INTRODUCTION
Acute abdomen is defined as a condition characterized by refractory and persistent pain leading the patient to seek medical emergency care(1). It is believed that up to 25% of cases with low abdominal pain admitted to emergency units are caused by acute pelvic inflammatory disease (APID)(1), which is the most common cause of acute pelvic pain among female patients(2).
Probably, the actual APID prevalence is underestimated, but there is a consensus that an increase has been observed over the last years, probably because of the higher frequency of diagnoses and changes in women's habits in the last decades(3).
Such prevalence rate has presented a significant increase in lower age ranges, proportionally inverse to the patients' age, and principally between the ages of 20 and 24(3).
APID includes a range of abnormalities affecting the uterine tubes, including salpingitis, pyosalpinx and tubo-ovarian abscess, as a result from ascending infection produced by germs from the vagina and uterine cervix, most commonly
Neisseria gonorrheae and
Chlamydia trachomatis which have been isolated in 12.2% of cases(3). In most cases, polymicrobial infection is observed, with isolation of endogenous agents such as anaerobic organisms and facultative bacteria, or even components of the vaginal microflora associated with bacterial vaginosis(3).
Main risk factors involved in the development of APID include having multiple sexual partners, high frequency of sex intercourse, young women and use of intrauterine devices. Imaging methods, particularly ultrasonography (US) have played a fundamental role in the APID diagnosis(1). Most recently, with the dissemination and wider availability of computed tomography (CT) and magnetic resonance imaging (MRI), such tools have been utilized as a supplement to US, most frequently in dubious or complicated cases(2).
In the present study, the authors present a pictorial essay based on a review of CT and MRI images acquired from a patient with proved APID in the period between January/2010 and December/2011, which were consensually interpreted by two radiologists.
CLINICAL AND LABORATORY FINDINGS
Acute pelvic inflammatory disease is frequently characterized by low abdominal pain, cervical motion and adnexal tenderness, either with or without association with fever(3). Associated clinical and laboratory findings present positive predictive values as low as 65% to 90%, even in the hands of more experienced gynecologists(3). Thus, many times the condition may be confused with acute appendicitis; and the presence of vaginal mucopurulent discharge in association with findings at digital examination is useful to guide the diagnosis(3).
Main laboratory findings include leukocytosis - a nonspecific finding with high levels in only 44% of patients -, and presence of inflammatory markers such as high C-reactive protein levels which, by its turn presents a good sensitivity (74% to 93%), but low specificity (25% to 90%)(3). Recently, vaginal smears were analyzed and showed high sensitivity (87% to 91%), as well as high negative predictive values for absence of upper genital tract infection (94.5%)(3).
It is important to establish a correlation with Β-hCG levels in order to rule out the diagnosis of ectopic pregnancy, even in cases where the patient reports a recent bleeding(4).
IMAGING FINDINGS
CT and MRI may be useful in cases of nonspecific clinical signs, inconclusive US, or in the suspicion of complications.
The findings differ from each other, depending on the degree of involvement and within the spectrum of presentations of this entity that may be classified as follows:
Salpingitis
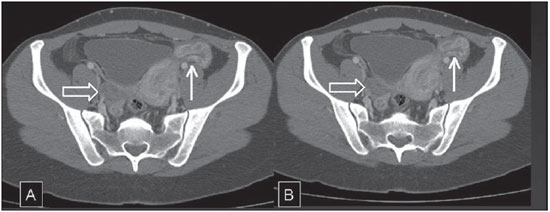
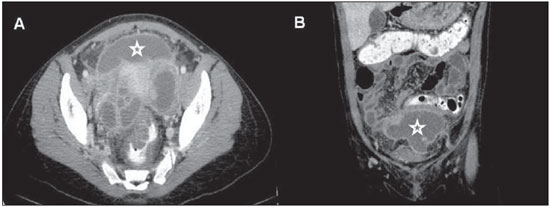
It is characterized by the absence of tubal dilatation, but with presence of thickening and contrast-enhancement of tubal walls in association with inflammatory signs of adjacent structures. Such signs are seen at CT as densification of adnexal fat planes, free fluid in the pelvic cavity, as well as reactional thickening of adjacent intestinal loops(5) (Figure 1).
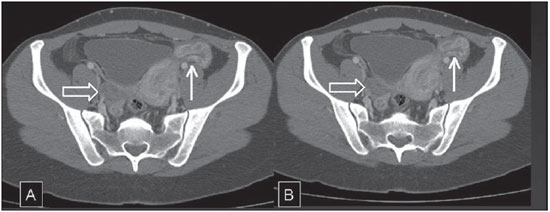
Figure 1. APID (salpingitis) - pelvic CT. Anomalous and increased enhancement is observed in the left adnexal region with a serpiginous appearance corresponding to the thickened and inflamed tubal wall (bold arrows). Also, a minimal amount of fluid is observed around the Fallopian tube. The right ovary presents a normal appearance (open arrows). (A, B: axial sections in the venous phase following contrast agent injection).
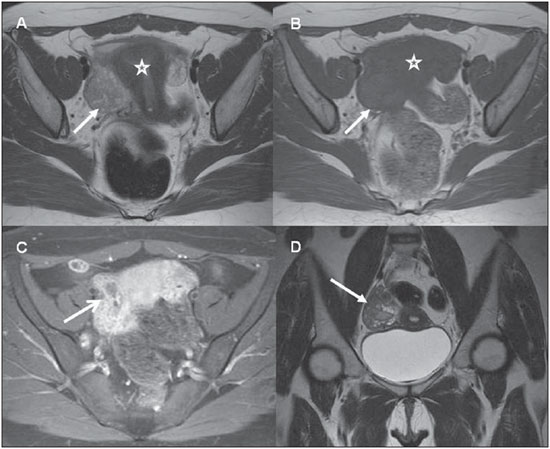
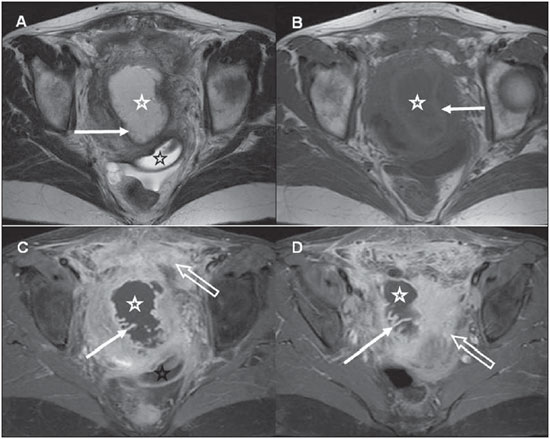
Similar findings are observed at MRI, and, because of its better spatial definition of pelvic structures, it is possible to define the parietal thickening and enhancement with greater detail(6) (Figure 2).
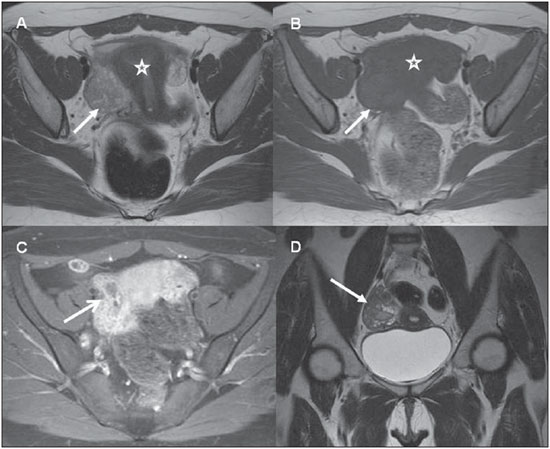
Figure 2. APID (salpingitis). Pelvic MRI. Presence of serpiginous mass in the right adnexal region (arrows on A, B and D), clearly separated from the uterus (stars on A and B), with intense parietal contrast-enhancement, characterizing its inflammatory nature (arrow on C). The finding on C is quite suggestive of thickened Fallopian tube wall. (A, B: axial T1- and T2-weighted images, respectively; C: axial, post-contrast injection Tl-weighted-image with fat saturation; D: coronal T2-weighted image).
At MRI, the tubal structure is identified by high signal intensity on T2-weighted sequences, without internal enhancement. On T1-weighted sequences, the signal intensity is variable, depending on the hemorrhagic and protein content of the mass. Parietal enhancement is observed on post-contrast sequences, with increase and densification of adjacent fat planes(5) (Figure 3).
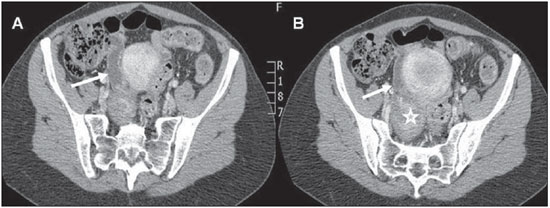
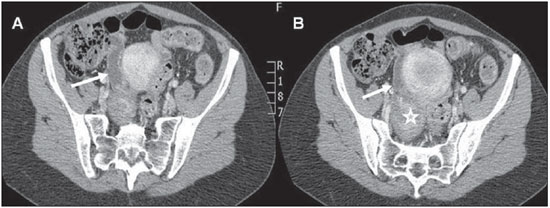
Figure 3. Tubo-ovarian abscess - Abdominal CT. A nodular mass with heterogeneous enhancement is observed in the right adnexal region, representing the ovary affected by infectious process (star on B). The Fallopian tube is dilated and with parietal enhancement, indicating salpingitis or pyosalpingix (arrows on A and B). (A, B: axial sections acquired in the portal phase following contrast injection).
Some differential diagnoses must be considered. Differently from pyosalpinx, in hydrosalpinx, contrast-enhancement of tubal walls does not occur. Other diagnoses, such as appendicitis and complex adnexal masses may complicate the differential diagnosis(5).
Tubo-ovarian abscess
It occurs through the progression of the infectious process, with compromise of healthy pelvic structures and development of an inflammatory mass involving the Fallopian tube and the ovary. The rupture of such mass might result in severe peritonitis with potential risk for death(7).
Tomographic findings include solidcystic adnexal mass, parietal enhancement, and gross septa demonstrating contrast-enhancement(7).
The presence of gas in the inflammatory/infectious process is not frequently observed, but represents a quite specific finding(7) (Figure 4).
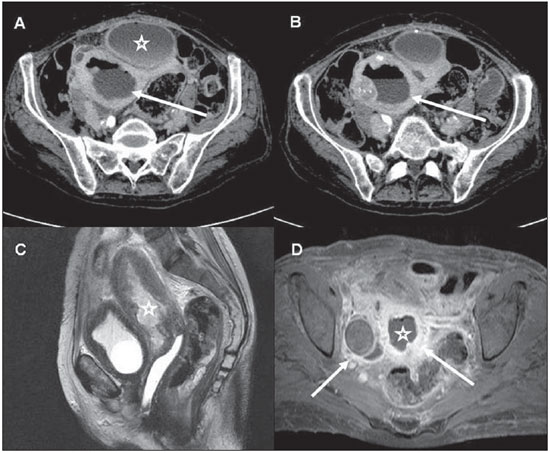
Figure 4. Severe APID - Abdominal/Pelvic CT (A, B) and Pelvic MRI (C, D). Extensive, diffuse endometrial thickening and presence of air-fluid level in the uterine cavity (arrows on A and B). Additionally, a heterogeneous collection is observed anteriorly to the uterus, with thickened walls and demonstrating moderate contrast-enhancement (star on A). The same patient underwent pelvic MRI that demonstrated the presence of thickened material in the uterine cavity (stars on C and D), as well as enhancement of adnexal structures (arrows on D). (A, B: axial sections acquires in the portal phase following contrast injection; C: sagittal MRI, T2-weighted image; D: axial MRI, post-contrast Tl-weighted image with fat saturation).
The anterior displacement of the broad ligament of the uterus caused by the posterior positioning of the mesovarium, observed at CT or MRI, may allow the differentiation between tubo-ovarian abscess and pelvic abscess of other origins(8).
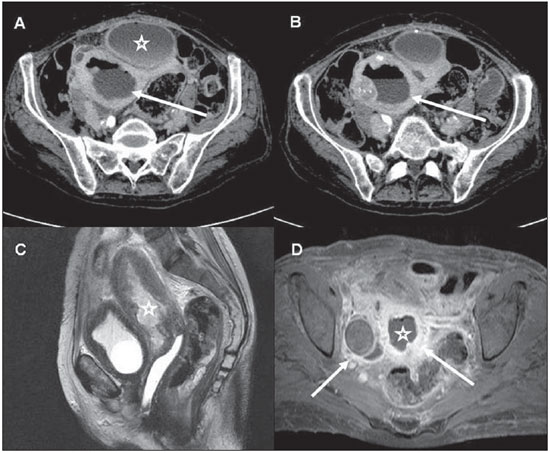
Commonly found associated signs include, principally, enhancement of the peritoneum and uterine ligaments. Additionally, involvement of adjacent structures such as the ileum, hydroureteronephrosis, and intraperitoneal abscess secondary to rupture may occur(5) (Figure 5).
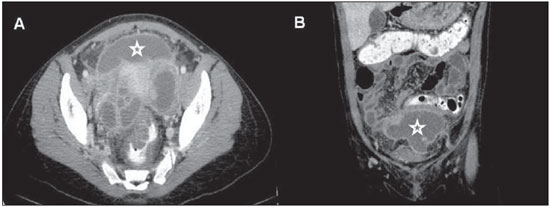
Figure 5. APID - Abdominal and Pelvic CT. Extensive, multiloculated collection with thick walls demonstrating intense enhancement, located in the pelvic cavity (stars on A and B). Also, twisted cystic masses are observed in adnexal fossas corresponding to dilated and fluid-filled Fallopian tubes. (A: axial section acquired in the portal phase following contrast injection; B: coronal reconstruction, also in the portal phase).
MRI findings depend on the hemorrhagic and protein content of the mass, presenting variable signal intensity on T1- weighted sequences, depending on the amount of such components(9,10). The presence of a hyperintense rim along the inner wall of the collection has been recently described and attributed to the presence of granulation tissue(5).
T2-weighted imaging demonstrates high signal intensity, with multiple, gross septa with low signal intensity, as well as high signal intensity on the peritoneal fat at T2- weighted sequences with fat saturation, corresponding to edema(5). Such septa, together with the collection capsule, demonstrate intense contrast-enhancement in association with enhancement of the involved fat and abdominal structures(5) (Figure 6).
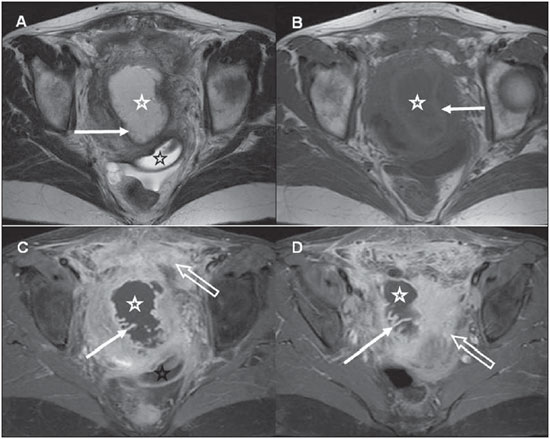
Figure 6. Tubo-ovarian abscess - Pelvic MRI. Large, adnexal, heterogeneous collection (white stars on A to D) with thickened walls with contrast enhancement and internal thin folds (bold arrows on A, C and D) compatible with dilated Fallopian tube. The wall of the mass presents high signal intensity at T1-weighted images (bold arrow on B) compatible with small foci of parietal hemorrhage. Also a loculated fluid collection is observed in the posterior cul-de-sac (black stars on A and C) and intense enhancement of the peritoneum in the pelvic cavity (open arrows on C and D). (A, B: axial T2- and Tl-weighted images, respectively; C, D: axial post-contrast T1-weighted image with fat saturation).
A meshlike stranding is frequently observed in the peritoneal fat adjacent to the process and is related to adhesions and fibrosis(5).
CONCLUSION
Acute pelvic inflammatory disease is a common condition among women and one of the main causes of inflammatory acute abdomen. Frequently, the diagnosis of such condition is confirmed by US. Most recently, CT and MRI have been adopted as supplementary diagnostic tools, as a result of the frequent complications associated with the condition which pose difficulties for an accurate noninvasive evaluation. In the present study, the authors have sought to illustrate the main, still poorly known CT and MRI findings of APID. Thus, the increasing role played by CT and MRI in the assessment of patients with acute abdomen, particularly those cases of gynecologic origin, requires radiologists' familiarization with imaging findings of APID, supplementing the utilization of US.
REFERENCES
1. Samraj GP, Curry RW Jr. Acute pelvic pain: evaluation and management. Compr Ther. 2004;30:173-84.
2. Bennett GL, Slywotzky CM, Giovanniello G. Gynecologic causes of acute pelvic pain: spectrum of CT findings. Radiographics. 2002;22:785-801.
3. Lareau SM, Beigi RH. Pelvic inflammatory disease and tubo-ovarian abscess. Infect Dis Clin North Am. 2008;22:693-708.
4. Potter AW, Chandrasekhar CA. US and CT evaluation of acute pelvic pain of gynecologic origin in nonpregnant premenopausal patients. Radiographics. 2008;28:1645-59.
5. Rezvani M, Shaaban AM. Fallopian tube disease in the nonpregnant patient. Radiographics. 2011;31:527-48.
6. Heverhagen JT, Klose KJ. MR imaging for acute lower abdominal and pelvic pain. Radiographics. 2009;29:1781-96.
7. Birnbaum BA, Jeffrey RB Jr. CT and sonographic evaluation of acute right lower quadrant abdominal pain. AJR Am J Roentgenol. 1998;170:361-71.
8. Wilbur AC, Aizenstein RI, Napp TE. CT findings in tuboovarian abscess. AJR Am J Roentgenol. 1992;158:575-9.
9. Tukeva TA, Aronen HJ, Karjalainen PT, et al. MR imaging in pelvic inflammatory disease: comparison with laparoscopy and US. Radiology. 1999;210:209-16.
10. Horrow MM. Ultrasound of pelvic inflammatory disease. Ultrasound Q. 2004;20:171-9.
1. Radiologist, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
2. Radiologist, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
3. Associate Professor, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP Brazil.
Mailing Address:
Dr. Giuseppe D'Ippolito
Departamento de Diagnóstico por Imagem - EPM-Unifesp
Rua Napoleão de Barros, 800, Vila Clementino
São Paulo, SP Brazil, 04024-002
E-mail: giuseppe_dr@uol.com.br
Received February 13, 2012.
Accepted after revision June 28, 2012.
* Study developed in the Department of Imaging Diagnosis at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP Brazil.
 Vol. 45 nº 6 - Nov. / Dec. of 2012
Vol. 45 nº 6 - Nov. / Dec. of 2012