INTRODUCTION
In the clinical practice, biliary obstruction is a frequent and severe situation, which can lead to generalized disease(1-3). Several conditions can trigger extrahepatic biliary obstruction with consequential cholestasis, both in humans and animals(4-6). Choledocholithiasis, neoplasia and stenosis present higher incidence(7).
The knowledge of normal anatomy and pathological imaging findings is fundamental for the detection of conditions in the hepatobiliary system(5,8,9). In the case of biliary obstruction, both biochemical and morphological changes occur, affecting the normal functioning of the liver(1,3,10,11). Therefore, the sonographic analysis of the hepatic and biliary morphometric parameters in the setting of biliary obstruction is very relevant, helping in the identification and evaluation of the obstruction site, contributing in the treatment of the patients.
The imaging evaluation, particularly by ultrasonography (US) of the liver and biliary tract has been the object of a number of recent articles in the Brazilian radiological literature(12-18). US represents the most utilized imaging method in the primary evaluation of patients with suspected biliary obstruction(4,8,9). Other imaging methods may also be utilized in the evaluation of the biliary tract, namely, radioisotope cholescintigraphy, computed tomography (CT), magnetic resonance imaging (MRI), trans-hepatic cholangiography, endoscopic retrograde cholangiopancreatography, or even radiography, oral cholecystography, and hepatic scintigraphy in some cases(4,7,9).
Bile duct injuries usually affect the upper part of the duct located close to the hepatic hilum, making it difficult to perform appropriate choledochoduodenal reconstruction(19). Additionally, injuries requiring biliary repair are commonly associated with long term complications, and the level of the injury and timing of repair are associated with the risk for post-surgical stenosis(20).
With the purpose of developing a more appropriate anatomical and physiological reconstruction for extensive biliary tract injuries, a study was proposed for reconstructing a bile duct by interposition of a "tube" constructed with a small bowel segment, similar to what Monti et al. have proposed for continent neobladder drainage(21). However, such a study requires an experimental model where one can induce jaundice with an obstructive pattern by ligating the extrahepatic bile duct, allowing for the analysis, evaluation and comparison of such changes in order to better understand the extent of the injury and the consequential compromising, as well as providing a previous knowledge on the surgical site, indicating specific techniques for, as a second step proposing the reconstruction of the extrahepatic bile duct.
The present study was aimed at inducing obstructive jaundice in pigs, by performing common bile duct ligation through videolaparoscopic surgery. The hepatic morphology histopathologically analyzed and the morphometry of the liver and the biliary tract evaluated at ultrasonography were compared before and seven days after the biliary obstruction. The changes observed in the animals were described, thus confirming the success of the procedure.
MATERIALS AND METHODS
The present experimental study was approved by the Committee for Ethics in Research of Faculdade Dr. Francisco Maeda (FAFRAM/FE) under No. 19/2008.
Experiment outline
For the present study, six 36-day-old pigs (
Sus scrofa domestica) of the Landrace race with mean weight of 9.17 (± 1.69) kg, originated from a single offspring, were utilized. Such animals were followed-up on and clinically evaluated on a daily basis since birth.
Pre- and post-obstruction sonographic evaluation
All the animals underwent ultrasonography scans on the day before the obstructive procedure, and post-obstruction scans were performed seven days after the procedure.
The animals under food and water fasting for six hours were sedated with acepromazine (0.2 mg/kg/intramuscular) and placed on a 50 cm surgical positioner. US was performed with the animal in dorsal decubitus, in the B-mode (SIUI CTS-310B apparatus, with a 5.0 MHz convex transducer), utilizing gel as acoustic coupling medium. For the purpose of comparative analysis, the following measurements were performed: major and minor longitudinal diameters of the left lateral hepatic lobe; major and minor cross-sectional and longitudinal diameters of the gallbladder; and the cross-sectional diameter of the choledochal duct on each animal. Additionally, the hepatic parenchyma and the abdominal cavity were analyzed in the search for any possible alterations. The images were printed and recorded on video and the obtained morphometric values were recorded on a table attached to the clinical records regarding each animal. Such adopted procedures were standardized, both for the pre-obstruction and the post-obstruction ultrasonography scans.
Anesthetic and surgical procedures
The preoperative procedures were common to all animals, which were submitted to food and water fasting for six hours prior to the procedure. Upon arrival at the hospital, the animals were given a cold shower bath for body cleansing and were sedated with acepromazine (0.2 mg/kg/intramuscular) and then had shaving and antisepsis of their ventral abdominal region. After the medication onset of action, the animals were taken to the surgical center. The medial saphenous vein was catheterized for glycophysiological solution infusion and administration of dissociative anesthetic based on the association of tiletamine and zolazepam (5.0 mg/kg/intravenous), and also fentanyl (0.025 mg/kg/intravenous) and atropine sulfate (0.5 mg/kg/intravenous). The anesthetic induction was maintained with the dose of one third to one half of the original dose of the dissociative anesthetic. During the surgical procedure, the animals received oxygen by means of a face mask.
Once the anesthetic plan was confirmed, the videolaparoscopic procedure was initiated (Karl Storz laparoscopic endoscope, with 15" LCD video display, 175 W xenon light source, 30.1 thermal insufflator and a three-chip camera), with a pre-umbilical median 1.0 cm incision, through which a Verres needle was inserted to perform the pneumoperitoneum with intracavitary pressure of 11 mmHg. Subsequently, four trocars were positioned as follows: two 5.0 mm trocars - one located at the caudal region to the right costal margin, and the other at the level of the right iliac fossa -, and two 10 mm trocars, - one located 1.0 cm pre-umbilical and one caudal to the left costal margin.
During the procedure, prehilar structures were identified, isolated and dissected and the laparoscopic ligation of the bile duct was performed as distally as possible with the purpose of producing total extra-hepatic obstructive jaundice. Once the ligation was completed, hemostasis was verified, the cavity was washed with preheated (37.5 C) physiological solution, the pneumoperitoneum was relieved, followed by surgical wound closure with 2-0 cotton thread and surgical skin closure with mononylon 3-0 thread.
Seven days after the procedure, post-obstruction US scan was performed and the animals were taken to the surgical center (utilizing the same anesthesia protocol as in the obstructive procedure), where pre-umbilical median laparotomy was performed for inspection of the abdominal cavity, removal of the bile duct ligation and consequently desobstruction of the duct.
Pre- and post-obstruction histopathological analysis
During the pre- and post-obstruction surgical procedures, specimens of the left lateral hepatic lobe from each animal were collected for histopathological analysis. Such specimens were identified and fixed in 3.7% formalin solution. The processing of such material was carried out in the General Pathology Department of Universidade Federal do Triângulo Mineiro, according to the protocol normally utilized by that Department. In order to avoid any bias, the histopathological slides received identification different from those utilized for the animals.
Postoperative care
In the postoperative period (obstruction and desobstruction) the animals remained under constant care, with follow-up on the surgical wounds healing and administration of anti-inflammatory drug (intramuscular dexamethasone - dose of 0.025 mg/kg/day), analgesic drug (intramuscular flunixin meglumine - dose of 2.2 mg/kg/day) and preventive antibiotic therapy (intramuscular enrofloxacin - dose of 2.5 mg/kg/day). The mean weight of the animals at the end of the experiment was 9.42 (± 2.19) kg.
Statistical analysis
The statistical analysis for comparison of the pre- and post-obstruction morphometric results was performed by utilizing the Sigma Stat 2.03 software. The verification of the normal variables distribution was carried out by means of the Kolmogorov-Smirnov test, where the continuous variables with normal distribution were analyzed by the paired
t-test for dependent samples, being such variables expressed in mean values and standard deviation, assuming as significance level a probability lower than 5% (
p < 0.05).
RESULTS
By utilizing only the portals described in the method, the main bile duct ligation was successfully performed without difficulties in all the animals, with easy identification of the bile duct during videolaparoscopic surgery. The most frequent signs presented by the animals seven days after the obstructive procedure were jaundice, bilirubinuria, fecal acholia and hepatomegaly at palpation.
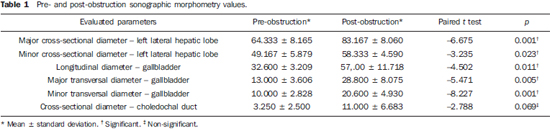
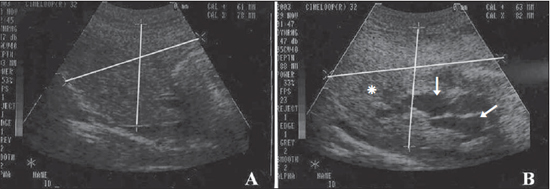
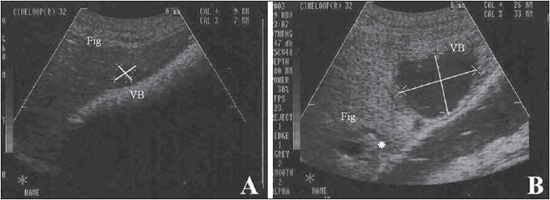
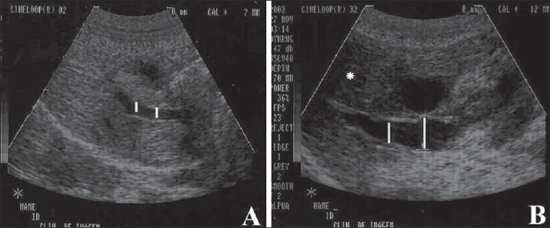
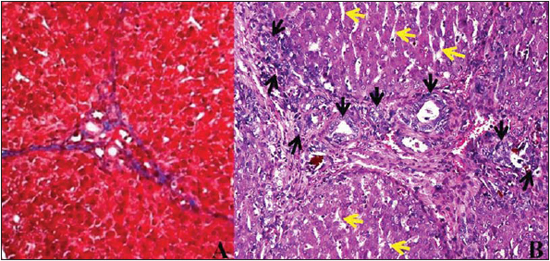
US performed seven days after the surgical obstruction revealed considerable and significant enlargement of the hepatic parenchyma (Figure 1; Table 1), as well as increased gallbladder diameter (Figure 2; Table 1). However, even with the biliary tract presenting considerable enlargement, such an enlargement was not significant in the case of the common bile duct (Figure 3; Table 1).
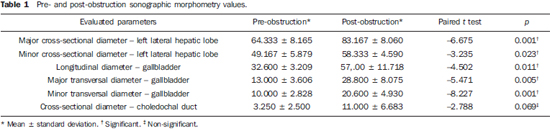
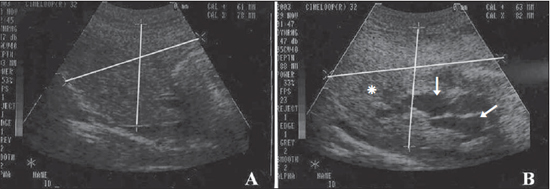
Figure 1. Sonographic images showing left lateral hepatic lobe (lines) of pigs experimentally submitted to biliary obstruction. On A, observe the pre-procedural normal longitudinal diameters; On B, observe the increased post-procedural longitudinal diameters. Also, observe the increased echogenicity of the hepatic parenchyma (asterisk) and dilation of intrahepatic biliary ducts on B (arrows).
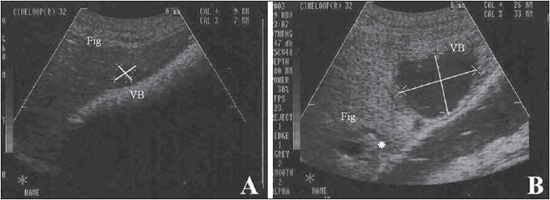
Figure 2. Sonographic images showing the gallbladder (lines) of a pig experimentally submitted to surgical biliary obstruction. On A, pre-obstruction crosssectional diameters; on B, post-obstruction cross-sectional diameters. On B, one observes increased gallbladder diameter, as well as increased echogenicity of the hepatic parenchyma (asterisk). (Fig., liver; VB, gallbladder).
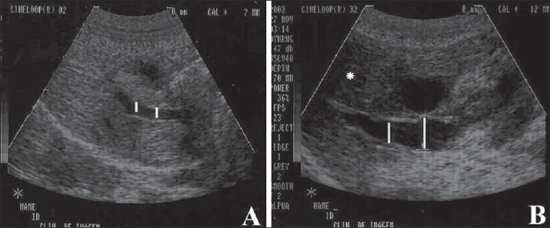
Figure 3. Sonographic images showing choledochal duct (lines) in a pig experimentally submitted to surgical biliary obstruction. On A, pre-obstruction longitudinal diameters; on B, post-obstruction longitudinal diameters. On B, one observes increased diameter of the choledochal duct, as well as increased echogenicity of the hepatic parenchyma (asterisk).
During laparotomy for reconstruction of the common bile duct by interposition of a tube (Monti's procedure), noticeable hepatomegaly was observed in the six animals, with the liver being felt firmer than normal, moderately pale and with a strong yellowish color. Also, increased caliber and consistency of the gallbladder and extra-hepatic biliary ducts were observed.
At histopathological analysis, as comparing pre-obstruction with post-obstruction specimens, presence of hyperplasia of the biliary ducts in the region of the portal space and dilation of the hepatic sinusoids was observed among other changes (Figure 4).
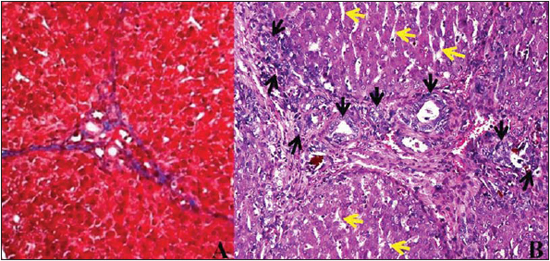
Figure 4. Photomicrography of left lateral hepatic lobe specimen from a pig experimentally submitted to biliary obstruction. On A, hepatic portal space in the preobstruction period; on B, postobstruction portal space with proliferation of biliary ducts (black arrows) and sinusoids dilation (yellow arrows). Hematoxylineosin staining, 320 × magnification.
For the present study, pigs (
Sus scrofa domestica) were utilized, because of their resistance, easy management and with good possibilities of standardization, frequently being utilized in experimental studies, and considered as appropriate animal models for the study of diseases related to the human life style(22,23). In the present study, the authors have observed that pigs represent an ideal type of experimental model since they develop obstructive jaundice within a short period of time.
The option for the videolaparoscopic surgery was justified for being the most utilized technique to approach biliary ducts, besides other advantages such as better acceptance by patients, smaller incisions, better aesthetic results, less postoperative pain, besides shorter hospital stay and low incidence of complications(2,19,24). In such a context, a more efficient surgical recovery of the animals was observed, since manipulating the animals for wound dressing is more practical and agile and the surgical wound healing is faster with less stress for the animals. Thus, the fast recovery allowed for the wellbeing of the animals and greater dedication of the team to the changes resulting from the obstructive procedure.
The experimental induction of extrahepatic cholestasis is not always a successful procedure(1). However, seven days after the obstructive procedure, the animals presented with signs compatible with those described for cholestasis in humans and animals(1,2,10,19). Thus it is possible to accept that both in humans and animals, when there is increase in the concentration of bilirubin in the blood circulation, deposition of such substance on tissues (jaundice) and glomerular excretion (bilirubinuria) are observed, while the decrease or absence of bilirubin excretion in the intestinal lumen causes changes in the color of the feces (acholia) which become lighter than normal(3,6,25). Therefore, the authors believe that pigs can be utilized as experimental surgical models for observation of obstructive jaundice.
Extrahepatic biliary tract
There is currently a wide variety of imaging techniques for evaluation of the biliary tract(4,6,9). Among such techniques, US is preferred by most professionals in the initial investigation on patients with suspected biliary conditions(4,6,8,9). The utilization of such technique is indicated in most abdominal diseases, and is totally non-invasive and essential for establishing diagnosis and approach in many situations(5,26,27). It has the advantage of being accessible, rapid, and innocuous, besides its bedside capability. Furthermore, it is a low cost method, does not rely on ionizing radiation or contrast utilization and does not require patient(4,26) or animal(5) sedation. In the present study, there were no difficulties in performing the ultrasonography scan on the animals, with easy and clear visualization of the liver and biliary tract.
Regardless of the gastrointestinal, hepatic or biliary function, US is appropriate for evaluation of both parenchymal organs and hollow viscera filled with fluid(26,27). Biliary system disorders can be easily detected at US(28,29). Because of its cost and convenience in association with high sensitivity and specificity, US is considered the best screening method in cases of lithiasis, detecting 95% of the calculi, and is also useful for visualizing choledochal dilatation(4,6,9,26), besides allowing, many times, the characterization of diseases developing outside the gallbladder(4). According to Zeman et al.(30), peripheral biliary dilatation can be diagnosed four hours after biliary obstruction, even before significant elevation of bilirubin serum levels and onset of jaundice. However, US presents limitations in the analysis of organs with gas content(26,27). Factors such as obesity and meteorism, among others, may impair a proper analysis and identification of the gallbladder, even in the presence of calculi(4), and fail in diagnosing calculi in the common bile duct, particularly in its terminal portion, where there is greater interposition of the duodenal gas content(5,9), thus the relevance of fasting prior the performance of ultrasonography. In the present study, water and food fasting was essential for a good visualization of the hepatic tissue and biliary tract.
A healthy gallbladder presents non echogenic content, with no echoes in its interior and thin, regular walls(4). Thus, ultrasonography allows the delineation of the anatomic texture of the gallbladder walls, with evaluation of parameters such as shape, size, motility and thickness of the wall, as well as the appearance of its content. It also allows the demonstration of dilated intra- and extrahepatic biliary ducts, helping in the differentiation between obstructive and non-obstructive jaundice(4,5,8,9,27). In the present study, the presence of calculi was not observed within the gallbladder, however, the increase in its diameter was observed as the pre- and post-obstruction images were compared.
Significant dilation of extrahepatic biliary ducts, with noticeable perception at ultrasonography has important diagnostic and prognostic value(4,5,30,31). Thus, although statistically significant difference has not been found in the diameter of the common bile duct in the present study, a considerable increase in diameter was observed above the obstructive ligation site, which demonstrates that the procedure was effective, confirming the biliary obstruction.
The dilation of the biliary tract evolves in a retrograde way after the complete obstruction of the common bile duct, so the observation of gallbladder enlargement and dilation of the ducts is frequent, particularly at their terminal portion(4,30,31). According to Nyland et al.(32), gallbladder and common bile duct enlargement is first seen, followed by extrahepatic bile duct dilation in the period between 24 and 48 hours; with distended intrahepatic ducts becoming visible five to seven days after complete biliary obstruction. However, as the biliary ducts dilate, their caliber may exceed the diameter of the portal vein branches, being visualized as parallel structures, showing the classical double duct sign(6,27). Thus, the identification of the obstructive site is based on the identification of the region above which the duct is dilated and below which the caliber is normal or non-identifiable.
The clear distension of the gallbladder is one of the first signs of complete biliary obstruction(30-32). Mwanza et al.(10), in a study involving obstruction of the common bile duct in dogs, have observed that the distension of the gallbladder was clearly seen within the first week after the ligation. Such a fact was also observed in the present study, since after seven days from the obstruction of the common bile duct a significant alteration could be clearly observed, with such distension also occurring because of the established cholestasis(3,10,32). However, Santo(2), evaluating the caliber of the main biliary duct in 67 human patients with choledocholithiasis, has verified that only 42 patients presented choledochal dilation. Liu et al.(33) have reported that the association of clinical, laboratory and sonographic criteria determine a sensitivity of 96% to 98% in the diagnosis of choledocholithiasis.
Thus, in dubious cases or those requiring more accurate information, or even for differential diagnosis, sonographic must be correlated with other diagnostic imaging methods and/or laboratory analyses(6,8,11). In the present study, the analysis of the biochemical profile of the animals was performed in the two periods, revealing the changes in serum levels which are directly related to biliary obstruction.
Liver
When there is an obstruction of the common bile duct, the drainage of the bile into the bowel does not happen, and it gradually accumulates in the ducts, bile canaliculi and hepatocytes which, consequently, dilate, inducing the increase in size of the liver. Such increase, on its turn, causes compression of hepatic cells and structures, which, in association with the degenerative processes caused by cholestasis, may progress to cellular death and, secondarily, to hepatic cirrhosis(3). In the present experiment, besides hyperplasia of bile ducts, the authors have observed collagen fibers stating to accumulate forming nodules characterizing the presence of early-stage hepatic cirrhosis.
According to Sullivan(9), at early stages of the cirrhotic process, the human cirrhotic liver is enlarged, with a relative enlargement of the lateral aspect of the left lateral lobe, a fact also observed in the present study, as when comparing the liver diameters measured before and after the obstructive procedure, the authors observed a significant increase in the volume of the animals' organ, later confirmed by histopathological analysis.
The determination of liver size is a common procedure in pediatrics routine, both for detecting hepatomegaly and for monitoring the progress of diseases or hepatic response to treatment(26,28,29). In case of suspicion of hepatomegaly,
in vivo liver measurements can be performed by means of clinical and/or imaging methods such as radiography, scintigraphy, US and CT(26). In the present study, significant results were obtained with ultrasonography as the moments of the experiment were compared, so such method may be utilized for evaluation of cholestasis.
According to Sullivan et al.(34), the clinical determination of the liver size is often inaccurate, and all studies relying um such parameters should be put under suspicion. Walk(35) also describes the evaluations by means of radiography as unsatisfactory. Thus, the utilization of more reliable methods for liver measurements is recommended, as a large liver is easily detectable, but smaller abnormalities may be underestimated(34). In such a context, US is considered a simple and quantitative method for assessment of liver size, being the first imaging study requested for such purpose(4,26), also in those cases of cholestasis associated with biliary obstruction(4,5).
The knowledge of the normal hepatic anatomy and of the pathological imaging findings of the lesions, is essential for their detection(8). At US, a healthy liver is seen with a smooth contour, and the hepatic parenchyma with a uniform and homogeneous echotexture, presenting echogenicity that is equal or slightly higher as compared with the spleen(5,11). US is a valuable method for evaluating the internal architecture of the liver(36), allowing a detailed study of the parenchyma, evaluating dimensions, shape, contour, borders, changes in echogenicity and appearance of vessels and hepatic structures, as well as its relationship with adjacent structures(5,26,37). However, one should be careful, as there are diseases which normally cause increased echogenicity of the hepatic parenchyma, without changes in the liver dimensions, which remain normal, such in fatty infiltration, steroid hepatopathy, diabetes mellitus, lymphoma and some toxic hepatopathies, while in cirrhosis and chronic cholangiohepatitis the liver generally presents reduced dimensions and irregular contour(3,5). Thus, the diffuse and increased echogenicity and insufficient definition of the portal vessels visualized on the animals' liver parenchyma can be attributed to cholestasis(4,11).
In certain cases, the sonographic appearance may be nonspecific(28), as observed by Mwanza et al.(10) who, by obstructing the common bile duct in dogs, reported little change in echogenicity of the liver parenchyma, even with jaundice, biochemical alterations and noticeable distension of the gallbladder at the first week after ligation. According to Sullivan(9), US, CT or MRI rarely detect early-stage diffuse hepatic diseases, diagnosing them only in cases where noticeable changes are observed in dimensions, density, and signal intensity, i.e., in advanced stages of the disease. In the present study, seven days of biliary obstruction were enough for the animals to develop changes which could be visualized at US, biochemical alterations and noticeable clinical signs of jaundice.
As a subjective and individual analysis is considered, differences may be observed in the interpretation of US findings. The diagnosis may be influenced by different factor such as the observer experience, type of apparatus and settings of depth, gain and contrast resolution. Concomitantly with hepatic alterations, several diseases may lead to alterations in other organs utilized for comparison of echogenicity and echotexture. Such alterations constitute additional factors that might impair the diagnosis(5,37). In such cases, the diagnosis can be substantially considered when the clinical signs are consistent(28) or by association with other diagnostic methods.
CONCLUSIONS
Considering the conditions in which the experiment was undertaken, it is possible to conclude that the pigs represent appropriate experimental models in the study of obstructive jaundice, as findings were observed at ultrasonography, biochemical and histopathological analysis. US allowed the visualization of significant hepatomegaly and cholecystomegaly, besides considerable enlargement of the common bile duct in the animals, demonstrating to be a sensitive and relevant method in the diagnosis of alterations resulting from extrahepatic biliary obstruction in such animals. Additionally, changes caused by cholestasis such as insufficient definition of the portal vessels and increased and diffuse echogenicity were perceptible.
REFERENCES
1. Prado IB, Santos MHH, Lopasso FP, et al. Cholestasis in a murine experimental model: lesions include hepatocyte ischemic necrosis. Rev Hosp Clín Fac Med S Paulo. 2003;58:27-32.
2. Santo MA. Litíase na via biliar principal: análise do tratamento cirúrgico por videolapascopia [tese]. São Paulo, SP: Faculdade de Medicina - Universidade de São Paulo; 2000.
3. Cotran RS, Kumar V, Robbins SL. Robbins: pathologic basis of disease. 7th ed. Philadelphia, PA: Elsevier; 2005.
4. Chammas MC, Marcelino ASZ, Saito OC, et al. Vesícula biliar. Ductos biliares. In: Lopes AC. Tratado de clínica médica. São Paulo, SP: Roca; 2006. p. 1217-32.
5. Nyland TG, Mattoon JS, Herrgesell EJ, et al. Fígado. In: Nyland TG, Mattoon JS. Ultra-som diagnóstico em pequenos animais. 2ª ed. São Paulo, SP: Roca; 2005. p. 95-130.
6. Franchi-Teixeira AR, Antoniali F, Boin IFSF, et al. Icterícia obstrutiva: diagnóstico laboratorial e de imagem. Medicina (Ribeirão Preto). 1997;30:198-208.
7. Dähnert W. Radiologia: manual de revisão. 3ª ed. Rio de Janeiro, RJ: Revinter; 2001.
8. Gunderman RB. Fundamentos de radiologia: apresentação clínica, fisiopatologia, técnicas de imagens. 2ª ed. Rio de Janeiro, RJ: Guanabara Koogan; 2007.
9. Sullivan LM. O fígado, o sistema biliar e o pâncreas. In: Juhl JH, Crummy AB, Kuhlman JE, editores. Paul & Juhl: interpretação radiológica. 7ª ed. Rio de Janeiro, RJ: Guanabara Koogan; 2000. p. 433-63.
10. Mwanza T, Miyamoto T, Okumura M, et al. Ultrasonographic evaluation of portal vein hemodynamics in experimentally bile duct ligated dogs. Jpn J Vet Res. 1998;45:199-206.
11. Biller DS, Kantrowitz B, Miyabayashi T. Ultrasonography of diffuse liver disease. A review. J Vet Intern Med. 1992;6:71-6.
12. Borges VFA, Diniz ALD, Cotrim HP, et al. Dopplerfluxometria da veia hepática em pacientes com esteatose não alcoólica. Radiol Bras. 2011;44:1-6.
13. Matsuoka MW, Oliveira IRS, Widman A, et al. Contribuição da ultrassonografia para o diagnóstico das alterações histopatológicas presentes na hepatite C crônica, com ênfase na esteatose hepática - Parte I. Radiol Bras. 2011;44:141-6.
14. Burke LMB, Vachiranubhap B, Tannaphai P, et al. Realce por contraste de lesões hepáticas em pacientes com cirrose: estudo cruzado comparativo de dois agentes de contraste para RM realizado em uma única instituição. Resultados preliminares. Radiol Bras. 2011;44:147-50.
15. Barbosa ABR, Souza LRMF, Pereira RS, et al. Espessamento parietal da vesícula biliar no exame ultrassonográfico: como interpretar? Radiol Bras. 2011;44:381-7.
16. Gössling PAM, Alves GRT, Silva RVA, et al. Bilioma espontâneo: relato de caso e revisão da literatura. Radiol Bras. 2012;45:59-60.
17. Souza LRMF, Rodrigues FB, Tostes LV, et al. Avaliação por imagem das lesões císticas congênitas das vias biliares. Radiol Bras. 2012;45:113-7.
18. Guimarães Filho A, Carneiro Neto LA, Palheta MS, et al. Doença de Caroli complicada com abscesso hepático: relato de caso. Radiol Bras. 2012;45:362-4.
19. Crema E, Silva AA, Lenza RM, et al. Excluded-loop hepatojejunal anastomosis with use of laparoscopy in late management of iatrogenic ligature of the bile duct. Surg Laparosc Endosc Percutan Tech. 2002;12:110-4.
20. Walsh RM, Henderson JM, Vogt DP, et al. Long-term outcome of biliary reconstruction for bile duct injuries from laparoscopic cholecystectomies. Surgery. 2007;142:450-7.
21. Monti PR, Lara RC, Dutra MA, et al. New techniques for construction of efferent conduits based on the Mitrofanoff principle. Urology. 1997;49:112-5.
22. Almond GW. Research applications using pigs. Vet Clin North Am Food Anim Pract. 1996;12:707-16.
23. Bustard LK, McClellan RO. Use of pigs in biomedical research. Nature. 1965;208:531-5.
24. Machado MAC, Herman P, Makdissi FF, et al. Ressecções hepáticas por videolaparoscopia: utilidade da técnica de Hemi-Pringle. Rev Bras Videocir. 2005;3:56-9.
25. Lassen ED. Avaliação laboratorial do fígado. In: Thrall MA. Hematologia e bioquímica clínica veterinária. São Paulo, SP: Roca; 2007. p. 335-43.
26. Rocha SMS, Oliveira IRS, Widman A, et al. Hepatometria ultra-sonográfica em crianças: proposta de novo método. Radiol Bras. 2003;36:63-70.
27. Cerri GG, Vogueira LAA. Ultra-sonografia em gastroenterologia. In: Mincis M. Gastroenterologia e hepatologia: diagnóstico e tratamento. 3ª ed. São Paulo, SP: Lemos Editorial; 2002. p. 45-53.
28. Nyland TG, Hager DA. Sonography of the liver, gallbladder, and spleen. Vet Clin North Am Small Anim Pract. 1985;15:1123-48.
29. Nyland TG, Hager DA, Herring DS. Sonography of the liver, gallbladder, and spleen. Semin Vet Med Surg (Small Anim). 1989;4:13-31.
30. Zeman RK, Taylor KJ, Rosenfield AT, et al. Acute experimental biliary obstruction in the dog: sonographic findings and clinical implications. AJR Am J Roentgenol. 1981;136:965-7.
31. Léveillé R, Biller DS, Shiroma JT. Sonographic evaluation of the common bile duct in cats. J Vet Intern Med. 1996;10:296-9.
32. Nyland TG, Gillett NA. Sonographic evaluation of experimental bile duct ligation in the dog. Vet Radiol. 1982;23:252-60.
33. Liu TH, Consorti ET, Kawashima A, et al. The efficacy of magnetic resonance cholangiography for the evaluation of patients with suspected choledocholithiasis before laparoscopic cholecystectomy. Am J Surg 1999;178:480-4.
34. Sullivan S, Krasner N, Williams R. The clinical estimation of liver size: a comparison of techniques and an analysis of the source of error. Br Med J. 1976;30:1042-3.
35. Walk L. Quantitative method to determine the liver size. Radiologe. 1978;18:354-5.
36. Lamb CR. Ultrasonography of the liver and biliary tract. Probl Vet Med. 1991;3:555-73.
37. Zwiebel WJ. Sonographic diagnosis of diffuse liver disease. Semin Ultrasound CT MR. 1995;16:8-15.
1. Master, Teacher, Course of Veterinary Medicine, Faculdade Dr. Francisco Maeda (FAFRAM/FE), Ituverava, SP, Brazil.
2. Students, Program of Advanced Studies of Veterinary Practice and Surgery, Faculdade Dr. Francisco Maeda (FAFRAM/FE), Ituverava, SP, Brazil.
3. Master, Associate Professor, Faculdade de Medicina da Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil.
4. MD, Radiologist, Radiology Department of Santa Casa de Misericórdia de Ituverava, Ituverava, SP, Brazil.
5. PhD, Associate Professor, Faculdade de Medicina da Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil.
6. PhD, Teacher, Course of Veterinary Medicine at Faculdade Dr. Francisco Maeda (FAFRAM/FE), Ituverava, SP, Brazil. (In memoriam).
Mailing Address:
Edmilson Rodrigo Daneze
Avenida Primeiro de Maio, 930, Vila Virgínia
Ribeirão Preto, SP, Brazil, 4030-390
E-mail: eddaneze@hotmail.com
Received October 20, 2012.
Accepted after revision January 18, 2013.
* Study developed at Faculdade Dr. Francisco Maeda (FAFRAM/ FE), Ituverava, SP, Brazil.
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013