A 47-year-old female patient was admitted to the emergency department presenting abdominal discomfort for ten days, with stitch pain in the epigastric region. The patient reported worsening with fever over the last three days. No history of previous disease was reported. Laboratory tests demonstrated leukocytosis with no deviation. Considering the intensity of the epigastric pain, the patient was referred for endoscopy which demonstrated the presence of an elevated lesion in the antrum, measuring approximately 1 cm, and umbilication covered by fibrin. Biopsy was performed.
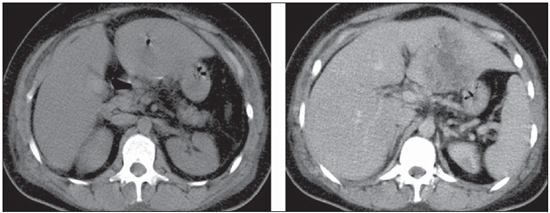
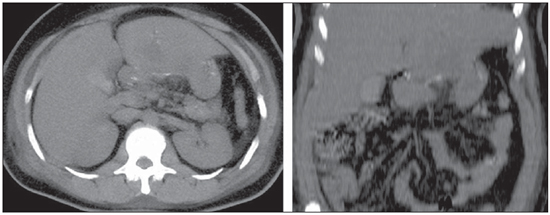
The patient progressed with worsening of the pain, remaining febrile but with no sign of peritonitis. Abdominal non-contrastenhanced and contrast-enhanced computed tomography was performed (Figures 1 and 2).
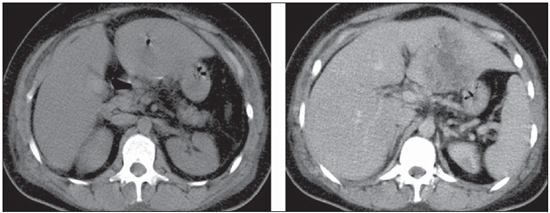
Figure 1. Abdominal computed tomography before and after intravenous contrast injection.
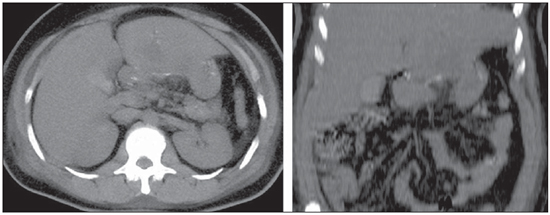
Figure 2. MIP reconstruction, non-contrast-enhanced, fine axial and coronal views.
Figure 1. A: Predominantly hypodense, expansile, loculated mass with anfractuous contours, measuring 8.1 cm x 6.2 cm, presenting peripheral, heterogeneous contrast enhancement, located in the left hepatic lobe (segments II and III). The presence of intermingled gas bubbles is observed.
B: A hyperdense linear image is observed in close contact with the left hepatic lobe. Such image remained unaltered along all the study phases.
Figure 2. Axial and coronal MIP reconstructions at non-contrast-enhanced phases, demonstrating the presence of a hyperdense linear image in close contact with the left hepatic lobe. Observe the small gastric curve in close contact with the left hepatic lobe.
Diagnosis: Pyogenic liver abscess caused by a foreign body which perforated the small gastric curvature.
COMMENTS
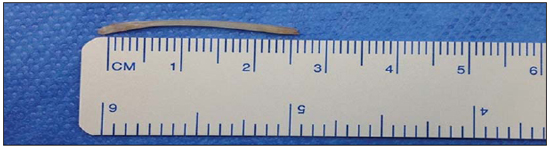
Liver abscess caused foreign body is a relatively rare condition of difficult diagnosis(1) and was firstly described in 1898 2,3. The greatest majority of cases are caused by tooth-picks, fish-spine (Figure 3) and dental prostheses(1,3,4). The degree of suspicion by health professionals is limited, since the symptoms are varied and nonspecific. Moreover, most of patients do not promptly report the foreign body ingestion(1,2).
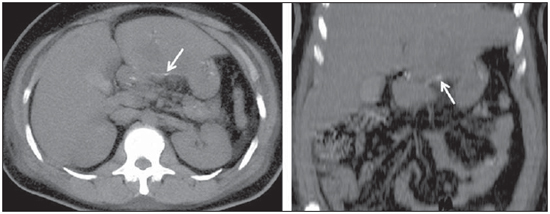
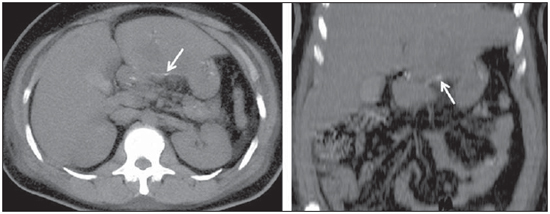
Figure 3. Axial and coronal MIP reconstructions in the non-contrast-enhanced phase, identifying a hyperintense linear mass (arrow) representing the foreign body.
Most ingested foreign bodies (Figure 4) pass through the gastrointestinal tract asymptomatically in a seven-day time span (3). In cases of development of a liver abscess, the site of penetration into the gastrointestinal tract cannot always be identified, but normally it results from perforation of the stomach, duodenum or transverse colon, with tamponade of the liver parenchyma or direct penetration of the foreign body(1). Usually, the foreign body lodges in the left liver lobe(1,2), which leads to increased diagnostic suspicion as an abscess is identified in this region.
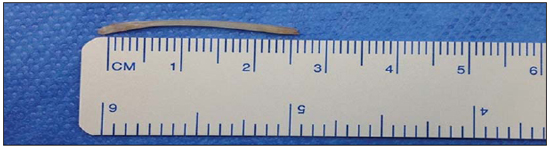
Figure 4. Foreign body - fish spine - removed by laparoscopy. In this case, the foreign body had totally migrated and was found posteriorly to the gastric serosa and perforating the left liver lobe, which has made the diagnosis by endoscopy more difficult.
Imaging methods, particularly computed tomography, present excellent sensitivity in the characterization of abscesses, besides allowing the identification of the foreign body, like in the present case(1,5). The lesion is typically round-shaped, with well defined walls, and may be either solitary or multiple. The variation in density depends on the necrosis intensity and the phase of the pathological process(5). The treatment comprises antibiotic therapy, abscess drainage and foreign body removal.
FINAL CONSIDERATIONS
Liver abscesses caused by foreign body generally lead to death because of late diagnosis in most of cases(5). Other etiologies should be sought in the absence of response to aspiration or drainage and antibiotic therapy. Despite the rarity of such an event, the presence of a foreign body must be taken into consideration, with an active search for radiographic/tomographic signs to identify the object and aid in the therapeutic surgery(2).
REFERENCES
1. Liu HJ, Liang CH, Huang B, et al. Migration of a swallowed toothpick into the liver: the value of multiplanar CT. Br J Radiol. 2009;82:e79-81.
2. Borba CC, Gomes ARS, Filgueira JPPS, et al. Abscessos hepáticos secundários a espinha de peixe. Relato de caso. Rev Bras Clin Med. 2012;10:83-6.
3. Santos SA, Alberto SCF, Cruz E, et al. Hepatic abscess induced by foreing body: case report and literature review. World J Gastroenterol. 2007;13:1466-70.
4. Waisberg J, Aráuz SNZ, Altieri LG. Abscesso hepático piogênico por corpo estranho. Rev Col Bras Cir. 2002;29:240-1.
5. Silva RF, Junior PCA, Duca WJ, et al. Abscesso hepático por osso de peixe. Arq Ciênc Saúde. 2006;13:61-3.
1. Physician, 3rd year Trainee at Unidade de Radiologia Clínica (URC), São José dos Campos, SP, Brazil.
2. MDs, Radiologists, Unidade de Radiologia Clínica (URC), São José dos Campos, SP, Brazil.
3. Master, MD, General Surgeon and Coloproctologist, Hospital Vivalle, São José dos Campos, SP, Brazil.
4. Associate Professor, Faculdade de Ciências Médicas da Santa Casa de São Paulo, Head of the Group of Liver Surgery, Santa Casa de São Paulo, São Paulo, SP, Brazil.
5. PhD, Professor, Department of Radiology, Faculdade de Medicina da Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil.
Mailing Address:
Dr. Marcelo Souto Nacif
Rua Barão de Cocais, 324, Bosque Imperial
São José dos Campos, SP, Brazil, 12242-042
msnacif@huap.uff.br / www.msnacif.med.br
Study developed at the Unidade de Radiologia Clínica (URC) and at Hospital Vivalle, São José dos Campos, SP, Brazil.
 Vol. 46 nº 1 - Jan. /Feb. of 2013
Vol. 46 nº 1 - Jan. /Feb. of 2013