Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012
|
CASE REPORT
|
|
Congenital ranula: antenatal sonographic diagnosis* |
|
|
Autho(rs): Livia Teresa Moreira Rios1; Edward Araujo Júnior2; Luciano Marcondes Machado Nardozza3; Antonio Fernandes Moron4; Marília da Glória Martins5 |
|
|
Keywords: Prenatal diagnosis; Ultrasound; Oral tumor; Ranula. |
|
|
Abstract: INTRODUCTION
Congenital ranula is a rare tumor located on the mouth floor which raises the tongue. It may be caused either by a mucus extravasation cyst secondary to obstruction and rupture of sublingual or minor salivary glands, or, less commonly, to a mucus retention cyst originating from dilatation of an obstructed submandibular gland duct, and therefore surrounded by epithelium(1,2). Congenital mucus extravasation cyst or mucoceles is a pseudocyst usually located in the sublingual space between the mylohyoid muscle and the lingual mucosa, with estimated prevalence of 0.74%(3). Few cases of prenatal diagnosis have been reported in the literature. The authors report the case of a congenital ranula, antenatally diagnosed by ultrasonography, emphasizing possible differential diagnoses. CASE REPORT A 24-year-old, G3P2 woman, with gestational age around 29 weeks, was referred to the Unit of Ultrasonography, Service of Gynecology and Obstetrics, Universidade Federal do Maranhão (UFMA), because of polihydramnios and a large oral cavity mass of cystic nature. Both personal and family history with no relevant data. Obstetric ultrasonography was performed and revealed the presence of a large, anechoic, homogeneous cystic mass measuring 5.0 cm in diameter, with thin and smooth 2.8 cm thick walls (Figures 1 and 2). Vascularization was not observed at color Doppler ultrasonography. Fetal screening did not reveal any other associated malformation.  Figure 1. Lateral view of fetal face demonstrating a large anechoic, homogeneous collection with thin and regular walls, impairing the fetal deglutition. 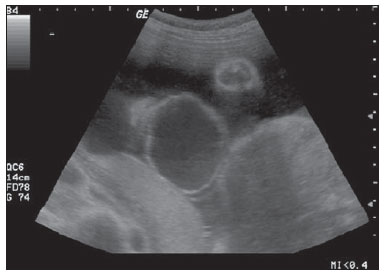 Figure 2. Coronal section of fetal face revealing normality of the nose and upper lip, and highlighting the increased diameter of the cystic mass. Increased amniotic fluid volume was observed. The largest pocket measured 112 mm, and the amniotic fluid index (AFI) was 317 mm (normal between 92 and 231 mm for gestational age, according to the table proposed by Moore & Cayle(4)). At the 30th gestational week, preterm premature rupture of ovular membranes was diagnosed and the woman entered premature labor. Cesarean section was performed, and macroscopic examination confirmed the previous findings. Decompression was performed by means of percutaneous aspiration of the cystic collection. The neonate died some hours after birth because of respiratory complications. DISCUSSION In the last years, ultrasonography has been widely utilized by all obstetrics reference centers. Amongst the recent advances in imaging diagnosis, 3D ultrasonography (3DUS) is utilized with amplitude Doppler to assess the fetal brain vascularization(5) or the fetal limbs volume(6). Ranula is most commonly found in children and young adults, and rarely occurs in neonates. This entity may be classified according its location, as follows: simple ranula - located on the floor of the mouth; cervical ranula - located in the paracervical region; and plunging ranula - located near to the upper airways, resulting from rupture of a simple ranula. Few cases of antenatal detection of ranulas have been reported in the literature(2). Solid and cystic exophytic masses should be considered in the differential diagnosis, as well as lymphatic malformations, epignatus (oropharyngeal teratoma) and other cystic lesions of the mouth(2,7). Lymphatic malformations (vascular hamartomas and lymphangiomas) are solid-cystic lesions with indistinct and irregular margins, which are observed from the birth and continue to grow with the development of the patient(2,7,8). Oropharyngeal teratoma or epignatus is an uncommon, solid tumor that is seen as hypo- and hyperechogenic areas, affecting between 1:35000 and 1:200000 living neonates, with high morbidity and mortality rates(2,9,10). Cystic lesions considered in the differential diagnosis for congenital ranula include gingival and palatal cysts, whose resolution occurs spontaneously(2) and, more rarely, thyroglossal duct cysts typically located on the buccal floor, duplication cysts and cysts with heterotopic gastric mucosa(7). In such cases, magnetic resonance imaging (MRI) could be useful in the differential diagnosis. Tamaru et al.(11) have described a case of ranula diagnosed at the 36th gestational week, where MRI identified a small lesion in the midline of the mouth, in the sublingual space, below the mylohyoid muscle, where a T2-weighted sequence clearly defined the presence of a homogeneous mass. Other described prenatal diagnostic method is 3DUS, which can play a role as adjuvant to 2D ultrasonography, allowing a spatial evaluation of the relation between the mass and the oral cavity of the fetus(12). In the present case, the diagnosis of the cystic lesion was facilitated by the findings of homogeneity, thin and regular walls at ultrasonography, and avascular mass at color Doppler, besides the aspirated mucous content. A correct antenatal diagnosis becomes extremely relevant because generally such neonates present varied degrees of airways obstruction, requiring the presence of a multidisciplinary team including obstetricians, neonatologists and head & neck surgeons at the moment of the birth. Such a multidisciplinary team is required to avoid respiratory failure, and many times it is necessary to perform extrauterine intrapartum treatment - a procedure carried out during the Cesarean section, with preservation of the fetal-placental circulation, which allows a safe handling of the conceptus' airways, reducing the risk of airways obstruction. In summary, the authors describe a case of antenatal diagnosis of ranula. The correct diagnosis is essential to allow a prenatal follow-up in a reference center, besides the planning of the delivery with a multidisciplinary team. REFERENCES 1. Galloway RH, Gross PD, Thompson SH, et al. Pathogenesis and treatment of ranula: report of three cases. J Oral Maxillofac Surg. 1989;47:299-302. 2. Onderoglu L, Saygan-Karamürsel B, Deren O, et al. Prenatal diagnosis of ranula at 21 weeks of gestation. Ultrasound Obstet Gynecol. 2003;22:399-401. 3. Jorgenson RJ, Shapiro SD, Salinas CF, et al. Intraoral findings and anomalies and neonates. Pediatrics. 1982;69:577-82. 4. Moore TR, Cayle JE. The amniotic fluid index in normal human pregnancy. Am J Obstet Gynecol. 1990;162:1168-73. 5. Moron AF, Milani HJ, Barreto EQ, et al. Análise da reprodutibilidade do Doppler de amplitude tridimensional na avaliação da circulação do cérebro fetal. Radiol Bras. 2010;43:369-74. 6. Cavalcante RO, Araujo Júnior E, Nardozza LM, et al. Reprodutibilidade do volume de membros fetais pela ultrassonografia tridimensional utilizando o método XI VOCAL. Radiol Bras. 2010;43:219-23. 7. Fernandez Moya JM, Cifuentes Sulzberger S, Díaz Recaséns J, et al. Antenatal diagnosis and management of a ranula. Ultrasound Obstet Gynecol. 1998;11:147-8. 8. Rousseau T, Couvreur S, Senet-Lacombe E, et al. Prenatal diagnosis of enteric duplication cyst of the tongue. Prenat Diagn. 2004;24:98-100. 9. Martinelli P, Paladini D, Nicotra A, et al. In utero diagnosis of oropharyngeal teratoma: a case report. Eur J Obstet Gynecol Reprod Biol. 1990;35:291-4. 10. Levine AB, Alvarez M, Wedgwood J, et al. Contemporary management of a potentially lethal fetal anomaly: a successful perinatal approach to epignathus. Obstet Gynecol. 1990;76:962-6. 11. Tamaru S, Kikuchi A, Ono K, et al. Prenatal ultrasound and magnetic resonance imaging depiction of a small sublingual ranula. J Clin Ultrasound. 2010;38:147-50. 12. Pires P, Pereira M, Machado L, et al. Prenatal diagnosis of a ranula with 2- and 3-dimensional sonography and sonographically guided aspiration. J Ultrasound Med. 2006;25:1499-502. 1. Master, MD, Unit of Ultrasonography, Service of Gynecology and Obstetrics, Universidade Federal do Maranhão (UFMA), São Luís, MA, Brazil. 2. PhD, Associate Professor, Division of Fetal Medicine, Department of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 3. Private Docent, Associate Professor, Division of Fetal Medicine, Division of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 4. Private Docent, Chair of the Department of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 5. PhD, Associate Professor, Service of Gynecology and Obstetrics, Universidade Federal do Maranhão (UFMA), São Luís, MA, Brazil. Mailing Address: Dr. Edward Araujo Júnior Rua Carlos Weber, 956, ap. 113, Visage, Vila Leopoldina São Paulo, SP, Brazil, 05303-000 E-mail: araujojred@terra.com.br Received March 17, 2012. Accepted after revision July 20, 2012. * Study developed at the Service of Gynecology and Obstetrics of Hospital Universitário da Universidade Federal do Maranhão (UFMA), São Luís, MA, and at Department of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPMUnifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554