Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
ORIGINAL ARTICLE
|
|
Thyroid arterial embolization as a therapeutic option for hyperthyroidism: a case series |
|
|
Autho(rs): Josivan Gomes de Lima1; Alexandre Barbosa Câmara de Souza2; Raphael Pinto de Mendonça3; Lúcia Helena Coelho Nóbrega3; Fernando Antônio de Araujo Moura4; Zankennedy Jales de Queiroz5 |
|
|
Keywords: Hyperthyroidism; Treatment; Embolization. |
|
|
Abstract: INTRODUCTION
Hyperthyroidism, in most cases, is a chronic disease and common cause of goiter and exophthalmos(1). Among the therapeutic modalities, three are currently feasible, namely, antithyroid drugs, radioactive iodine and surgery(2,3). In spite of the lack of a global consensus on the initial therapeutic approach, pharmacological treatment with thionamides (methimazole or propylthiouracil) is considered in many countries as the first choice in the attempt to control in patients hyperthyroidism. The main obstacles to their use are represented by remission difficulties and possible side effects resulting from such treatment option. Thyroidectomy (whether subtotal or total) provides the possibility of definitive resolution of hyperthyroidism, but it may present complications caused by anesthesia, and fail in the control of the clinical condition (particularly in attempts of partial resection of the gland), besides being an invasive procedure involving risks for injuries to the recurrent laryngeal nerve and cervical vessels, and possibility of hypoparathyroidism. Currently, with improvements in operative techniques and in the knowledge on corticosteroid preparation for surgery, the complication rates have decreased(2). The radioactive iodine therapy causes actinic lesions which culminate in atrophy of the thyroid tissue. Such an effect, however, presents a variable response, depending upon several factors such as thyroid gland volume, dose delivered, dietary iodine content, previous utilization of iodinated contrast agents and thionamides for control, concomitance or not of utilization of antithyroid drug during iodine administration and gastrointestinal tract integrity(1-3). Main contraindications include pregnancy and lactation (absolute contraindications) and active Graves' ophthalmopathy classified as intense (relative contraindication). However, this definitive therapeutic procedure is widely utilized nowadays(2-7). In cases of side effects or contraindications for some specific therapy, the therapy by embolization, as already utilized in other organs (liver, uterus, etc.) may be a new modality for treating hyperthyroidism. In 2002, Xiao et al.(8) reported satisfactory results with the utilization of a new technique in an attempt to obtain temporary or definitive remission of hyperthyroidism activity: occlusive endovascular embolization of nourishing arteries of the thyroid tissue. Such study consisted in performing the occlusion of two of the four thyroid arteries in 22 patients with 27-month follow-up. Over the whole follow-up period, remission was observed 14 (63%) of the patients, with one patient presenting hypothyroidism, and the others requiring supplementary dose of radioactive iodine. In 2007, Zhao et al.(9) reported a remission rate of 78.6% in patients of another Asian center, over a 12-month follow-up period. In their series, such Asian centers reported a sustained hyperthyroidism, goiter and symptoms management with the mentioned technique(8,9). The present study was aimed at evaluating the therapeutic response of thyroid arteries embolization (TAE) in five Brazilian patients with hyperthyroidism and diffuse goiter after failure of conventional treatment. MATERIALS AND METHODS The study followed-up five hyperthyroidism patients who did not achieve remission over consecutive 24 months under treatment with thionamides (Table 1). The clinical and laboratory criteria for considering the failure of the pharmacological treatment were suppressed TSH (< 0.4 mUI/ml), free T4 and/or T3 levels above the reference range of normality, as well as presence of hyperthyroidism symptoms under pharmacotherapy (propylthiouracil or methimazole, with or without beta-blockers). Only patients with Graves' disease were included (patients with ophthalmopathy and/or TRAb - thyroid-stimulating hormone receptor antibody - positive). Patients with severe ophthalmopathy (activity score showing important injury of conjunctiva, corneas, extraocular muscles and/or optic nerve) were excluded. The patients were followed-up from September/2005 to December, 2006. 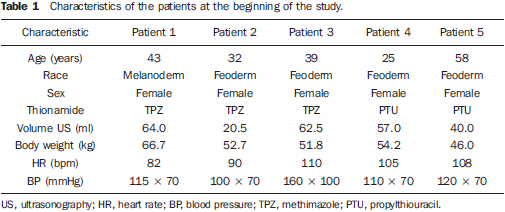 The study project was previously approved by the committee for Ethic in Research of the institution. All the patients signed a term of free and informed consent and were allowed to leave the investigation at any moment if they so wished. Pre-embolization evaluation Initially, all the patients were submitted to laboratory tests, comprising blood count, renal and hepatic function, whose results should be. Doppler ultrasonography of the thyroid arteries and plain chest radiography were performed before the procedure. The patients were submitted to volumetric measurement and evaluation of vascularization (by means of Doppler flowmetry) before and after the embolization procedure, for investigation of revascularization (in case it occurred). Thyroid artery embolization The patients received sedation with diazepine or thiopental, with heart rate monitoring. Intravenous antibiotic prophylaxis was performed with a single 2 mg cephalozine dose. Prophylactic heparinization (5,000 UI intravenously) was performed in some patients after arterial puncture in order to avoid hypercoagulability phenomena. The Seldinger technique was utilized for right transfemoral insertion, with series in both superior and inferior and lower thyroid arteries for angiography and embolization(10). Subsequently, angiographic contrast was utilized to identify the thyroid vascular anatomy coming from the thyrocervical trunk and from the external carotid arteries (Figure 1). 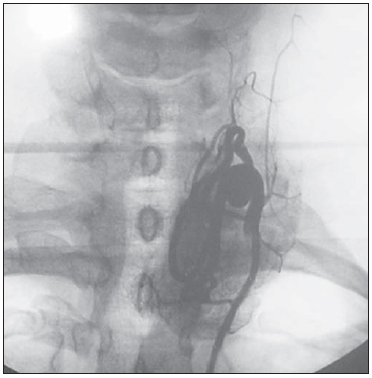 Figure 1. Angiography of left inferior thyroid artery. At the beginning of the procedure, hemodynamic angiography evaluated the patency and dominance of the arterial supply to the thyroid in order to perform the arterial occlusion of the most calibrous vessels, with embolization of the three largest arteries with polyvinyl-alcohol (150-300 μm in diameter), leaving the artery with the smaller diameter totally pervious. At the end of the procedure, a panoramic cervical angiography was performed, with iodinated contrast injection in the aortic arch to demonstrate the absence of thyroid blush. The femoral catheter was removed, with manual compression on the puncture site for 15 minutes, followed by bed rest for four to six hours. Prednisone 20 mg/day was initiated the day after the procedure and maintained for 7 days, and methimazole was reinitiated, at the same pre-procedural dose, 24 hours after the procedure and maintained until the fourth week after the procedure. The beta-blocker was maintained at a personalized dose until euthyroidism was reached. All the procedures were performed in a single unit, by a single interventional radiologist who followed a pre-established protocol. Post-procedural follow-up Calcemia and serum creatinine tests, besides monitoring of symptoms and hemodynamic changes were performed during the first 48 hours. Thereafter the patients underwent weekly clinical and laboratory evaluations over the first four weeks, and at the 8th, 16th, 20th and 24th weeks (Table 2), with thyroid ultrasonography being performed under basal conditions and then at the 1st, 8th, 16th and 24th weeks (Table 3). 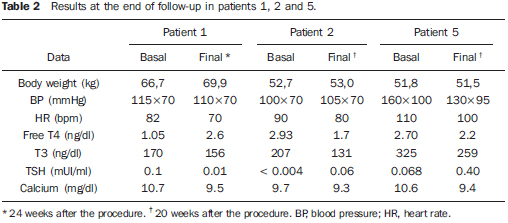 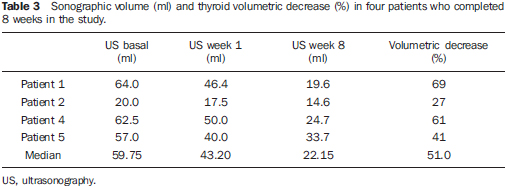 The laboratory tests were performed by chemiluminescence, with an Immulite 1000 Siemens apparatus, with the following reference levels: TSH, 0.4-4.0 mUI/ml; free T4, 0.8-2.2 ng/dl; total T3, 70-170 ng/dl. The primary objective was analyzing the responses regarding hyperthyroidism control, clinical and laboratorial remission, goiter volume decrease and prevention of complications in 24 weeks. Persistent hyperthyroidism would be treated with radioactive iodine, 12 to 15 mCi doses. The secondary objective was evaluating changes in thyroid function (hyper or hypothyroidism), besides identifying undesirable collateral effects from the procedure, such as embolization of a non-target organ, vascular dissection, phlebitic syndrome, aneurysm or pseudoaneurysm and hypoparathyroidism secondary to from parathyroid ischemia. RESULTS Five patients were submitted to the procedure, which had a mean duration of 77.4 ± 23.1 minutes. Two patients left the study protocol (patient 3 on the 4th week and patient 4 on the 12th week). Thus, only three patients underwent the pre-determined period on minimum follow-up (20 weeks) of the project. The initial data of the patients enrolled in the study, such as thyroid volume at ultrasonography (ml), weight (kg), heart rate (bpm) and arterial pressure (mmHg), are shown on Table 1. Data on weight (kg), arterial pressure (mmHg), heart rate (bpm), free T4 (ng/dl), T3 (ng/gl), TSH (mUI/ml) and calcium (mg/dl) levels in the patients before embolization and after follow-up are shown on Table 2. Size of the thyroid gland, basal volume and treatment progress after one and eight weeks are described on Table 3. Out of the five patients initially evaluated, only three completed a minimum postprocedural follow-up of 20 weeks. The whole study sample (five patients) could complete the follow-up only up to the 8th week. Before embolization, one patient (patient 3) presented more severe hypertension, one patient was intolerant to glucose (patient 1), and the others did not present any comorbidity. After embolization, all the patients presented subacute thyroiditis and, among the patients who completed the follow-up, even for the minimum of 16 weeks, or at the 24th week re-evaluation, none achieved complete hyperthyroidism remission, notwithstanding the significant reduction in the volume of goiter previously observed in all the patients. Clinical case 1 A 43-year-old, melanoderm, female patient followed-up at the endocrinology clinic for hyperthyroidism secondary to Graves' disease, undergoing 60 mg/day methimazole therapy. Upon admission, prediabetes was diagnosed. The patient was submitted to thyroid embolization, with no vascular complication (dissection, non-target organ embolization, aneurysms) (procedure shown on Figure 2). During hospital stay, diabetes was diagnosed and insulin therapy was initiated with an adjustment scheme according to capillary glycemia. Algic cervical syndrome was reported on the first week. No post-procedural infectious complication was observed. A noticeable aesthetic improvement was observed as a result from the decreased in goiter (Figure 3), as well improvement of the cervical compressive symptoms. After six months, ultrasonography demonstrated a 16.7 ml gland (Figure 4), with hypervascularization at Doppler analysis, even in previously embolized thyroid lobes. There were neither reports of visual disorders nor hyperglycemic complication. At the end of the follow-up, the patient was referred to a public nuclear medicine service for radioactive iodine therapy at a dose of 15 mCi, as previously determined by the protocol. 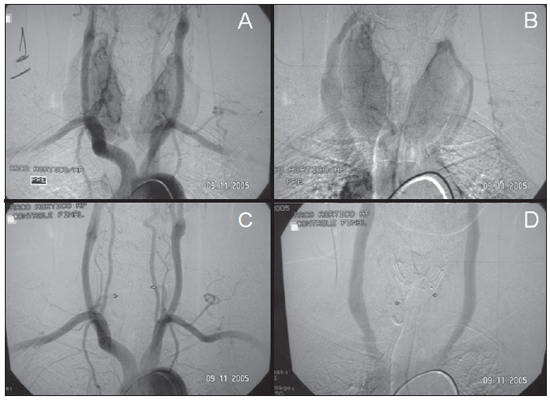 Figure 2. Patient 1. A: Preembolization image. B: Embolization with polynivyl alcohol particles. C,D: Post-embolization image. 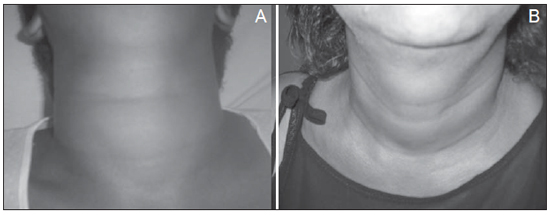 Figure 3. Patient 1. A: Diffuse thyroid goiter with 64 ml, before arterial embolization. B: Anterior cervical region 8 weeks after embolization, with 19 ml. 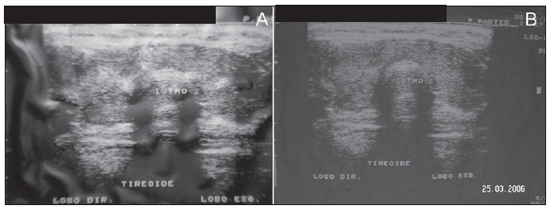 Figure 4. Patient 1. A: Preembolization ultrasonography, with a volume of 64 ml.; B: Ultrasonography after 16 weeks, with a volume of 16.7 ml (reduction of 73.9% in relation to pre-embolization volume). Clinical case 2 A 32-year-old, feoderm, female patient followed-up in the endocrinology clinic for hyperthyroidism secondary to Graves' disease, and under 60 mg/day methimazole therapy. At the admission for the procedure, the patient complained of insomnia, headache and weight loss. Embolization was performed and, during the procedure, the thyroid presented signs of anatomic variation, with five thyroid arteries being identified. Occlusion was performed in the three arteries with larger diameters. The procedure was successful, with no vascular complications (dissection, non-target organ embolization, aneurysms). The patient progressed without complaints, and reported improvement of initial symptoms. There was no report of visual disorders. After follow-up, the patient was referred to a reference public nuclear medicine service for radioactive iodine therapy at a dose of 15 mCi, as previously determined by the protocol. Clinical case 3 A 39-year-old, feoderm, female patient with hyperthyroidism secondary to Graves' disease, undergoing 60 mg/day methimazole therapy, and hypertensive, under 75 mg/day captopril. The patient was admitted into the service to undergo the procedure, with report of tremors, palpitations and weight loss. Embolization was performed, with no vascular complication (dissection, non-target organ embolization, aneurysm). After the procedure, the patient experienced a hypertensive peak, and was successfully treated with sodium nitroprusside, with no sequel. Appropriate blood pressure control was restored with 150 mg/day captopril. After the fourth week, follow-up of this patient was lost. Clinical case 4 A 25-year-old, feoderm, female patient undergoing follow-up in the endocrinology service for hyperthyroidism secondary to Graves' disease treated with propylthiouracil 100 mg/day. The patient reported insomnia, menstrual irregularity, tremors, palpitations and weight loss. Embolization was performed and, during the procedure, signs of anatomical variations were found with five thyroid arteries being identified. Occlusion was performed in the three arteries with larger diameters. There was no vascular complication (dissection, non-target organ embolization, aneurysm). In the post-operative period, the patient presented a hypertensive peak, and was treated with captopril, remaining stable and with no other complaints. Doppler analysis revealed hypervascularization at the 8th week, even in the previously embolized thyroid lobes. During the follow-up, the patient reported partial improvement of her initial complaints and quality of life, but the follow-up of this patient was lost after 12 weeks. Clinical case 5 A 58-year-old, feoderm, female patient referred to the endocrinology service for hyperthyroidism secondary to Graves' disease, undergoing treatment with 100 mg/day of propylthiouracil. The patient reported insomnia, weight loss, headaches, tremors and palpitations. Embolization was performed without vascular complications (dissection, non-target organ embolization, aneurysm). In the post-operative period the patient developed subacute thyroiditis which complicated with cachexia. Support treatment was instituted, with improvement of the algic symptoms, and the patient reported partial decrease of her initial complaints. There was no report of visual disorders. After the follow-up period, the patient was referred to a reference public nuclear medicine service for radioactive iodine therapy at a dose of 15 mCi, as previously determined by the protocol. DISCUSSION In the present study, after embolization of three thyroid arteries, a volumetric decrease was observed, besides management of the cervical symptoms caused by goiter in the patients with Graves' disease whose clinical treatment had failed. However, despite the aesthetic improvement reported by the patients, as well as improvements in cervical compressive symptoms, the serum TSH concentration did not reach the levels compatible with euthyroidism at the end of the protocol follow-up period (24 weeks for three patients). Additionally, there was a tendency towards increase in the free T4 levels, characterizing established hyperthyroidism. The persistence of the disease after the TAE procedure, has determined the necessity of treatment with radioactive iodine at the 15 mCi dose to control the hyperthyroidism as recommended in the study design. No sign of hypervascularization was found at the Doppler analysis, even in the previously embolized thyroid lobes in two of the five patients (patients 1 and 4) who underwent repeated ultrasonography at the end of the 8th week. A study has demonstrated that the expression of VEGF (vascular endothelial growth factor) is increased until six months after embolization, and is decreased after one year, suggesting a decrease of angiogenesis in the long term(11). Xiao et al.(8) have developed a study with 22 patients who refused treatment with radioactive iodine, and had severe side effects with thionamides or presented voluminous goiter. In such study, 14 patients achieved hyperthyroidism remission and goiter control in 50 months of follow-up. Later, two patients required use of thionamides and six, surgery (without complications) because of voluminous goiter persistence. No case of hypothyroidism was reported. Zhao et al.(9) have reported control of hyperthyroidism in patients with Graves' disease, with significant decrease in TRAb levels in 37 patients. In another study, those authors have found decrease in the CD4+/CD8+ ratio to normal levels at immunophenotyping(12). Indications on the elevation of post-immunohistochemical apoptosis parameters demonstrated a tendency towards volumetric decrease months after arterial occlusion(13). In a series with 28 patients, Zhao et al. have described euthyroidism in 78% of the patients in a 22-month follow-up period(10). On the other hand, Hiraiwa et al. have reported exacerbation of ophthalmopathy after TAE procedure(14). Some investigators have already initiated the utilization of TAE with a perspective of tumor reduction in patients with thyroid anaplastic carcinoma(15) or for tumor mass reduction, but published data on such utilization are still scarce(15-17). The present study had a small number of patients, which impairs comparative analysis with other studies. Additionally, the follow-up of two of five patients was lost. All the patients presented Graves' disease, and even in the absence of TRAb testing during the follow-up, the noticeable non-remission, even in 24 weeks, already demonstrated an ongoing autoimmune hyperthyroidism activity. In the present study, the follow-up demonstrated a rapid mean thyroid volumetric reduction of 49.5% of the thyroid parenchyma within 8 weeks after embolization, with a sustained response on the following eight weeks. Thus, from a primary observation, arterial embolization has offered satisfactory results for reduction of thyroid volume without the need for hyperfunction control of the organ. This fact can be corroborated by studies aimed at tumor mass reduction(15,16). The failure in controlling hyperthyroidism may have been a result of the irregularity of the utilized polyvinyl alcohol particles which microscopically were roughly "H"-shaped, perhaps favoring the recanalization of the thrombi located in the spaces of such "H", and also by the persistence of the blood flow in the remaining thyroid artery. In a normal functioning organ, smaller occlusive particles make the procedure more selective and effective. However, it should be considered that in a hyperstimulated organ, like in the case of Graves' disease, recanalization or neovascularization after embolization with smaller particles may occur, impairing the hyperthyroidism remission. Novel protocols with embolization of the four arteries with different sizes of occlusive particles, as well as the utilization of calibrated acrylate gel particles are being undertaken, and shall provide new data on such therapeutic modality in the control of hyperthyroidism. REFERENCES 1. Page S. Hipertireoidismo. In: Lima JG, Nóbrega LHC, Nóbrega MLC. Aulas em endocrinologia. Rio de Janeiro, RJ: Atheneu; 2001. p. 63-74. 2. Lima JG, Nóbrega LHC, Nóbrega MLC, et al. Fatores associados com recidiva precoce do hipertireoidismo após tratamento com radioiodoterapia. Arq Bras Endocrinol Metab. 2003;47:701-4. 3. Lopes MHC. Hipertireoidismo. In: Bandeira F, Macedo G, Caldas G, et al. Endocrinologia e diabetes. Rio de Janeiro, RJ: Medsi; 2003. p. 213-35. 4. Bonnema SJ, Bennedbaek FN, Veje A, et al. Continuous methimazole therapy and its effect on the cure rate of hyperthyroidism using radioactive iodine: an evaluation by a randomized trial. J Clin Endocrinol Metab. 2006;91:2946-51. 5. Bartalena L, Marcocci C, Bogazzi F, et al. Relation between therapy for hyperthyroidism and the course of Graves' ophthalmopathy. N Engl J Med. 1998;338:73-8. 6. Kerr L, Vidigal MEL, Rozenkwit D. Pode a gestação influenciar a evolução de nódulo tireoidiano maligno? Radiol Bras. 2012;45:65-6. 7. Brandão CDG, Antonucci J, Correa ND, et al. Efeitos da radioiodoterapia nas gerações futuras de mulheres com carcinoma diferenciado de tireóide. Radiol Bras. 2004;37:51-5. 8. Xiao H, Zhuang W, Wang S, et al. Arterial embolization: a novel approach to thyroid ablative therapy for Graves' disease. J Clin Endocrinol Metab. 2002;87:3583-9. 9. Zhao W, Gao BL, Tian M, et al. Graves' disease treated with thyroid arterial embolization. Clin Invest Med. 2009;32:E158-65. 10. Zhao W, Gao BL, Yi GF, et al. Thyroid arterial embolization for the treatment of hyperthyroidism in a patient with thyrotoxic crisis. Clin Invest Med. 2009;32:E78-83. 11. Zhao W, Gao BL, Liu ZY, et al. Angiogenic study in Graves' disease treated with thyroid arterial embolization. Clin Invest Med. 2009;32:E335-44. 12. Zhao W, Gao BL, Jin CZ, et al. Long-term immunological study in Graves' disease treated with thyroid arterial embolization. J Clin Immunol. 2008;28:456-63. 13. Zhao W, Gao BL, Yi GF, et al. Apoptotic study in Graves disease treated with thyroid arterial embolization. Endocr J. 2009;56:201-11. 14. Hiraiwa T, Imagawa A, Yamamoto K, et al. Exacerbation of thyroid associated ophthalmopathy after arterial embolization therapy in a patient with Graves' disease. Endocrine. 2009;35:302-5. 15. Tazbir J, Dedecjus M, Kaurzel Z, et al. Selective embolization of thyroid arteries (SETA) as a palliative treatment of inoperable anaplastic thyroid carcinoma (ATC). Neuro Endocrinol Lett. 2005;26:401-6. 16. Dedecjus M, Tazbir J, Kaurzel Z, et al. Selective embolization of thyroid arteries as a preresective and palliative treatment of thyroid cancer. Endocr Relat Cancer. 2007;14:847-52. 17. Dedecjus M, Tazbir J, Kaurzel Z, et al. Evaluation of selective embolization of thyroid arteries (SETA) as a preresective treatment in selected cases of toxic goitre. Thyroid Res. 2009;2:7. 1. Specialization in Endocrinology, Professor of Endocrinology at Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil. 2. Graduate Student of Medicine at Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil. 3. MDs, Endocrinologists, Centro de Endocrinologia de Natal, Natal, RN, Brazil. 4. MD, Interventional Radiologist, Hospital universitário Onofre Lopes da Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil. 5. MD, Radiologist, Hospital universitário Onofre Lopes da Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil. Mailing Address: Dr. Josivan Gomes de Lima Rua Joaquim Fabrício, 233, Petrópolis Natal, RN, Brazil, 59012-340 E-mail: josivanlima@gmail.com Received May 25, 2012. Accepted after revision December 3, 2012. * Study developed at Hospital universitário Onofre Lopes da Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554