Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 1 - Jan. /Feb. of 2013
Vol. 46 nº 1 - Jan. /Feb. of 2013
|
CASE REPORT
|
|
Dysplasia epiphysealis hemimelica (Trevor-Fairbank disease): case report |
|
|
Autho(rs): Regina Bosenbecker da Silveira1; Felipe Augusto Rozales Lopes2; Ana Luiza Behrensdorf Reis3; Enrico Granzotto4; André Guimarães de Oliveira2 |
|
|
Keywords: Epiphysis; Osteochondrodysplasia; Dysplasia epiphysealis hemimelica; Trevor disease. |
|
|
Abstract: INTRODUCTION
Dysplasia epiphysealis hemimelica (DEH) is defined as a localized osteochondral overgrowth arising from half of an epiphysis and affecting either one or several epiphyses or ossification centers(1-3). It is an abnormal and asymmetrical proliferation of cartilage with osteochondral ossification which ceases once the growth process is completed(3). It is a rare disease, with a reported incidence of 1:1.000.000, whose etiology still remains unknown. However, it is known that such condition is connected with the group of osteochondromatoses(1,2). Because of such disease rarity, there is a scarcity of cases described in the literature, hence the authors' objective of presenting the case of a three-year-old boy with DEH in his right knee. CASE REPORT A male, three-year-old patient presented pain and edema in his right knee for three days. Along the previous two months the patient presented abnormality in gait, more significantly when running. At physical examination, a moderate swelling and local warmth were observed, with pain and flexion limitation. At radiography, irregularities on the articular surfaces with exuberant calcifications were observed in the articular space and adjacent to the distal femoral and proximal tibial epiphyses (Figure 1). 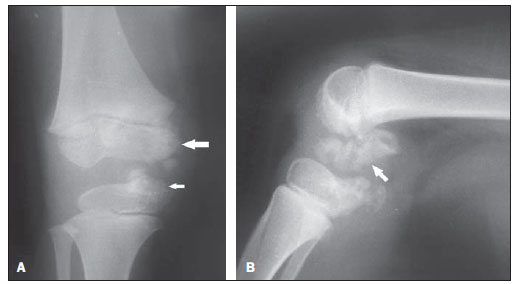 Figure 1. A: Anteroposterior radiograph demonstrating irregularities on articular surfaces with calcifications adjacent to the distal femoral (large arrow) and proximal tibial (small arrow) epiphyses. B: Lateral radiograph of knee identifying exuberant calcifications in the articular space (arrow). Computed tomography (CT) revealed the presence of moderate joint effusion with irregularity in the contours of the femoral condyle and tibial plateau in the medial compartment, and multiple, irregular calcifications within the joint, particularly on the posterior aspect of the femur. Magnetic resonance imaging (MRI) demonstrated irregularities and dysplastic alterations on articular surfaces of the medial femoral condyle and internal tibial plateau, with calcifications and adjacent intrasynovial ossifications (Figure 2). 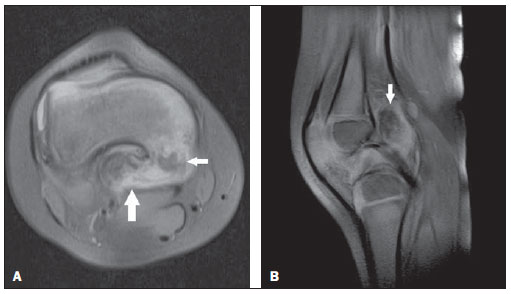 Figure 2. A: Axial MRI proton-density-weighted fat sat image demonstrating involvement of the distal femur by the disease, with irregularities, dysplastic alterations (small arrow), calcifications and intra-articular ossification (large arrow). B: Sagittal MRI proton-density-weighted fat sat image showing the presence of calcifications and intrasynovial ossification (arrow). Soft tissue preservation is also observed. Surgical excision of the lesion was performed because of the significant functional limitation and pain. Anatomopathological analysis revealed osteochondroma. DISCUSSION DEH - also known as Trevor-Fairbank disease - generally affects children in the age range between 2 and 14 years and is most frequent in boys. Generally with unilateral involvement, the lesion originates a tone of the epiphyseal aspects, preferentially affecting the lower limbs, in decreasing order of occurrence: knee, ankle and foot(4,5). Initially the clinical presentation corresponds to local painless swelling determined by the cartilage overgrowth, which may become painful and generate deformities, limited range of motion and limb length discrepancy(1,6). According to Peduto et al., the diagnosis is based on radiographic findings(1), and biopsy is not required, except in case of surgical excision of the lesion or in the presence of atypical radiological findings(5). Histologically, the lesion characteristics are identical to those of osteochondroma(2). According to Carlson et al., the osteocartilaginous overgrowth of DEH, originated from the epiphysis, must not be confused with exostosis originated from the metaphysis. Such authors describe the following differential diagnoses: chondrodysplasia punctata and multiple epiphyseal dysplasia, which occur bilaterally, and areas of asceptic necrosis presenting irregularities, but without any characteristic of osteochondral overgrowth(6). Radiography shows one or more irregular masses with focal ossification adjacent to the border of one of the halves of the epiphysis (with overgrowth), with irregular enlargement of epiphyseal centers and adjacent metaphysis, like in the present case, where the lesion was adjacent to the distal femoral and proximal tibial epiphyses. Such mass may be located on the underlying bone in cases where bone maturation is present(1,2,6). CT can more accurately define the anatomical relationship between the mass and the bone, as well as the continuity of the bone cortical and bone marrow, but it is inferior to MRI in the evaluation of changes in cartilage and soft tissues(1,2). With MRI, one can better evaluate the epiphyseal osteochondral growth and its probable effects on adjacent structures, allowing a better definition of bone and cartilage structures at multiple planes, but scarce reports describing MRI findings of DEH are found in the literature(1,2,7). MRI is useful at early phases of the disease, when a small mass with calcifications inside is observed, likewise in the present case(1,2). At the T1-weighted sequence, the signal intensity is the same for both the healthy epiphyseal cartilage and the cartilage affected by disease, but the latter presents small spots of low intensity corresponding to calcifications. On the other hand, at T2-weighted sequences, the higher intensity is observed in the cartilaginous cap as compared with the osteocartilaginous junction(8). As regards treatment, radiographic follow-up is performed to evaluate the lesion progression. In cases of pain, skeletal deformities or functional limitations, surgical excision is indicated(2). Follow-up is required to evaluate lesion recidivation after surgery(2,3). Finally, DEH is a rare disease characterized by asymmetrical epiphyseal overgrowth, whose diagnosis is made by means of radiography, supplemented by MRI which can better evaluate the osteochondral overgrowth as well as adjacent structures. REFERENCES 1. Peduto AJ, Frawley KJ, Bellemore MC, et al. MR imaging of dysplasia epiphysealis hemimelica: bony and soft-tissue abnormalities. AJR Am J Roentgenol. 1999;172:819-23. 2. Araujo CR Jr, Montandon S, Montandon C, et al. Best cases of the AFIP: dysplasia epiphysealis hemimelica of the patella. Radiographics. 2006;26:581-6. 3. Bansal P, Khare R, Lal H, et al. Dysplasia epiphysealis hemimelica or Trevor's disease of proximal tibia mimicking loose body. J Clin Orthop Trauma. 2010;1:105-6. 4. Wiart E, Budzik JF, Fron D, et al. Bilateral dysplasia epiphysealis hemimelica of the talus associated with a lower leg intramuscular cartilaginous mass. Pediatr Radiol. 2012;42:503-7. 5. Rosero VM, Kiss S, Terebessy T, et al. Dysplasia epiphysealis hemimelica (Trevor's disease): 7 of our own cases and a review of the literature. Acta Orthop. 2007;78:856-61. 6. Carlson DH, Wilkinson RH. Variability of unilateral epiphyseal dysplasia (dysplasia epiphysealis hemimelica). Radiology. 1979;133:369-73. 7. Vogel T, Skuban T, Kirchhoff C, et al. Dysplasia epiphysealis hemimelica of the distal ulna: a case report and review of the literature. Eur J Med Res. 2009;14:272-6. 8. Iwasawa T, Aida N, Kobayashi N, et al. MRI findings of dysplasia epiphysealis hemimelica. Pediatr Radiol. 1996;26:65-7. 1. Master of Health and Behavior, Professor of Pediatrics, Universidade Católica de Pelotas (UCPel), MD, Pediatric Physician at Hospital Universitário São Francisco de Paula, Pelotas, RS, Brazil. 2. Graduate Students of Medicine, School of Medicine, Universidade Católica de Pelotas (UCPel), Pelotas, RS, Brazil. 3. MD, Pediatric Physician, Hospital Universitário São Francisco de Paula, Pelotas, RS, Brazil. 4. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist, Hospital Universitário São Francisco de Paula and Hospital Santa Casa de Misericórdia de Pelotas, Pelotas, RS, Brazil. Mailing Address: Felipe Augusto Rozales Lopes Rua Emílio Jorge dos Reis, 512, Bairro Três Vendas Pelotas, RS, Brazil, 96020-440 E-mail: felipearlopes@gmail.com Received March 30, 2012. Accepted after revision August 20, 2012. * Study developed at Hospital Universitário São Francisco de Paula, Pelotas, RS, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554