INTRODUCTION
Recently, the imaging evaluation of the musculoskeletal system has motivated a series of studies published in the Brazilian radiological literature(1-10).
Intersection syndrome of the forearm (ISF) is an inflammatory process of the tendons of the second extensor compartment (extensor carpi radialis brevis and extensor carpi radialis longus) generally caused by direct local trauma or activities requiring repeated flexion and extension of the wrist (11-13).
It is clinically characterized by pain in the dorsal aspect of the forearm and the wrist, and edema proximal to the Lister's tubercle. A careful physical examination and appropriate clinical workup limit the hypotheses to a relatively small number of differential diagnoses, principally De Quervain's tenosynovitis. Magnetic resonance imaging (MRI) is a fundamental tool for the diagnosis of such a common, but not frequently diagnosed syndrome(11-13).
The authors present, in the form of an iconographic essay, MRI findings and discuss the most relevant differential diagnoses.
MRI PROTOCOLS
The images were acquired in a 1.5 T (Magnetom Avanto; Siemens Medical Systems, Erlagen, Germany) and a 3 T (Magnetom Trio; Siemens Medical Systems, Erlagen, Germany) apparatuses, with surface coils.
The following pulse sequences were utilized: axial and coronal T1-weighted sequences, as well as axial, coronal and sagittal DP with fat suppression before and after intravenous paramagnetic contrast injection (gadolinium, 0.1 mmol/kg of weight).
ANATOMY (Figures 1, 2 and 3)
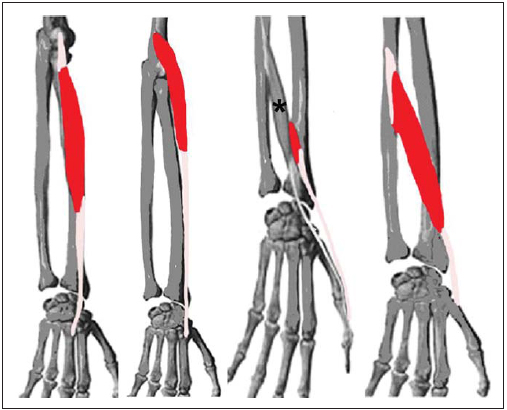
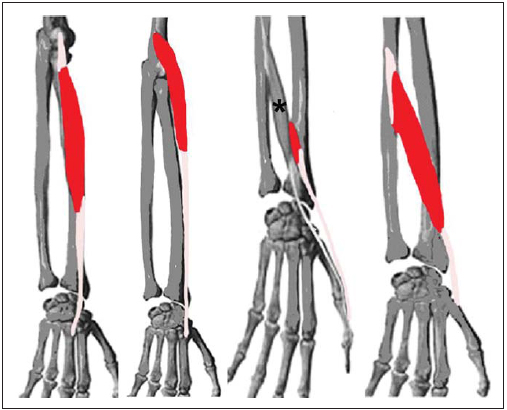
Figure 1. Schematic drawing showing the anatomy of the forearm muscles involved in the intersection syndrome. Muscle belly in red and origin and muscles insertion in pink. From left to right: extensor radialis carpi brevis, extensor radialis carpi longus, extensor pollicis brevis and abductor pollicis longus. Asterisk: extensor pollicis longus.
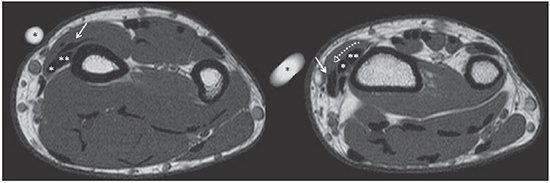
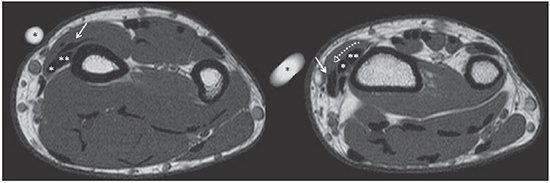
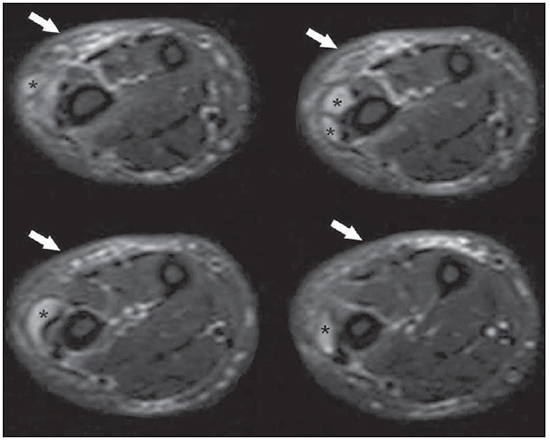
Figure 2. Axial, T1-weighted sequences at the level of the distal third of the forearm on the first intersection of the extensor tendons. Abductor pollicis longus and extensor pollicis brevis muscles (arrow) cross (dashed arrow) the extensor carpi radialis longus (white asterisk) and extensor carpi radialis brevis muscles (white double asterisk). Skin marker (black asterisk).
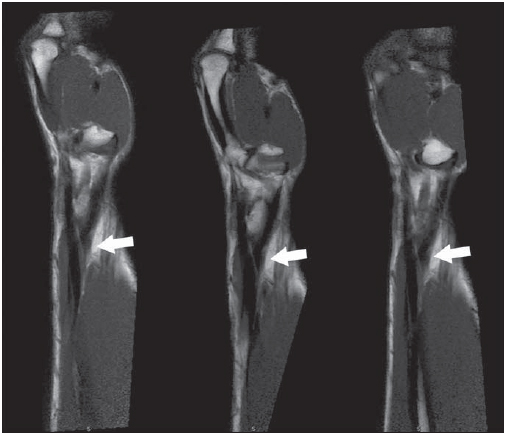
Figure 3. Proton density-weighted sequences with fat suppression in the oblique sagittal plane, demonstrating the intersection (arrow) of the tendons of the first and second compartments.
The extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) muscles act synergically with the finger flexor muscles for wrist flexion. The first one covers the latter, and originates from the supracondylar crest of the humerus, but some fibers come from the common extensor tendon of the forearm. It ends at a flattened tendon which deeply follows the deep extensor muscles of the forearm, abductor pollicis longus muscle (APL) and the abductor pollicis brevis muscle (APB). The ECRB originates from the lateral epicondyle of the humerus, through a common tendon with the common extensor muscle of the fingers and ends at a flattened tendon which follows the ECRL. It inserts into the dorsal surface of the base of the second and third metacarpal bones. Such two tendons cross the same compartment of the extensor retinaculum in a single synovial sheath and may unfold into two or three fascicles, or may join together or exchange muscle fascicles(14).
The abductor pollicis longus muscle (APL) and the abductor pollicis brevis muscle (APB) represent the principal deep extensor muscles of the forearm involved in the ISF. The APL originates from the posterior surface of the ulnar diaphysis, below the anconeus, the interosseous membrane and the middle third of the posterior surface of the radius, and follows inferolaterally, becoming superficial at the distal segment of the forearm, and visible as an oblique relief. It ends in tendon which becomes devoid of muscle fibers proximally to the wrist, which runs in a lateral groove together with the APB tendon. The tendon generally unfolds into two components, one inserting into the radial aspect of the base of the first metacarpal bone, and the other into the trapezoid bone. The APB is medially and inferiorly located in relation to the APL and originates from the posterior surface of the radius. Its direction is similar to that of the APL and its tendon inserts into the dorsal surface of the proximal phalanx of the hallux. In the lower third of the forearm, the APL and the APB become superficial, and then obliquely cross the tendons of the extensor carpi radialis, cover the termination of the brachioradialis muscle and, while crossing the most lateral compartment of the extensor retinaculum in a single synovial sheath, superficially cross the radius styloid process and the radial artery(14).
DISCUSSION
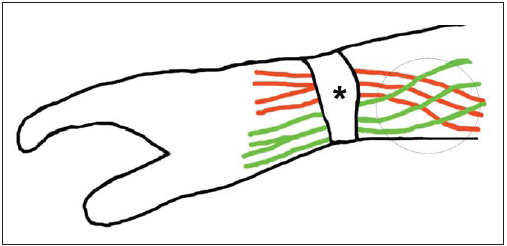
ISF, a not often diagnosed cause of pain on the dorsal aspect of the wrist, is a noninfectious inflammatory process affecting the dorsal aspect of the forearm, about 4 to 8 cm proximal to the Lister's tubercle(12,13). Also known as crepitating peritendinitis, cross syndrome, subcutaneous perimyositis, bursitis of the abductor pollicis longus, oarsman's wrist, bugaboo forearm, among others(11-16), this syndrome was described by Velpeau in 1841, however the term "intersection syndrome" was introduced by Dobyns et al. in 1978 and defined as an inflammatory process of the tendons of the second extensor compartment of the forearm (ECRB and ECRL), generally caused by direct local trauma or activities that require repeated flexion and extension of the wrist. Such activities may be sport activities such as rowing, canoeing, racket games, weight lifting, ski and horse riding, or labor activities such as those of farmers, carpenters or secretaries(13). It is most prevalent in young adults (mean age of 39.3 years) regardless of gender(12). The physiopathology of this condition is uncertain, but two theories have been described. The first theory, proposed by Howard in 1937, reports that the friction between the muscle bundles of the APL and APB and the synovial sheath of the second compartment would be responsible for the genesis of the disorder (Figure 4). The other theory, de-scribed in 1985 by Grundberg et al., suggested that the genesis of the process would be a stenosing tenosynovitis of second dorsal compartment, with extension of the inflammatory process to adjacent soft tissues. (13,16)
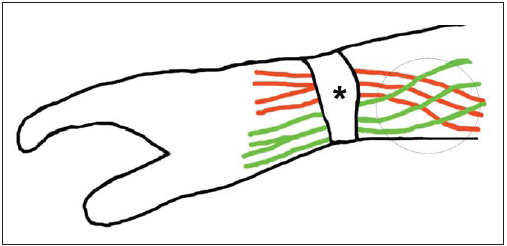
Figure 4. Schematic drawing showing forearm anatomy, indicating the intersection point (circle) of the extensor radialis longus and extensor carpi radialis brevis (in orange) with the tendons of the abductor pollicis longus and extensor pollicis brevis (in green) muscles, and their pathways through the extensor retinaculum (asterisk).
Clinical manifestations include phlogistic signs on the dorsal aspect of the wrist, typically between 4-8 cm proximal to the Lister's tubercle, with functional limitation and crepitation at wrist movements, present in more severe cases(11-13).
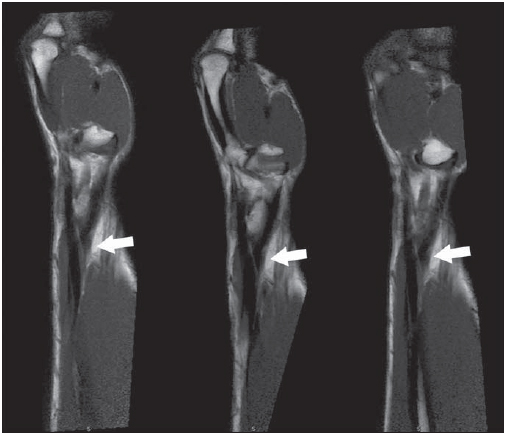
Ultrasonography and MRI are extensively applied methods, both in athletes or in non athletes, for evaluation of musculoskeletal lesions(17-19). In ISF, MRI is the main diagnostic method and the findings include peritendinous edema around the first and second extensor compartments, at the level of their intersection, with fluid surrounding the tendons and in their sheaths or between them, notably at the level of the intersection point (Figures 5 and 6). Additional findings include tendinosis, muscle and subcutaneous edema(11). The utilization of gadolinium is questionable, since T2-weighted sequences can easily identify the findings of intersection syndrome; but, when utilized, the peritendinous enhancement is intense(11-13,20). It is important to utilize skin markers, and the extent of the field of view (FOV) must proximally cover the area of intersection(11-13,20). The axial plane is most appropriate for diagnosis(12,13), however, a sagittal oblique plane oriented towards the tendinous intersection provides more details than the standard sagittal plane(12,13).
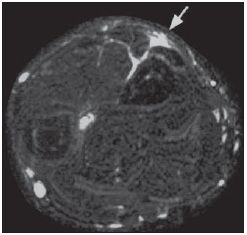
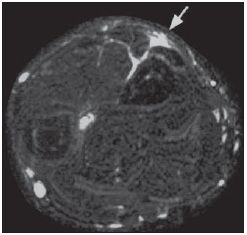
Figure 5. Intersection syndrome of the forearm. Male, 30-year-old patient, tennis player, presenting focal increase of soft tissues in the distal forearm. Proton density- weighted sequence with fat suppression in the axial plane shows subcutaneous and peritendinous edema on the intersection point of the first and second extensor compartment tendons (arrow).
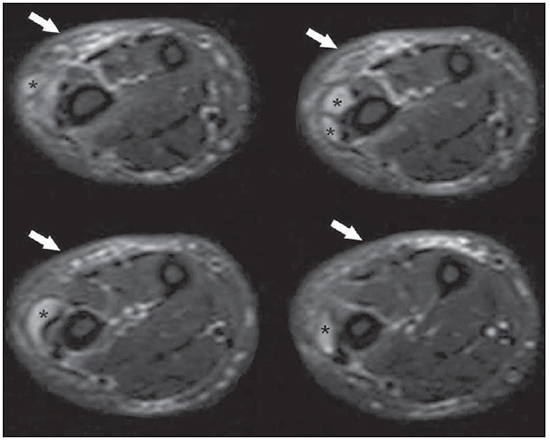
Figure 6. Intersection syndrome of the forearm. Male, 55-year-old patient, swimmer, presenting pain and edema in the dorsal surface of the forearm. Proton density-weighted sequence with fat suppression in the axial plane shows marked edema of peritendinous soft tissues (arrows) as well as presence of fluid collection (asterisks) in the intersection point of the first and second extensor compartment tendons.
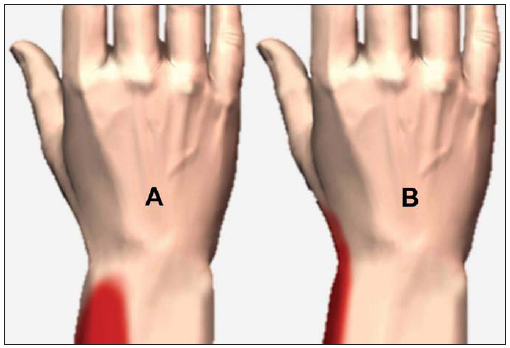
De Quervain's tenosynovitis is the main differential diagnosis (Figure 7), corresponding to a stenosing tenosynovitis of the first extensor compartment, generally occurring several centimeters below the tendinous intersections. The Finkelstein's test at physical examination is pathognomonic of such a condition. The MRI findings described by Glajchen et al. include increased thickness of the tendon inside the first extensor compartment at the level of the radius distal extremity and increased signal intensity within the synovial sheath, indicating tenosynovitis. Subcutaneous edema is found in some patients(20).
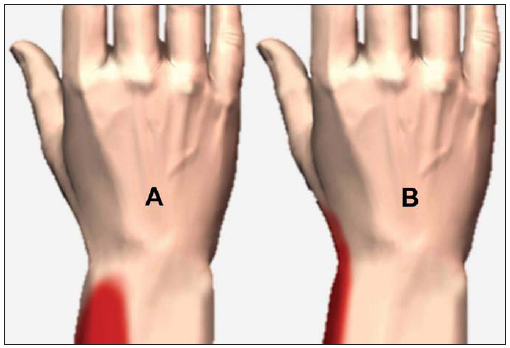
Figure 7. Schematic drawing of the differential topognosis between intersection syndrome (A) and De Quervain's tenosynovitis (B).
Other hypotheses considered in the differential diagnosis include ligament lesions, tendinosis, tenosynovitis, cystic ganglions, soft tissue tumors, infection, Wartemberg's syndrome (a sensitive neuropathy involving the superficial branch of the radial nerve), cellulitis and muscle strain(11-13).
The treatment is initially conservative with non-steroid anti-inflammatory drugs. Surgery for decompression of the intersection area is only performed on those patients who are refractory to conservative treatment(13,15).
CONCLUSION
MRI is the method of choice in the investigation of ISF and its differential diagnoses, as the clinical evaluation is usually not diagnostic. Radiologists must be attentive to some details during the scan and to the findings which characterize ISF.
REFERENCES
1. Chojniak R, Grigio HR, Bitencourt AGV, et al.Biópsia percutânea por agulha grossa de tumores de partes moles guiada por tomografia computadorizada: resultados e correlação com análise da peça cirúrgica. Radiol Bras. 2012;45:259-62.
2. Cotta AC, Melo RT, Castro RCR, et al. Dificuldades diagnósticas no osteoma osteoide do cotovelo: estudo clínico, radiológico e histopatológico. Radiol Bras. 2012;45:13-9.
3. Tavares Júnior WC, Faria FM, Figueiredo R, et al. Fadiga óssea: causa de dor em joelhos na osteoartrite. Radiol Bras. 2012;45:273-8.
4. Moura MVT. Interposição de fragmento periosteal na fratura da placa epifisária femoral distal: estudo por ressonância magnética. Radiol Bras. 2012;45:184-6.
5. Ribeiro DS, Araújo Neto C, D'Almeida F, et al. Achados de imagem das alterações musculoesqueléticas associadas ao lúpus eritematoso sistêmico. Radiol Bras. 2011;44:52-8.
6. Nunes RB, Amaral DT, Oliveira VS. Propedêutica radiológica do impacto femoroacetabular em tempos de tomografia computadorizada e ressonância magnética: o que o radiologista precisa saber. Radiol Bras. 2011;44:249-55.
7. Simão MN, Nogueira-Barbosa MH. Ressonância magnética na avaliação das variações anatômicas meniscais e da anatomia ligamentar perimeniscal: potenciais causas de erro de interpretação. Radiol Bras. 2011;44:117-22.
8. Simão MN, Helms CA, Richardson WJ. Magnetic resonance imaging findings of disc-related epidural cysts in nonsurgical and postoperative microdiscectomy patients. Radiol Bras. 2012;45:205-9.
9. Jacob Jr C, Barbosa DM, Batista PR, et al. Fratura toracolombar do tipo explosão: o que o radiologista deve conhecer. Radiol Bras. 2012;45:101-4.
10. Grassi CG, Diniz FV, Garcia MRT, et al. Aspectos de imagem na tendinite calcária pré-vertebral. Radiol Bras. 2011;44:327-30.
11. Costa CR, Morrinson WB, Carrino JA. MRI features of intersection syndrome of the forearm. AJR Am J Roentgenol. 2003;181:1245-9.
12. Lee RP, Hatem SF, Recht MP. Extended MRI findings of intersection syndrome. Skeletal Radiol. 2009;38:157-63.
13. de Lima JE, Kim HJ, Albertotti F, et al. Intersection syndrome: MR imaging with anatomic comparison of the distal forearm. Skeletal Radiol. 2004;33:627-31.
14. Caetano MBF, Albertoni WM, Caetano EB. Estudo anatômico das inserções distais do tendão extensor longo do polegar. Acta Ortop Bras. 2004;12:118-24.
15. Hanlon DP, Luellen JR. Intersection syndrome: a case report and review of the literature. J Emerg Med. 1999;17:969-71.
16. Parellada AJ, Gopez AG, Morrison WB, et al. Distal intersection tenosynovitis of the wrist: a lesserknown extensor tendinopathy with characteristic MR imaging features. Skeletal Radiol. 2007;36:203-8.
17. Barbosa LH, Gil Coury HJC. A atividade do médico ultra-sonografista apresenta riscos para o sistema músculo-esquelético? Radiol Bras. 2004;37:187-91.
18. Silva HR, Simão MN, Elias Jr J, et al. Diagnóstico por imagem nas síndromes do estalido ou do ressalto. Radiol Bras. 2009;42:49-55.
19. Cunha GM, Marchiori E, Ribeiro EJ. Avaliação ultra-sonográfica da articulação do ombro em nadadores de nível competitivo. Radiol Bras. 2007;40:403-8.
20. Timins ME, O'Connell SE, Erickson SJ, et al. MR imaging of the wrist: normal findings that may simulate disease. Radiographics, 1996;16:987-95.
1. MD, Radiologist, Clínica Medimagem, Cachoeiro de Itapemirim, ES, Brazil.
2. MDs, Radiologists, Clínica de Diagnóstico Por Imagem (CDPI)/MD.X, Rio de Janeiro, RJ, and Centro de Diagnóstico por Imagem Fátima Digittal, Nova Iguaçu, RJ, Brazil.
3. MD, Radiologist, Clínica de Diagnóstico Por Imagem (CDPI), Rio de Janeiro, RJ, Brazil.
Mailing Address:
Dr. Claudio Marcio Amaral de Oliveira Lima
CDPI/MD.X Barra Medical Center
Avenida das Américas, 6205, Loja G e subsolo, Barra da Tijuca
Rio de Janeiro, RJ, Brasil, 22793-080
E-mail: cmaolima@gmail.com/antoniocoutinhojr@yahoo.com.br
Received November 6, 2012.
Accepted after revision December 21, 2012.
* Study developed at Clínica de Diagnóstico Por Imagem (CDPI)/MD.X, Rio de Janeiro, RJ, Brazil.
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013