Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 3 - May / June of 2013
Vol. 46 nº 3 - May / June of 2013
|
ICONOGRAPHIC ESSAY
|
|
Pyogenic and tuberculous discitis: magnetic resonance imaging findings for differential diagnosis |
|
|
Autho(rs): Cristiano Gonzaga de Souza1; Emerson Leandro Gasparetto2; Edson Marchiori3; Paulo Roberto Valle Bahia4 |
|
|
Keywords: Magnetic resonance imaging; Discitis; Intervertebral disc; Spinal tuberculosis. |
|
|
Abstract: INTRODUCTION
The imaging evaluation of the musculoskeletal system has been object of a range of studies recently published in the Brazilian radiological literature(1–7). Among such studies, some related to the vertebral spine are highlighted(8–10). Spondylodiscitis represent 2%–4% of all cases of skeletal infection(11) and its radiological diagnosis is based on the demonstration of the involvement of the vertebral body and adjacent intervertebral disc, although several non-infectious diseases may mimic this condition(11). Three forms of dissemination are described, as follows: hematogenous spread from a distant septic focus; direct inoculation (either by surgery or trauma); contiguity with an adjacent septic focus. Generally, the infection starts in the anterior portion of the vertebral body because of its rich arterial supply, and spreads through the medullary spaces, affecting the intervertebral disc by contiguity, most frequently involving the lumbar and dorsal segments of the spine (50% and 35% of cases, respectively)(12). Generally, late diagnosis is the rule (on average, two to six months after the symptoms onset)(13). A fast diagnosis allows the institution of appropriate treatment and may avoid complications such as vertebral collapse and medullary compression syndrome. In this context, imaging investigation is critical for the diagnosis and follow-up of the lesions so as to reduce the necessity of invasive procedures. Magnetic resonance imaging (MRI) is the method of choice because of its high sensitivity and specificity(14), as well as good tissue resolution and multiplanar capacity(15). Also, MRI can be useful to suggest the origin of the infection – although this is not always possible –, aiding in the differentiation between tuberculous and pyogenic infections, thus allowing efficacy in the treatment of the patient(16). Main MRI findings include hyposignal on T1-weighted and hypersignal on T2-weighted images from the vertebral bodies and adjacent intervertebral discs, as well as enhancement after intravenous paramagnetic contrast medium injection, besides paravertebral masses/abscesses, all of them nonspecific(17). However, as some details are correctly individualized and each finding is appropriately interpreted, they may become useful tools to guide the radiologist in the differential diagnosis. The present pictorial essay is aimed at gathering and demonstrating some imaging findings in order to appropriately highlight evidences of higher suspicion degree of etiological agents, according to the available literature. PYOGENIC SPONDYLODISCITIS Pyogenic spondylodiscitis affects most frequently the lumbar spine, involving only one vertebral segment (one intervertebral disk and adjacent vertebral bodies). Most frequently, Staphylococcus aureus is the etiological agent implied in the infection, responsible for 55%–90% of the cases(18). Other relevant agents include Streptococcus, Pneumococcus, Enterococcus, Escherichia coli, Salmonella, Pseudomonas aeruginosa and Klebsiella(18). Because of the high concentration of proteolytic enzymes intrinsic to the virulence of these biological agents, the disc involvement occurs early in the course of the disease and can be demonstrated concomitantly with the corresponding vertebral body lesion at very initial stages of infection. The vertebral body involvement tends to be more homogeneous in relation to the alterations in signal intensity on T1- and T2-weighted sequences and to the enhancement of its medullary spaces(19). Considering the remarkable worsening in the general condition as well as important features of the symptoms affecting the patient, imaging studies are requested at the initial phase of the disease where, although the appearance of the lesion is more aggressive, it is less disseminated in multiple vertebral bodies, so the finding of large abscesses or paravertebral masses is not expected. In cases where such findings are present, however, the lesion is poorly defined, depending on the aggressiveness of the implied etiological agent(11). Thus, MRI findings which lead to the suspicion of pyogenic spondylodiscitis include segmental involvement (Figures 1 and 2), presence of poorly defined paravertebral mass (Figure 3), early intervertebral disc involvement (Figure 2), and homogeneous enhancement/alteration of signal of affected vertebral bodies (Figures 1 and 2). 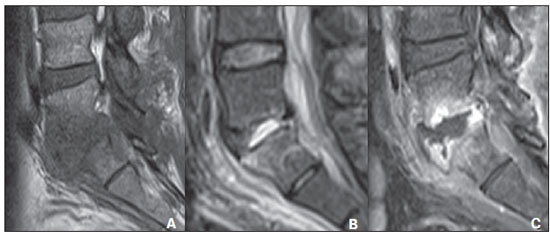 Figure 1. Segmental involvement of L5-S1 and of the interposed intervertebral disc. Lesion with hyposignal on T1-weighted (A) and hypersignal on STIR (B) images of the L5-S1 disc, with enhancement and irregularities in the adjacent vertebral plateaus (C). Culture of the material collected from the vertebral body revealed the presence of Staphylococcus aureus. 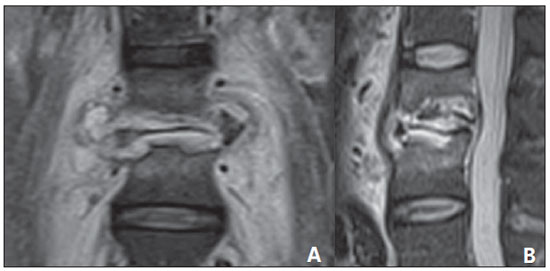 Figure 2. Segmental involvement of L3-L4 and of the interposed intervertebral disc in the coronal (A) and sagittal planes (B). Remarkable irregularity of the vertebral plateaus in association with homogeneous hypersignal of the vertebral body on the STIR image. Culture of the material collected from the intervertebral disc revealed the presence of Enterococcus sp. 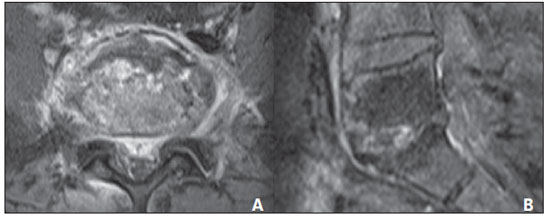 Figure 3. Segmental involvement of L5-S1 and of the interposed intervertebral disc. Poorly defined paravertebral collection, with intense gadolinium enhancement on axial (A) and sagittal (B) T1-weighted image with fat suppression. Note the early disc involvement. Culture of the collected material revealed the presence of Pneumococcus sp. TUBERCULOUS SPONDYLODISCITIS The spine is the main site of bone involvement by tuberculosis, responsible for 50% of the cases(20). The differential diagnosis with pyogenic spondylodiscitis is clinically and radiologically difficult to be achieved, particularly in cases where the etiological agent is less aggressive, like in cases of brucelosis. The scarcity of proteolytic enzymes, which is an intrinsic characteristic of Mycobacterium tuberculosis, results in a remarkably late, indolent infection of the intervertebral disc(21). Thus, tuberculous spondylodiscitis may originate large paravertebral abscesses or granulomatous masses with well defined borders(17), extending into the subligamentous space through several (typically more than three) vertebral bodies at the time of the imaging diagnosis. An irregular pattern of involvement may also be observed15, besides a more heterogeneous involvement of vertebral bodies, provided there is time for the bone tissue to react against the infection. Thus, focal areas of altered signal intensity are observed on T1- and T2-weighted images, besides focal enhancement of part of medullary spaces of the vertebral body. Such findings allow the demonstration of discrepancy in the involvement between discs and adjacent structures such as vertebral bodies and paravertebral region. Thus, disc involvement is noticeable in later phases of the disease. At early phases, the disc is usually intact, although it is already possible to identify the presence of extensive bone involvement or large paravertebral abscesses/masses which, typically, tend to present well defined contours. At early phases of the disease, the differential diagnosis with, for example, neoplastic (Figure 6), degenerative (Figure 7) or inflammatory etiologies may be hardly made. In such cases, morphological criteria, presence of signal from affected regions on T2-weighted images, and the characteristics of the gadolinium enhancement may be useful to shorten the list of diagnostic hypotheses(22). 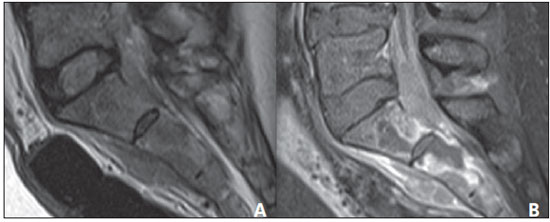 Figure 4. Multisegmental involvement. Paravertebral mass with subligamentous extension on STIR image (A) and intense and heterogeneous contrast enhancement on L5-S1 to S2-S3, with development of intraosseous abscesses at S1 and S2 on post-gadolinium T1-weighted sequence with fat suppression (B). Note that the corresponding intervertebral disc is apparently intact. PCR of the material was positive for Mycobacterium tuberculosis. 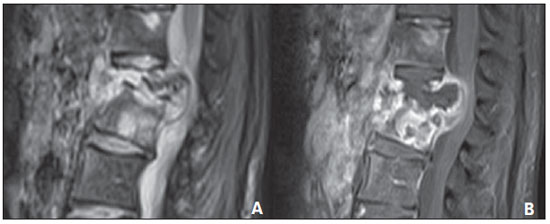 Figure 5. Multisegmental involvement. Total collapse of L1 and partial collapse of L2 in association with heterogeneous medullary space enhancement following intravenous gadolinium injection, demonstrating the presence of intraosseous abscess at L2 and heterogeneous, expansile paravertebral mass at the level of L1 to L3 with hypersignal on STIR (A) and peripheral enhancement (B). The lesion extends toward the paravertebral region, posteriorly compressing the dural sac. Culture of the material revealed the presence of Mycobacterium tuberculosis. 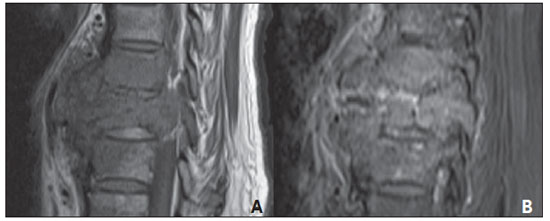 Figure 6. Large, poorly defined paravertebral mass on T1-weighted image (A), with heterogeneous contrast-enhancement on T1-weighted image with fat suppression (B), affecting vertebral bodies T8 and T9, in association with intact intervertebral disc. Vertebral body biopsy revealed the neoplastic etiology of the lesion (implant). 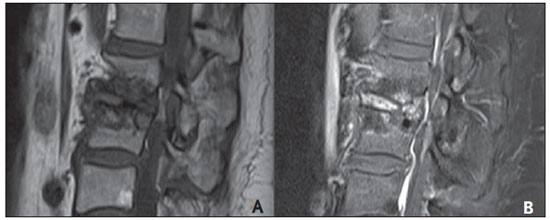 Figure 7. Remarkable irregularity and hyposignal of vertebral plateaus L2-L3 on T1-weighted image T1 (A), with intense disc enhancement on gadoliniumenhanced T1-weighted image with fat suppression (B). The vertebral plateaus do not present contrast enhancement. Several punctures were performed to evaluate the material. Microorganisms growth was not observed. Vertebral body biopsy revealed the presence of degenerative joint disease mimicking infectious spondylodiscitis. Inflammatory spondylites such as ankylosing spondylitis, psoriatic spondylitis and reactive spondylitis, over its natural history, may present alterations similar to the ones of degenerative spondylitis. However, the vertebral involvement is typically associated with, and sometimes preceded by either symmetrical or asymmetrical, bilateral sacroiliitis, depending on each etiology(23). Usually, neoplastic lytic lesions with metastasis to the axial skeleton are not associated with reactive sclerosis or periosteal reaction; and, typically, the first sites of involvement are the vertebral pedicles(23). Degenerative spondylites, like infectious cases, may present enhancement of the intervertebral disc on the post-gadolinium sequences. However, the affected vertebral plateaus tend to present hyposignal on T2-weighted images and no contrast-enhancement after intravenous gadolinium injections(23). Considering the complex dissemination of the etiological agent of tuberculosis through the body, with different dissemination patterns depending on the phase of disease onset, some atypical patterns (classified according the mode and initial site of infection) are described in addition to the classical paradiscal infection where the disc involvement occurs by contiguity with adjacent vertebral plateaus, classified according their initial involvement(23). Thus the central, anterior subperiosteal and appendicular patterns of dissemination are observed, all of them corresponding to the findings focused by the present essay, but their description is not included in the scope of this study. The MRI findings suspicious for tuberculous spondylodiscitis include multisegmental subligamentous involvement (Figure 4); presence of well defined paravertebral mass/abscess (Figures 5 and 8); relatively spared disc at early phases of the disease (Figure 4); and heterogeneous enhancement/change in signal of vertebral bodies (Figures 5 and 8). 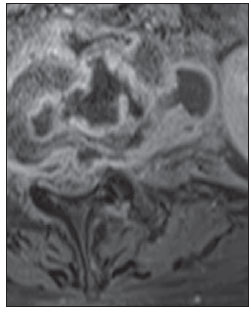 Figure 8. Paravertebral, well-defined, thin-walled collection on post-gadolinium T1-weighted sequence. Note the presence of exuberant, peripheral contrast enhancement, typical of collections. Culture of the collected material revealed Mycobacterium tuberculosis. CONCLUSION The characteristics of MRI findings play a relevant role in the diagnosis of complications inherent to infectious processes established in the vertebral spine, as well as in the determination of the involvement extent. However, it is not rare that radiologists investigate evidences suggesting the probable implied etiological agent. The etiological diagnosis of spondylodiscitis is hardly established on the grounds of isolated imaging findings criteria since many times they are nonspecific. However, the disproportion of the degree of involvement of the intervertebral disc in relation to the corresponding vertebral plateaus, the homogeneity of the vertebral bodies signal and enhancement, as well as the paravertebral masses volume and contours(19) should be appropriately taken into consideration as useful – although not definitive – tool in the investigation of a possible etiologic agent (Table 1). Thus, the MRI specificity for the diagnosis of spondylodiscitis is directly dependent on the characteristics of the signal, on the anatomic distribution, on the proportionality between vertebral bodies and intervertebral discs involvement, on the homogeneity of enhancement of the medullary spaces of vertebral bodies and, invariably, on the clinical history of the patient, although it is not always available at the moment of the imaging reporting(17). 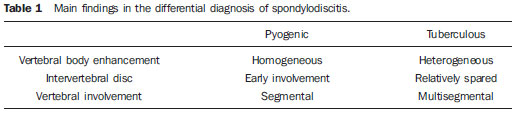 REFERENCES 1. Ribeiro DS, Araújo Neto C, D'Almeida F, et al. Achados de imagem das alterações musculoesqueléticas associadas ao lúpus eritematoso sistêmico. Radiol Bras. 2011;44:52–8. 2. Simão MN, Nogueira-Barbosa MH. Ressonância magnética na avaliação das variações anatômicas meniscais e da anatomia ligamentar perimeniscal: potenciais causas de erro de interpretação. Radiol Bras. 2011;44:117–22. 3. Nunes RB, Amaral DT, Oliveira VS. Propedêutica radiológica do impacto femoroacetabular em tempos de tomografia computadorizada e ressonância magnética: o que o radiologista precisa saber. Radiol Bras. 2011;44:249–55. 4. Cotta AC, Melo RT, Castro RCR, et al. Dificuldades diagnósticas no osteoma osteoide do cotovelo: estudo clínico, radiológico e histopatológico. Radiol Bras. 2012;45:13–9. 5. Moura MVT. Interposição de fragmento periosteal na fratura da placa epifisária femoral distal: estudo por ressonância magnética. Radiol Bras. 2012;45:184–6. 6. Chojniak R, Grigio HR, Bitencourt AGV, et al. Biópsia percutânea por agulha grossa de tumores de partes moles guiada por tomografia computadorizada: resultados e correlação com análise da peça cirúrgica. Radiol Bras. 2012;45:259–62. 7. Tavares Júnior WC, Faria FM, Figueiredo R, et al. Fadiga óssea: causa de dor em joelhos na osteoartrite. Radiol Bras. 2012;45:273–8. 8. Grassi CG, Diniz FV, Garcia MRT, et al. Aspectos de imagem na tendinite calcária pré-vertebral. Radiol Bras. 2011;44:327–30. 9. Jacob Jr C, Barbosa DM, Batista PR, et al. Fratura toracolombar do tipo explosão: o que o radiologista deve conhecer. Radiol Bras. 2012;45:101–4. 10. Simão MN, Helms CA, Richardson WJ. Achados de ressonância magnética em cistos epidurais de origem discal em pacientes não operados e após microdiscectomia. Radiol Bras. 2012;45:205–9. 11. Maiuri F, Iaconetta G, Gallicchio B, et al. Spondylodiscitis. Clinical and magnetic resonance diagnosis. Spine (Phila Pa 1976). 1997;22:1741–6. 12. Sharif HS. Role of MR imaging in the management of spinal infections. AJR Am J Roentgenol. 1992;158:1333–45. 13. Malawski SK, Lukawski S. Pyogenic infection of the spine. Clin Orthop. 1991;(272):58–66. 14. Varma R, Lander P, Assaf A. Imaging of pyogenic infectious spondylodiskitis. Radiol Clin North Am. 2001;39:203–13. 15. Prasad A, Manchanda S, Sachdev N, et al. Imaging features of pediatric musculoskeletal tuberculosis. Pediatr Radiol. 2012;42:1235–49. 16. Daher S, Pimenta Jr WE, Souza Jr ZA, et al. Qual o seu diagnóstico? Radiol Bras. 2004;37:v–vii. 17. Hong SH, Choi JY, Lee JW, et al. MR imaging assessment of the spine: infection or an imitation? Radiographics. 2009;29:599–612. 18. Resnik D. Osteomyelitis, septic arthritis and soft tissue infection: axial skeleton. In: Resnick D, editor. Diagnosis of bone and joint disorders. 4th ed. Philadelphia, PA: Saunders; 2002. p. 2481–509. 19. Ledermann HP, Schweitzer ME, Morrison WB, et al. MR imaging findings in spinal infections: rules or myths? Radiology. 2003;228:506–14. 20. Moon MS. Tuberculosis of the spine. Controversies and a new challenge. Spine (Phila Pa 1976). 1997;22:1791–7. 21. Gouliamos AD, Kehagias DT, Lahanis S, et al. MR imaging of tuberculous vertebral osteomyelitis: pictorial review. Eur Radiol. 2001;11:575–9. 22. Bron JL, de Vries MK, Snieders MN, et al. Disco-vertebral (Andersson) lesions of the spine in ankylosing spondylitis revisited. Clin Rheumatol. 2009;28:883–92. 23. Jacobson JA, Girish G, Jiang Y, et al. Radiographic evaluation of arthritis: inflammatory conditions. Radiology. 2008;248:378–89. 1. MD, Resident of Radiology and Imaging Diagnosis, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 2. Associate Professor, Department of Radiology, School of Medicine – Universidade Federal do Rio de Janeiro (UFRJ), MD, Neuroradiologist, Grupo DASA, Rio de Janeiro, RJ, Brazil. 3. Full Professor of Radiology, Universidade Federal Fluminense (UFF), Niterói, RJ, Adjunct Coordinator, Course of Postgraduation in Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 4. Associate Professor, Department of Radiology, School of Medicine – Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. * Study developed in the Service of Radiology at Hospital Universitário Clementino Fraga Filho – Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. Mailing Address: Dr. Cristiano Gonzaga de Souza Rua Nossa Senhora do Carmo, 155, Vila Tereza Cataguases, MG, Brazil, 36772-016 E-mail: souzacataguases@gmail.com Received November 24, 2012. Accepted after revision January 18, 2013. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554