(30), supposedly related to the high detection capability of these diagnostic methods. Patients with biliary hamartomas were not included in the present study, as the authors understand that such entities are different from hepatic cysts(29). However, on the 363 MRI studies initially evaluated, no case resembling imaging findings suggestive of biliary hamartomas was observed. Hemangiomas correspond to vascular spaces filled with slow flowing blood. They present hypersignal at T2-weighted sequences, which demonstrates to become more conspicuous as the echo time of the sequences increases, because of the decrease in signal from the surrounding hepatic parenchyma(33,34). Three enhancement patters can be observed after contrast agent injection(34). The first pattern refers to lesions with intense enhancement at the earlier phases, which remains unchanged at delayed phases, and is called flash-filling. The second pattern is the most common one, and is characterized by peripheral, discontinued and progressive enhancement. The third pattern comprises the lesions with progressive enhancement, however with their center persistently without enhancement. Like other authors(10), the authors of the present study have opted for grouping the second and third patterns into a single group for the purpose of calculations. A clear predominance of the progressive pattern over the flash-filling pattern was observed (89.4% versus 10.6%). The classical enhancement pattern associated with its chronological stability has been utilized as a reference standard in the determination of such diagnosis(10,35) and this was the utilized strategy to define the typical hemangiomas found in the present sample. The references cited by authors who describe the prevalence of hemangiomas commonly refer to decades-old studies either with autopsy or surgical series. For example, a 1999 study reported that in 508 hepatectomies in cirrhotic individuals only 9 hemangiomas were found, corresponding to a prevalence of 1.7%(11). In 1997, another study found a prevalence of 1.2% in a series of 596 autopsies(3). Higher values are reported by a 1986 study(4), and like the references cited by Semelka et al. in 1997 reach 20%(36). Finally, some studies still rely on decades-old references, such as a 1958 North-American atlas, which points out a prevalence of hemangiomas in 0.4% of the individuals(37). Although this is not a population study, no previous attempts have been made to establish the prevalence of such lesions by means of MRI. The wide variation in data presented in the literature – from 0.4% to 20% for hemangiomas, and from 0.1% to 18% for simple cysts –, in association with the attention that has been devoted to incidental liver lesions have motivated the authors to seek more updated data utilizing modern and noninvasive diagnostic tools. The results from the present study allow the conclusion that the frequency of cysts and hemangiomas found at MRI is high and above that observed in autopsy studies, perhaps because of the diligent survey for such findings at MRI and because of the facility in characterizing such type of lesion. Because of vascular alterations observed in cases of chronic liver disease, one has suggested that, in such patients, there might be differences in the presentation of hepatic hemangiomas(10,38). Reports have suggested that hemangiomas could degenerate and decrease in size as cirrhosis progresses(11,39). On the other hand, at least one study has demonstrated that size, number, location and enhancement pattern of hemangiomas are not different in cirrhotic patients(10). Similarly, in the present study, no difference was observed in relation to frequency or presentation of hemangiomas in cirrhotic and non-cirrhotic livers. Additionally, it was suggested that supposed alterations of hemangiomas in cirrhotic patients might decrease their detect-ability and, therefore, reduce their prevalence at imaging studies(9,11). The present study results, however, contradict such a possibility, demonstrating similar prevalence in both groups. Although hemangiomas and hepatic cysts are easily diagnosed and differentiated from other liver lesions at ultrasonography, computed tomography and MRI, it is known that small hepatocarcinomas may present homogeneous and early enhancement similar to the flash-filling pattern which may occur in some hemangiomas(40,41) and like in approximately 10% of the present study sample. The main limitation in the present study lies in the inclusion criteria of the sample. One can argue that the population referred to a tertiary health center is not representative of the general population, for being knowingly composed of unhealthy individuals, which might interfere in the verification of FLLs frequency. However, considering the lack of recent prevalence studies relying on diagnostic imaging methods, the authors believe that the present study brings a significant contribution to understanding the behavior of cysts and hemangiomas. Future population studies will certainly clarify such questions. Additionally, anatomopathological studies were not utilized as a reference standard in the present study. However, the utilization of imaging parameters for the diagnosis of cysts and hemangiomas is widely diffused in the literature, thus eliminating the necessity of utilizing the gold standard, considering the questionable cost-benefit ratio in utilizing invasive procedures instead, to obtain a diagnosis of little prognostic repercussion for the patients under investigation. On the other hand, the analysis of liver explants in cirrhotic patients might contribute for the establishment of the actual frequency of cysts and hemangiomas in such group of patients. Finally, the diagnostic criteria utilized for inclusion of patients in the cirrhotic group considered clinical/laboratory parameters in a part of the sample (65%), and anatomopathological study in the other (35%) with less advanced stages of the disease, which, in a certain manner, reflects the characteristics of the population assisted in the authors' institution. CONCLUSIONS In the present study the values for prevalence of cysts and hemangiomas are higher than values reported by previously published autopsy series, a fact which the authors attribute to the high diagnostic capability of MRI for the described FLLs. Values that may be extrapolated to the general population are still to be obtained by means of population studies. The prevalence and behavior of such lesions in cirrhotic patients do not seem to be different from that in the non-cirrhotic population, contrary to what initial reports suggested. REFERENCES 1. Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754–73. 2. Megibow AJ. Preface imaging of incidentalomas. Radiol Clin North Am. 2011;49:xi–xii. 3. Ruiz Guinaldo A, Martín Herrera L, Roldán Cuadra R. Hepatic tumors in patients with cirrhosis: an autopsy study. Rev Esp Enferm Dig. 1997;89:771–80. 4. Karhunen PJ. Benign hepatic tumours and tumour-like conditions in men. J Clin Pathol. 1986;39:183–8. 5. Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975;59:995–1013. 6. Kudo M, Zheng RQ, Kim SR, et al. Diagnostic accuracy of imaging for liver cirrhosis compared to histologically proven liver cirrhosis. A multicenter collaborative study. Intervirology. 2008;51 Suppl 1:17–26. 7. Liver Imaging Reporting and Data System [homepage on the Internet]. Reston: American College of Radiology; c2011 [updated 2011 March; cited 2011 Aug 18]. Available from: http://www.acr.org/SecondaryMainMenuCategories/quality_safety/LI-RADS.aspx. 8. Lee KS, Sekhar A, Rofsky NM, et al. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010;105:2079–84. 9. Brancatelli G, Federle MP, Blachar A, et al. Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology. 2001;219:69–74. 10. Mastropasqua M, Kanematsu M, Leonardou P, et al. Cavernous hemangiomas in patients with chronic liver disease: MR imaging findings. Magn Reson Imaging. 2004;22:15–8. 11. Dodd GD 3rd, Baron RL, Oliver JH 3rd, et al. Spectrum of imaging findings of the liver in end-stage cirrhosis: Part II, focal abnormalities. AJR Am J Roentgenol. 1999;173:1185–92. 12. Sorensen AG, Buonanno FS, Gonzalez RG, et al. Hyperacute stroke: evaluation with combined multisection diffusion-weighted and hemodynamically weighted echo-planar MR imaging. Radiology. 1996;199:391–401. 13. Moseley ME, Kucharczyk J, Mintorovitch J, et al. Diffusion-weighted MR imaging of acute stroke: correlation with T2-weighted and magnetic susceptibility-enhanced MR imaging in cats. AJNR Am J Neuroradiol. 1990;11:423–9. 14. Gourtsoyianni S, Papanikolaou N, Yarmenitis S, et al. Respiratory gated diffusion-weighted imaging of the liver: value of apparent diffusion coefficient measurements in the differentiation between most commonly encountered benign and malignant focal liver lesions. Eur Radiol. 2008;18:486–92. 15. Koike N, Cho A, Nasu K, et al. Role of diffusion-weighted magnetic resonance imaging in the differential diagnosis of focal hepatic lesions. World J Gastroenterol. 2009;15:5805–12. 16. Vuillemin-Bodaghi V, Zins M, Vullierme MP, et al. Imaging of atypical cysts of the liver. Study of 26 surgically treated cases. Gastroenterol Clin Biol. 1997;21:394–9. 17. Gupta AA, Kim DC, Krinsky GA, et al. CT and MRI of cirrhosis and its mimics. AJR Am J Roentgenol. 2004;183:1595–601. 18. Washington K. Masses of the liver. In: Odze R, Goldblum JR, editors. Surgical pathology of the GI tract, liver, biliary tract and pancreas. 2nd ed. New York: Elsevier; 2009. p. 657–789. 19. Jones WL, Mountain JC, Warren KW. Symptomatic non-parasitic cysts of the liver. Br J Surg. 1974;61:118–23. 20. Cowles RS, Mulholland MW. Solitary hepatic cysts. J Am Coll Surg. 2000;191:311–21. 21. Kim JY, Kim SH, Eun HW, et al. Differentiation between biliary cystic neoplasms and simple cysts of the liver: accuracy of CT. AJR Am J Roentgenol. 2010;195:1142–8. 22. Foley PT, Sithasanan N, McEwing R, et al. Enteric duplications presenting as antenatally detected abdominal cysts: is delayed resection appropriate? J Pediatr Surg. 2003;38:1810–3. 23. Seo JK, Kim SH, Lee SH, et al. Appropriate diagnosis of biliary cystic tumors: comparison with atypical hepatic simple cysts. Eur J Gastroenterol Hepatol. 2010;22:989–96. 24. Eliason EL, Smith DC. Solitary nonparasitic cyst of the liver: case report. Clinics. 1944;3:607–21. 25. Sanfelippo PM, Beahrs OH, Weiland LH. Cystic disease of the liver. Ann Surg. 1974;179:922–5. 26. Feldman M. Polycystic disease of the liver. Am J Gastroenterol. 1958;29:83–6. 27. Gaines PA, Sampson MA. The prevalence and characterization of simple hepatic cysts by ultrasound examination. Br J Radiol. 1989;62:335–7. 28. Caremani M, Vincenti A, Benci A, et al. Ecographic epidemiology of non-parasitic hepatic cysts. J Clin Ultrasound. 1993;21:115–8. 29. Craig JR, Peters RL, Edmonson HA. Tumors of the liver and intrahepatic bile ducts. In: Atlas of human pathology. 2nd ed. Washington, DC: Armed Forced Institute of Pathology; 1989. p. 56–62. 30. Carrim ZI, Murchison JT. The prevalence of simple renal and hepatic cysts detected by spiral computed tomography. Clin Radiol. 2003;58:626–9. 31. Faulds JM, Scudamore CH. Technical report of a novel surgical technique: laparoscopic cyst fenestration and falciform ligament pedicle graft for treatment of symptomatic simple hepatic cysts. J Laparoendosc Adv Surg Tech A. 2010;20:857–61. 32. Ramia JM, de La Plaza R, Figueras J, et al. Tumores hepáticos quísticos benignos no parasitarios. Cir Esp. 2011;89:565–73. 33. Itoh K, Saini S, Hahn PF, et al. Differentiation between small hepatic hemangiomas and metastases on MR images: importance of size-specific quantitative criteria. AJR Am J Roentgenol. 1990;155:61–6. 34. Semelka RC, Brown ED, Ascher SM, et al. Hepatic hemangiomas: a multi-institutional study of appearance on T2-weighted and serial gadolinium-enhanced gradient-echo MR images. Radiology. 1994;192:401–6. 35. Tung GA, Vaccaro JP, Cronan JJ, et al. Cavernous hemangioma of the liver: pathologic correlation with high-field MR imaging. AJR Am J Roentgenol. 1994;162:1113–7. 36. Semelka RC, Sofka CM. Hepatic hemangiomas. Magn Reson Imaging Clin N Am. 1997;5:241–53. 37. Edmondson HA. Tumors of the liver and intrahepatic bile ducts. In: Atlas of tumor pathology. Washington, DC: Armed Forces Institute of Pathology; 1958. p. 24–8. 38. Oliver JH 3rd, Baron RL, Dodd GD 3rd, et al. Does advanced cirrhosis with portosystemic shunting affect the value of CT arterial portography in the evaluation of the liver? AJR Am J Roentgenol. 1995;164:333–7. 39. Yamashita Y, Ogata I, Urata J, et al. Cavernous hemangioma of the liver: pathologic correlation with dynamic CT findings. Radiology. 1997;203:121–5. 40. Namimoto T, Yamashita Y, Sumi S, et al. Focal liver masses: characterization with diffusion-weighted echo-planar MR imaging. Radiology. 1997;204:739–44. 41. Kim T, Federle MP, Baron RL, et al. Discrimination of small hepatic hemangiomas from hyper-vascular malignant tumors smaller than 3 cm with three-phase helical CT. Radiology. 2001;219:699–706. 1. MDs, Residents, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 2. MDs, Radiologists, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 3. Associate Professor, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Giuseppe D'Ippolito Departamento de Diagnóstico por Imagem – EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04508-011 E-mail: giuseppe_dr@uol.com.br Received April 21, 2012. Accepted after revision March 19, 2013. * Study developed in the Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554