INTRODUCTION
Metastatic calcification is the deposition of calcium salts in previously healthy tissues. The pulmonary parenchyma is most susceptible to calcification, and the resulting change is called metastatic pulmonary calcification (MPC). Such condition may be caused by both benign and malignant diseases, most commonly occurring in patients submitted to hemodialysis for chronic renal failure (CRF)(1,2). In autopsies, 60-80% of patients with CRF reportedly present MPC(3).
The respiratory symptoms in MPC are variable and, generally, the degree of respiratory discomfort is proportional to the amount of macroscopic calcification. Extensive pulmonary calcification may be asymptomatic, while subtle calcification with normal chest radiography may pose severe respiratory compromise(4).
Chest radiography may present as normal or with poorly defined and/or confluent nodular opacities mimicking alveolar filling disorders. The characterization of MPC is better defined at computed tomography(5,6). The most common parenchymal finding at high-resolution computed tomography (HRCT) is the presence of poorly defined centrilobular nodules with groundglass opacity, measuring approximately 3 to 10 mm in diameter. In spite of the histologically interstitial nature of the infiltrate, the HRCT findings may mimic nodular air space filling disease(7,8).
We report on the case of a female patient with CRF, under hemodialysis for 13 years, whose chest HRCT demonstrated groundglass opacities associated with poorly defined centrilobular nodules with groundglass attenuation, with no finding of parenchymal calcification on soft tissue window. Such findings might mimic air space disease, requiring histopathological study for diagnostic conclusion.
CASE REPORT
A 48-year-old, female patient undergoing hemodialysis for 13 years because of acute-on-chronic renal failure secondary to renal tuberculosis in her childhood, with onset of hemoptysis, fever, effort dyspnea and productive cough. Physical examination of the respiratory system revealed sparse and diffuse wheezes and stertors. Laboratory tests demonstrated the following results: red blood cells - hemoglobin, 11.7 g/dl and hematocrit, 35.3%; white blood cells - 7100 leukocytes (neutrophils, 60%; segmented neutrophils, 1%; lymphocytes, 20%; monocytes, 12%; eosinophils, 7%). Serum biochemistry revealed urea at 155 mg/dl (normal: 15 to 40 mg/dl), creatinine at 9.24 mg/dl (normal: 0.6 to 1.3 mg/ dl), alkaline phosphatase at 90 U/L (normal: 20 to 105 U/L), LDH at 402 U/L (normal: 95 to 225 U/L), total calcium at 8.9 mg/dl (normal: 8.5 to 10.5mg/dl), phosphorus at 6.2 mg/dl (normal: 2.5 to 4.5 mg/dl) and C-reactive protein at 1.76 mg/dl (normal: lower than 0.8 mg/dl).
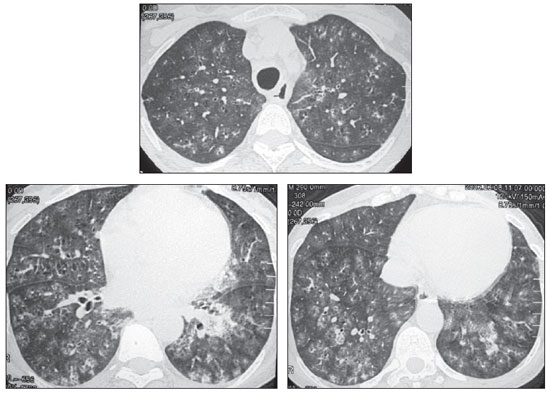
Chest radiography revealed bilateral condensation predominating in the middle and lower thirds. Chest HRCT presented ground-glass opacities associated with poorly defined centrilobular nodules with ground-glass attenuation (Figure 1). Neither parenchymal nor vascular calcifications were identified on sections with mediastinal window. At bronchoscopy, the bronchoalveolar lavage revealed 63% of macrophages, 16% of lymphocytes (49% mononuclear), 2% of monocytes, 2% of eosinophils and 17% of segmented neutrophils. Numerous vacuolated macrophages and hemorrhagic aspect were observed. Culture did not demonstrate microorganism growth. Respiratory function tests were not performed. Open biopsy revealed pulmonary tissue with exuberant alveolar hemosiderosis associated with microcalcifications located in alveolar septa and vascular walls, compatible with MPC. Some months after diagnosis, the patient presented worsening of dyspnea and hemoptysis, progressing to acute respiratory failure and death.
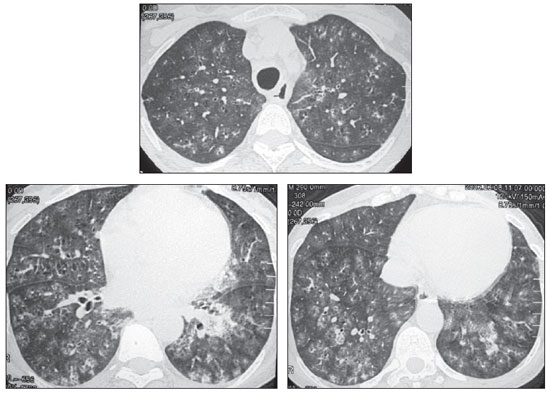
Figure 1. High resolution computed tomography of chest, with sections at three different levels with lung window, demonstrating the presence of multiple ill defined centrilobular nodules and ground-glass attenuation.
Ectopic pulmonary calcification is divided into two groups, according to the physiopathological mechanism, as follows: dystrophic calcification - deposition of calcium salts in previously injured tissues, and metastatic calcification - deposition of calcium salts in previously healthy tissues(1,2,7). Other organs such as stomach, kidneys and heart can also be affected by calcification; but the pulmonary parenchyma is the most susceptible tissue. The pulmonary calcification mechanism, either with or without ossification, still remains to be completely understood. Metastatic calcification may be influenced by increased serum calcium and phosphate concentrations, alkaline phosphatase activity and local physicochemical conditions such as pH(1).
MPC may be caused by both benign and malignant conditions. Among the benign conditions, the following can be mentioned: primary hyperparathyroidism, hypervitaminosis D, Paget's disease and osteopetrosis. Malignant causes include multiple myeloma, lymphoma/leukemia, and choriocarcinoma, among others. However, MPC occurs most notably in patients undergoing hemodialysis for CRF. Dystrophic calcification occurs secondarily to caseation necrosis or fibrosis and may also be secondary to pulmonary infections, including granulomatous, viral and parasitic infections(1).
In those patients undergoing hemodialysis, four conditions predispose to metastatic calcification. The first one is acidosis, which "dissolves" the bones calcium phosphate salts. The second condition involves increased secretion of parathormone caused by negative balance of serum calcium due to kidneys failure in converting 25-hydroxyvitamin D into vitamin D 1.25, resulting in increased release of calcium and phosphate by bone tissue. Autonomous parathyroid glands function may occur, resulting in tertiary hyperparathyroidism and severe hypercalcemia. In the third condition, the intermittent alkalosis caused by the bicarbonate utilized in dialysis predisposes to precipitation of calcium salts on soft tissues. The fourth condition is the decrease or absence of glomerular filtration, contributing to the increase in serum phosphate levels. High levels of serum phosphate have shown correlation with the presence of vascular calcification in uremic patients(9).
Most of the patients presenting with MPC are asymptomatic and, usually, respiratory function tests present normal results. However, restrictive pulmonary function, decreased diffusion capacity, hypoxemia and, occasionally, respiratory failure may occur.(7)
The MPC distribution pattern is variable, sometimes being diffuse, other times lobar or predominating in the apexes. It is a predominantly interstitial process. However, histopathological studies demonstrate sites of calcium deposition in alveolar septa and, to a lesser extent, in arterioles and bronchioles. At histopathology, sites of calcium deposition are located in the alveolar epithelial basement membranes, alveolar capillary walls, bronchial walls, and the media of pulmonary arterioles(1).
Chest radiography is rarely useful in the diagnosis of MPC. Radiography is not sensitive enough to detect small amounts of calcium, and as compared with autopsy, this imaging method demonstrates parenchymal calcification in less than 15% of the patients. Radiographic findings, when present, are nonspecific. The abnormalities include poorly defined nodules, interstitial infiltration and alveolar filling. Such findings may mimic other conditions such as pulmonary edema, hemorrhage, pneumonia, infarction and malignant disease. Additionally, there is no correlation between the degree of pulmonary involvement and clinical symptoms(10).
HRCT is the most efficient method for detecting MPC. Three most common parenchymal patterns are described, namely, diffuse or irregular opacities with groundglass attenuation, dense consolidation with frequent lobar distribution, and multiple nodules with diffuse or localized distribution. Such patterns are not mutually exclusive, and a combination of patterns can exist(1,10). The most common parenchymal HRCT finding is the presence of poorly defined centrilobular nodules with groundglass opacity, and measuring approximately 3-10 mm in diameter. Despite the histologically interstitial nature of the infiltrate, the HRCT finding may mimic nodular alveolar filling(7). Recently, magnetic resonance imaging findings were also described(11).
Finally, in cases of patients with a history of CRF, the hypothesis of MPC must be included in the differential diagnosis of diffuse parenchymal opacities.
REFERENCES
1. Chan ED, Morales DV, Welsh CH, et al. Calcium deposition with or without bone formation in the lung. Am J Respir Crit Care Med. 2002;165:1654-69.
2. Sanders C, Frank MS, Rostand SG, et al. Metastatic calcification of the heart and lungs in endstage renal disease: detection and quantification by dual-energy digital chest radiography. AJR Am J Roentgenol. 1987;149:881-7.
3. Conger JD, Hammond WS, Alfrey AC, et al. Pulmonary calcification in chronic dialysis patients. Clinical and pathologic studies. Ann Intern Med. 1975;83:330-6.
4. Brodeur FJ Jr, Kazerooni EA. Metastatic pulmonary calcification mimicking air-space disease. Technetium-99m-MDP SPECT imaging. Chest. 1994;106:620-2.
5. Hartman TE, Müller NL, Primack SL, et al. Metastatic pulmonary calcification in patients with hypercalcemia: findings on chest radiographs and CT scans. AJR Am J Roentgenol. 1994;162:799-802.
6. Marchiori E, Müller NL, Souza AS Jr, et al. Unusual manifestations of metastatic pulmonary calcification: high-resolution CT and pathological findings. J Thorac Imaging. 2005;20:66-70.
7. Kobayashi T, Satoh K, Nakano S, et al. A case of metastatic pulmonary calcification after transient acute renal failure. Radiat Med. 2005;23:435-8.
8. Marchiori E, Souza AS Jr, Franquet T, et al. Diffuse high-attenuation pulmonary abnormalities: a pattern-oriented diagnostic approach on highresolution CT. AJR Am J Roentgenol. 2005;184:273-82.
9. Giachelli CM, Jono S, Shioi A, et al. Vascular calcification and inorganic phosphate. Am J Kidney Dis. 2001;38(4 Suppl 1):S34-7.
10. Janssen WJ, Sippel JM. Persistent radiographic infiltrates in a patient with chronic cough. Chest. 2005;128:1878-9,1880-1.
11. Hochhegger B, Marchiori E, Souza AS Jr, et al. MRI and CT findings of metastatic pulmonary calcification. Br J Radiol. 2012;85:e69-72.
1. Nuclear Physician, Fellow degree in Radiology, Hospital Universitário Antonio Pedro (HUAP), Niterói, RJ, Brazil.
2. PhD, Associate Professor, Department of Radiology, School of Medicine, Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil.
3. Full Professor, Department of Radiology, Universidade Federal Fluminense (UFF), Niterói, RJ, Adjunct Coordinator of the Course of Post-graduation in Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil.
Mailing Address:
Dr. Edson Marchiori
Rua Thomaz Cameron, 438, Valparaíso
Petrópolis, RJ, Brasil, 25685-120
E-mail: edmarchiori@gmail.com
Received May 10, 2012.
Accepted after revision July 5, 2012.
* Study developed at Hospital Universitário Antonio Pedro (HUAP), Niterói, RJ, Brazil.
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012