Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 3 - May / June of 2013
Vol. 46 nº 3 - May / June of 2013
|
CASE REPORT
|
|
Bilateral Killian-Jamieson diverticula demonstrated by videofluoroscopic swallowing study: case report |
|
|
Autho(rs): Betina Scheeren1; Renato José Kist de Mello2; Caren Meneghetti Gonçalves2; Antonio Carlos Maciel3 |
|
|
Keywords: Deglutition disorders; Diverticulum. |
|
|
Abstract: INTRODUCTION
Killian-Jamieson diverticulum was described in 1983 by Ekberg et al. and occurs in the anterolateral wall of the cervical esophagus and distally to the cricopharyngeal muscle(1). In the literature, it is described as a rare, generally unilateral diverticulum – only in 25% of cases it occurs bilaterally. It is different from Zenker's diverticulum that is most commonly known and develops at the midline of the posterior esophageal wall, above the cricopharyngeal muscle (a region that is also named Killian's triangle), frequently causing aspiration. Both types of diverticula occur in sites of anatomical weakness of the hypopharynx or cervical esophagus(2). Dysphagia is the main symptom of Killian-Jamieson diverticulum, particularly for solid foods(3). However, because of its location, it is less susceptible to cause as-piration(2). The diagnosis is made by means of barium esophagram(4), and videofluoroscopic swallowing study is a dynamic method which evaluates the deglutition process, allowing the detection of anatomic/functional dysfunctions(5–7). The present report is aimed at describing the case of a patient with bilateral Killian-Jamieson diverticula demonstrated by videofluoroscopic swallowing study. CASE REPORT Male, 56-year-old patient complaining of dysphagia for solids and food impaction referred to undergo videofluoroscopic swallowing study. The patient had undergone other diagnostic procedures, among them upper digestive endoscopy, which demonstrated only the presence of mild antral erosive gastritis, and barium esophagram, whose report described the presence of a Zenker's diverticulum. The patient was submitted to swallowing videofluoroscopy, including lateral and frontal dynamic imaging of the oral, pharyngeal and esophageal phases of deglutition performed with the patient upright. The patient ingested food of three different consistencies – liquid, pasty and solid – with barium sulfate contrast suspension. The study was performed by a speech therapist under the guidance of a radiologist. Such study demonstrated the presence of two diverticular structures in communication with the cervical esophagus, located below the upper esophageal sphincter, with retention of the contrast-enhanced food bolus (Figures 1, 2 and 3). 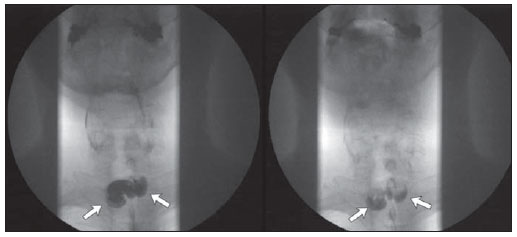 Figure 1. Frontal views demonstrate two lateral prominences (arrows) corresponding to Killian-Jamieson diverticula. 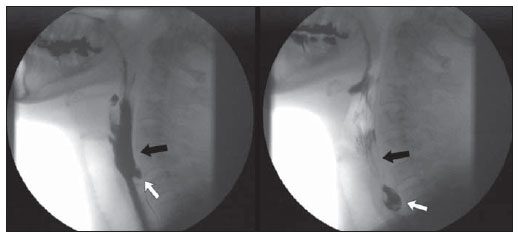 Figure 2. Lateral views demonstrate the presence of a Killian-Jamieson diverticulum (white arrows) located distally to the cricopharyngeal muscle (black arrows). 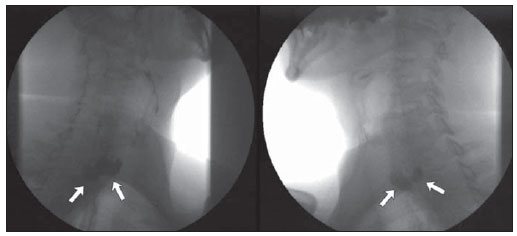 Figure 3. Oblique views demonstrate two diverticular structures (arrows) corresponding to Killian-Jamieson diverticula. DISCUSSION Killian-Jamieson diverticulum develops because of herniation of the mucosa and submucosa in a site of weakness in the anterolateral wall of the cervical esophagus, inferiorly to the cricopharyngeal muscle and superolaterally to the esophageal longitudinal muscle. This gap in the muscle was initially described by Killian as the site where the recurrent laryngeal nerve inserts into the pharynx. Jamieson confirmed such finding and thus this area was named Killian-Jamieson triangle(3). On the other hand, Zenker's diverticulum originates proximally to the upper esophageal sphincter and is classified as a pharyngeal diverticulum. This diverticulum protrudes through the weakened area of the muscle located between the cricopharyngeal and lower constrictor muscles and named Killian triangle (Figure 4)(8). In cases of large diverticula, food retention causing regurgitation, dysphagia and even aspiration pneumonia may occur(9). 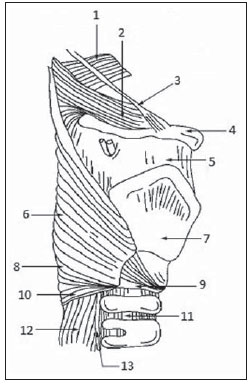 Figure 4. Anatomical drawing demonstrating weakened muscle areas through which Zenker's (8) and Killian-Jamieson (13) diverticula protrude. 1, upper constrictor muscle; 2, middle constrictor muscle; 3, styloid hyoid ligament; 4, hyoid bone; 5, thyrohyoid membrane; 6, thyropharyngeus muscle; 7, thyroid cartilage; 8, Killian's dehiscence; 9, cricoid cartilage; 10, cricopharyngeal muscle; 11, trachea; 12, esophagus; 13, recurrent laryngeal nerve. (drawing adapted from Siddiq et al.(8)). The location of the cricopharyngeal muscle is important to define and subsequently diagnose the type of diverticulum. It is possible to identify the cricopharyngeal muscle located ventrally at the level of C4–C6 and cricoids cartilage. It is observed during the videofluoroscopic swallowing study at the moment f its relaxation and consequential opening of the upper esophageal sphincter. The diagnosis of Killian-Jamieson diverticulum is generally made with barium esophagram, where it is seen as a lateral protrusion at frontal views, and overlapping to the anterior esophageal wall at lateral views(2). Studies in the literature(10–12) report the Killian-Jamieson diverticulum diagnosis by means of ultrasonography, either as an incidental finding or mimicking a thyroid nodule. At ultrasonography, Killian-Jamieson diverticulum is seen as an echogenic and heterogeneous nodule, with some hyperechoic spots suggesting the presence of air which do not move during swallowing. In a report about 13 cases of Killian-Jamieson diverticulum observed at ultrasonography(10), the communication with the adjacent esophageal wall could be demonstrated in 54% of the patients at the moment of the initial diag osis. The advantage of ultrasonography is the non-invasiveness and absence of ionizing radiation as compared with other imaging methods, besides the fact that the scan can be performed outside a hospital setting(13). However, in the present case, videofluoroscopic swallowing study was required for the differential diagnosis with Zenker's diverticulum. Sometimes, it may be difficult to differentiate between the two diverticula at barium esophagram, since the Zenker's diverticulum may extend downwards and, in cases of a large diverticulum, protrude to the left in relation to the mid-line(3). When unilateral, Killian-Jamieson diverticulum may sometimes be confused with Zenker's diverticulum. But, at lateral view the Killian-Jamieson diverticulum protrudes anteriorly in relation to the cervical esophagus, while the Zenker's diverticulum protrudes posteriorly(14). It is important to differentiate these two diverticula, particularly under the clinical point of view in relation to complications and therapeutic approach. Amongst the related complications, the main difference is concerned with tracheal aspiration which is much more frequent in cases of Zenker's diverticulum because of its location above the upper esophageal sphincter(2,3). Only symptomatic patients and those with large diverticula should be treated. Treatment options include either open or endoscopic surgery, with diverticolotomy, diverticulolectomy or diverticulopexy. According to Chea et al.(4), diverticulopexy is recommended as an effective and preferential option for treatment of Killian-Jamieson diverticula. For the treatment(15), it is important to differentiate Killian-Jamieson diverticulum from Zenker's diverticulum because despite the surgical and endoscopic options, the endoscopic treatment is preferable for Zenker's diverticula (particularly those < 3 cm); and for the Killian-Jamieson diverticula, the safety of the endoscopic approach is still to be completely established, mostly because of the rarity of cases. The main complication associated with the endoscopic treatment is injury to the recurrent laryngeal nerve, since the base of the Killian-Jamieson diverticulum is the site of insertion of the nerve into the larynx. The traditional videofluoroscopic swallowing study generally emphasizes the assessment of the oral cavity and pharynx, but constitutes a relevant diagnostic tool also in cases of disorders of the hypopharynx and esophagus because the symptom of cervical dysphagia may have an esophageal cause(16). CONCLUSION In the presently reported case, barium esophagram could not correctly identify the nature of the dysphagia and the food impaction reported by the patient. Such identification might be possible at the videofluoroscopic swallowing study. Therefore, the authors highlight the relevance of the analysis of the oral, pharyngeal and esophageal swallowing phases for the differential diagnosis of oropharyngeal complaints related to esophageal alterations. REFERENCES 1. Ekberg O, Nylander G. Lateral diverticula from the pharyngo-esophageal junction area. Radiology. 1983;146:117–22. 2. Rubesin SE, Levine MS. Killian-Jamieson diverticula: radiographic findings in 16 patients. AJR Am J Roentgenol. 2001;177:85–9. 3. Boisvert RD, Bethune DC, Acton D, et al. Bilateral Killian-Jamieson diverticula: a case report and literature review. Can J Gastroenterol. 2010;24:173–4. 4. Chea CH, Siow SL, Khor TW, et al. Killian-Jamieson diverticulum: the rarer cervical esophageal diverticulum. Med J Malaysia. 2011;66:73–4. 5. Cappabianca S, Reginelli A, Monaco L, et al. Combined videofluoroscopy and manometry in the diagnosis of oropharyngeal dysphagia: examination technique and preliminary experience. Radiol Med. 2008;113:923–40. 6. Levine MS, Rubesin SE, Laufer I. Barium esophagography: a study for all seasons. Clin Gastroenterol Hepatol. 2008;6:11–25. 7. Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008;19:769–85. 8. Siddiq MA, Sood S, Strachan D. Pharyngeal pouch (Zenker's diverticulum). Postrgrad Med J. 2001;77:506–11. 9. Freeny PC, Stevenson GW. Benign structural diseases of the pharynx. In: Margulis AR, Burhenne HJ, editors. Alimentary tract radiology. St. Louis, MO: Mosby; 1994. p. 114–26. 10. Kim HK, Lee JI, Jang HW, et al. Characteristics of Killian-Jamieson diverticula mimicking a thyroid nodule. Head Neck. 2012;34:599–603. 11. Kim MH, Kim EK, Kwak JY, et al. Bilateral Killian-Jamieson diverticula incidentally found on thyroid ultrasonography. Thyroid. 2010;20:1041–2. 12. Pang JC, Chong S, Na HI, et al. Killian-Jamieson diverticulum mimicking a suspicious thyroid nodule: sonographic diagnosis. J Clin Ultrasound. 2009;37:528–30. 13. Sakate M, Yamashita S, Toledo CGC, et al. Avaliação do tempo de trânsito esofágico pelo ultrassom: influência do gênero e índice de massa corpórea. Radiol Bras. 2011;44:360–2. 14. Johnson CD, Schmit GD. Mayo Clinic gastrointestinal imaging review. Rochester, MN: Mayo Clinic Scientific Press; 2005. 15. Kim DC, Hwang JJ, Lee WS, et al. Surgical treatment of Killian-Jamieson diverticulum. Korean J Thorac Cardiovasc Surg. 2012;45:272–4. 16. Allen JE, White C, Leonard R, et al. Comparison of esophageal screen findings on videofluoroscopy with full esophagram results. Head Neck. 2012;34:264–9. 1. Speech Therapist at Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil. 2. MDs, Residents, Unit of Radiology and Imaging Diagnosis, Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil. 3. PhD, Head of the Unit of Radiology and Imaging Diagnosis, Hospital Santa Clara and Hospital São Francisco da Santa Casa de Misericórdia de Porto Alegre, MD, Radiologist, Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brazil. * Study developed at Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil. Mailing Address: Betina Scheeren Rua Fernandes Vieira, 353, ap. 46, Bairro Bom Fim Porto Alegre, RS, Brazil, 90035-091 E-mail: betinascheeren@hotmail.com Received June 12, 2012. Accepted after revision January 28, 2013. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554