Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 4 - July / Aug. of 2013
Vol. 46 nº 4 - July / Aug. of 2013
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Lucas Fiore1; Nivaldo Adolfo da Silva Junior2; Renata Bertanha3; Ines Minniti Rodrigues Pereira4; Fabiano Reis4 |
|
|
A 58-year-old woman was complaining of headache for six days.
IMAGES DESCRIPTION Figure 1. Head unenhanced CT scan. A: Axial plane discloses a cerebellar parenchyma hematoma. B: Sagittal reformation image shows the cerebellar hematoma adjacent to the tentorium. 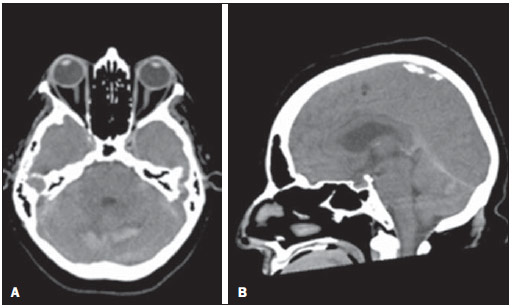 Figure 1. Head unenhanced computed tomography (CT). A: Axial slice. B: Sagittal reformation image. Figure 2. Head unenhanced axial MR T1-weighted image discloses an acute parenchyma hemorrhage in the cerebellar hemispheres. There is no signal abnormality within the dural sinuses. 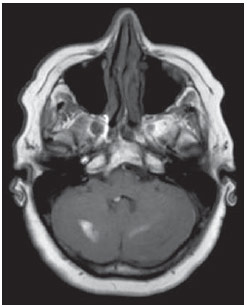 Figure 2. Head unenhanced axial T1-weighted magnetic resonance image (MRI). Figure 3. Head CT angiography. Sagittal reformation image demonstrates an abnormal vascular dilation, probably corresponding to the vermian vein draining into the straight sinus. 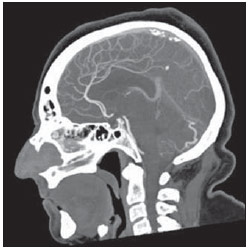 Figure 3. Head CT angiography, sagittal reformation image. Figure 4. Digital subtraction brain angiography (DSA) with selective injection in the internal (A) and external carotid artery (B), disclosing a dural fistula at the cerebellar tentorium supplied by tentorial and (A) and occipital arteries (B). The venous drainage occurs through a cortical vein (vermian vein). 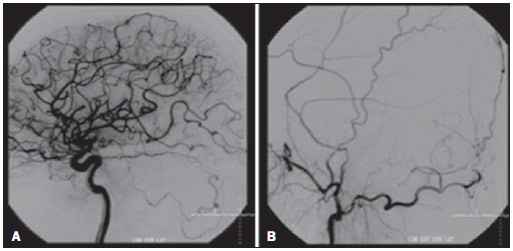 Figure 4. Selective internal(A) and external carotid artery angiography (B). Diagnosis: Intracranial dural arteriovenous fistula. COMMENTS Intracranial dural arteriovenous fistulas (DAVFs) comprise 10% to 15% of all cerebrovascular malformations. Although such fistulas may occur at any location in the dura mater, they are most frequently found in the cavernous and transverse sinuses(1). Clinical findings include those associated to intracranial hypertension (headache, nausea and vomiting, visual deficit, papilledema), focal deficits, convulsions, mental state alterations, tinnitus(1–3). The first classification of DAVFs was created in 1978, and showed that more aggressive symptoms and hemorrhage were usually associated to fistulas which had cortical venous drainage(4). One of the most accepted classifications was developed in 1995 by Cognard et al., and correlates the fistula angioarchitecture with the neurological prognosis, particularly the risk for intracranial hemorrhage. Its main objective is to aid the decision treatment. Such classification categorized dural fistulas into five types as : a) type I – venous drainage into to the dural sinus, and the flow direction of the fistula is the same of the physiological blood flow within the sinus; b) type II – subdivided into IIa, where the venous drainage occurs towards the venous sinus, but the drainage direction is opposite to the physiological blood flow within the sinus; IIb, as the venous drainage occurs towards the venous sinus and there is also reflux into the cortical veins; and IIa+b, a combination of both previous descriptions; c) type III – fistulas draining directly into cortical veins without ectasia; d) type IV – those draining into the cortical veins associated with ectasia; e) type V – those draining into perimedullary veins(2). Types I and IIa DAVFs represent almost half of the fistula cases and are not usually associated with hemorrhage. Type I DAVFs are associated with functional symptoms such as tinnitus. About one third of type II DAVFs may be associated with intracranial hypertension. Fistulas with cortical venous drainage present considerable risk for hemorrhage(2). Another widely accepted classification is that developed by Borden et al. (1995), dividing the patients into three groups, the first one with sinusal or meningeal venous drainage; the second group with sinusal drainage associated with cortical venous reflux; and the third one with only cortical venous reflux(5). Our case corresponds to the type II DAVF according to the classification developed by Cognard et al.(4), considering the presence of a direct drainage into the cortical vein, without ectasia. These fistulas are commonly associated with aggressive symptoms, and in about 40% of cases they complicate with hemorrhage(2). Pathological conditions involved in the development of DAVFs include: cranioencephalic trauma, cerebral thrombophlebitis, previous neurosurgery and infections(2). DSA remains as the gold standard in the diagnosis of DAVF, but either 3D time-off-light magnetic resonance angiography or 4D dynamic magnetic resonance angiography have high sensitivity and specificity in the diagnosis of moderate- to high-flow fistulas(6–8). 64-detector-row CT angiography represents a promising technique, both for its lower invasiveness and higher diagnostic sensitivity and specificity (93% and 98%, respectively)(9). Therapeutic options for DAVFs include conservative, endovascular or surgical treatment. Currently, the endovascular treatment is most commonly indicated, with good results and low complications index. Different materials, such as Onix® and micro-coils, can be utilized according to the medical team experience and fistula angioarchitecture(10,11). In cases where endovascular treatment is not possible, open surgery may be used, particularly in cases involving DAVFs in the anterior fossa(1). REFERENCES 1. iyosue H, Hori Y, Okahara M, et al. Treatment of intracranial dural arteriovenous fistulas: current strategies based on location and hemodynamics, and alternative techniques of transcatheter embolization. Radiographics. 2004;24:1637–53. 2. Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–80. 3. Geibprasert S, Pongpech S, Jiarakongmun P, et al. Radiologic assessment of brain arteriovenous malformations: what clinicians need to know. Radiographics. 2010;30:483–501. 4. Djindjian R, Merland JJ. Super-selective arteriography of the external carotid artery. Berlin: Springer-Verlag; 1978. 5. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166–79. 6. Nishimura S, Hirai T, Sasao A, et al. Evaluation of dural arteriovenous fistulas with 4D contrast-enhanced MR angiography at 3T. AJNR Am J Neuroradiol. 2010;31:80–5. 7. Wetzel SG, Bilecen D, Lyrer P, et al. Cerebral dural arteriovenous fistulas: detection by dynamic MR projection angiography. AJR Am J Roentgenol. 2000;174:1293–5. 8. Noguchi K, Melhem ER, Kanazawa T, et al. Intracranial dural arteriovenous fistulas: evaluation with combined 3D time-of-flight MR angiography and MR digital subtraction angiography. AJR Am J Roentgenol. 2004;182:183–90. 9. Lee CW, Huang A, Wang YH, et al. Intracranial dural arteriovenous fistulas: diagnosis and evaluation with 64-detector row CT angiography. Radiology. 2010;256:219–28. 10. Cognard C, Januel AC, Silva NA Jr. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: new management using Onyx. AJNR Am J Neuroradiol. 2008;29:235–41. 11. Yoshida K, Melake M, Oishi H, et al. Transvenous embolization of dural carotid cavernous fistulas: a series of 44 consecutive patients. AJNR Am J Neuroradiol. 2010;31:651–5. 1. MD, Resident, Radiology Department, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil 2. MD, Physician Assistant, Radiology Department, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil 3. MD, Resident, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil 4. PhDs, Professors, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil Mailing Address: Dr. Fabiano Reis Hospital de Clínicas da Universidade Estadual de Campinas Rua Vital Brasil, 251, Cidade Universitária Zeferino Vaz Campinas, SP, Brazil, 13083-888. Caixa Postal 6142 E-mail: fabianoreis2@gmail.com Study developed at Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554